Retained Wooden Intra-Lenticular Organic Foreign Body-Could it remains Asymptomatic and Sterile-?
S.K.Prabhakar1*, Raghavender Reddy A2, Oshin Middha3, Prashansa Yadav4
1 Faculty, Ophthalmology Department, JSS Academy of Higher education and research, JSS Medical College Hospital, Mysore-570004, Karnataka, India.
2 Consultant, Cataract and Cornea refractive services, Hyderabad, Andra Pradesh, India.
3 Junior Resident, Faculty, Ophthalmology Department, JSS Academy of Higher Education and Research, JSS Medical College Hospital, Mysore-570004 Karnataka India.
*Corresponding Author
S.K.Prabhakar,
Professor and Head, Department of Ophthalmology, JSS Hospital, Mysore-4, Karnataka, India.
Tel: +919880074529
Fax: 0821-2335556
E-mail: skprabhakar@jssuni.edu.in
Received: January 04, 2022; Accepted: February 17, 2022; Published: February 18, 2022
Citation: S.K.Prabhakar, Raghavender Reddy A, Oshin Middha, Prashansa Yadav. Retained Wooden Intra-Lenticular Organic Foreign Body-Could it remains Asymptomatic and Sterile-?. Int J Ophthalmol Eye Res. 2022;10(1):478-480 doi: dx.doi.org/10.19070/2332-290X-2200096.
Copyright: S.K.Prabhakar© 2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: To discuss possible factors responsible for ocular inertness without resulting in an inflammatory incitement is
the objective of this case study. A 35-year-old female patient presented with visual loss in the right eye following an accidental
stick injury at the workplace one year back. Previous medication history includes topical instillation of antibacterial and antifungal
agents with cycloplegics that resulted in relief of redness and eye pain. The patient noticed painless progressive visual
loss for the past year and is now reported to the outpatient ophthalmic department. The patient was diagnosed to have adherent
leucoma that obscured underlying traumatic cataract with the presence of light perception and accurate light projection.
Hyper reflective echoic reverberations noticed within the crystalline lens on B-scan ultrasonography suggesting a possible
presence of an intra-lenticular foreign body that the egression of the foreign body was confirmed during cataract extraction
particularly on performing hydro procedures and cortical cleanup. A provisional diagnosis of traumatic cataract with adherent
leucoma was considered and accordingly managed by performing penetrating keratoplasty, cataract extraction and sulcus
fixated intraocular lens implantation.
Previously controlled infection with antimicrobial topical administration, crystalline lens response of embedding foreign body
within opacified lens fibres, ocular, and systemic immunological response are some of the few plausible implications leading to
its inertness. Hence, we recommend a B scan investigation in all cases of traumatic cataracts and corneal opacities to diagnose
and to formulate action strategic plans for achieving good visual outcomes.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.Conclusion
7.References
Introduction
B-scan Ultrasonography; Intra Lenticular Foreign Body; Traumatic Cataract; Adherent Leucoma; Penetrating Keratoplasty; Triple Procedure; Inertness.
Introduction
Ocular defensive mechanisms that combat retained intraocular
foreign body (IOFB) reaction whether organic or non-organic,
largely depends on their chemical composition, sterility, duration
of stay. and location in addition to hosts tissue vascularity differentiation.
Asymptomatic and incidental diagnosis is the common
mode of presentation of intralenticular foreign bodies nevertheless
previous case studies revealed acute visual loss due to cataract
induced by a metallic foreign body.[1] A retrospective study
reported the incidence of intralenticular foreign bodies in 17
(6.94%) eyes out of 245 eyes.[2]. Inert and sterile foreign bodies
such as stone, sand, glass, porcelain, plastic, and cilia are generally
well tolerated and possibly resort to masterly inactive intervention
if their location is outside the visual axis.[3, 4]
Another retrospective study reported wood as an ILFB in one (4.8%) eye out of 21 eyes among all other types of foreign bodies.
[5] Common reactive metallic foreign bodies are zinc, aluminum,
copper, and iron that incite inflammation-causing glial and fibrovascular
proliferation in the vitreous cavity and the retina. The
occurrence of retinal detachment, infective endophthalmitis, and
phthisis bulbi complicates the process of further visual loss progression.
Consequently, especially copper and iron foreign bodies
are prone to their migration causing further tissue damage.
This is probably the second case report of vegetative foreign body
embedding and retaining in the crystalline lens for about one year
without inciting an inflammatory reaction and to describe the
possible resisting factors responsible for ocular unresponsiveness
is the objective of this case study.
Case Description
A 35-year-old female patient presented with diminished vision in
her right eye following a wooden stick injury while working in the
fields 12 months ago manifesting with pain, redness, and visual
reduction. Resolution of the symptoms observed on instilling
some topical antibiotics, anti-fungal, and cycloplegic agents for
about 10 days while the visual loss continues to progress, however
unfortunately the patient discontinued treatment and abstained
from hospital follow-ups. A central adherent leucoma measuring
about 6 mm in dimension, irregular anterior chamber depth,
presence of light perception, and an accurate projection of rays
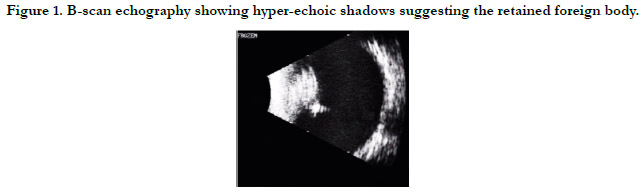
of light were noticed on cursory ocular examination. On B-Scan
echography, an attached retina was noted with an optically empty
vitreous cavity in addition to observing moderate to high hyperreflective
echoes that possibly arose in the crystalline lens suggesting
a retained intra-lenticular foreign body (RILFB). (Fig 1)
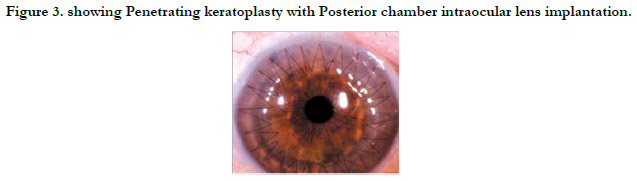
A triple procedure composed of penetrating keratoplasty, cataract
extraction, and intraocular lens implantation was considered taking
into account the contralateral biometric values for calculating
IOL power. After performing corneal trephination and releasing
the anterior synechiae and irido-lenticular adhesions, intracameral
adrenaline was instilled to achieve pupil dilation followed by capsular
staining with trypan blue.
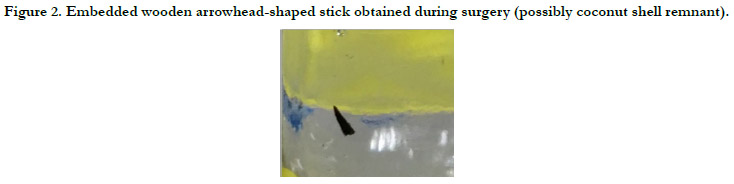
Can opener capsulotomy was performed and during hydro procedures
and cortical cleanup, egression of a brown triangular wooden
foreign body was observed and retrieved from the lenticular
substance. The surgical procedure was completed by implanting
a sulcus fixated IOL implantation after aspirating the corticonuclear
matter by irrigation and aspiration. (Fig 2) With Ethilon
10.0 suture material, penetrating keratoplasty was completed by
a continuous suturing pattern. And then air bubble was injected
for anterior chamber reformation. On the 7th post-operated day,
Snellen'svisual acuity was restored to 6/36 with stable intraocular
lens and anterior chamber maintenance. (Fig 3)
Figure 2. Embedded wooden arrowhead-shaped stick obtained during surgery (possibly coconut shell remnant).
Results and Discussion
Retained intraocular foreign bodies, whether metallic or vegetative
predispose to significant visual loss due to their predispositions
to endophthalmitis, retinal detachment, and in long-run
glaucoma, cataract, inflammation, and foreign body toxicity posing
visual problems. Traumatic endophthalmitis and retinal detachment
are of particular concern because they tend towards the
rapid progression of severe visual loss.
For the asymptomatic nature of RILFB, probable implications
in this present case is perhaps attributable to the previous administration
of topical broad-spectrum antibiotics and antifungal
agents that controlled infection, the role of the inflammatory
response of lens opacification producing encapsulation and embedding
the foreign body, and possibly to ocular and systemic
immunological mechanisms. A previous study hypothesized the
sealant-like effect produced by anterior cuboidal cell proliferation
once the anterior capsule is disrupted thus protecting the foreign
body from deleterious agents.
A previous medical literature search revealed the asymptomatic
nature of metallic ILFB retained for 20 to 60 years. [6-8]
Scheimpflug imaging technology offered an alternate diagnostic
imaging modality for RILFB localization in another case study
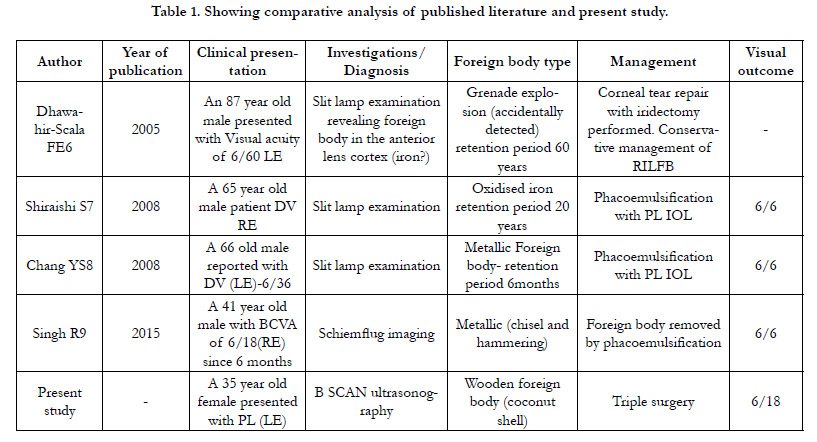
publication.[9] Table 1 The ideology of organic foreign bodies resulting
in fungal or combined infections has become questionable
and emphasizes the need for further studies about the implications
of retained organic foreign bodies and their response within
the eye. Arora R et al demonstrated foreign body removal by Kelman-
Macpherson forceps in contrast to spontaneous egression
during cortical clean-up procedures in the present case study.[10]
In conclusion, for patients with a history of stick-injury causing
leucomatous opacity, we recommend B scan ultrasound evaluation
of crystalline lens preoperatively to look for an embedded
intra lenticular foreign body and to perform triple surgery in a
single setting procedure that facilitates controlled intra-operative
maneuvers.
References
- Bastuji-Garin S, Rzany B, Stern RS, Shear NH, Naldi L, Roujeau JC. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol. 1993 Jan; 129(1): 92-6. PMID: 8420497.
- Chen CB, Hsu TH, Chung-Yee Hui R, Lu CW, Chen WT, Chiang PH, et al. Taiwan Severe Cutaneous Adverse Reaction Consortium. Disseminated intravascular coagulation in Stevens-Johnson syndrome and toxic epidermal necrolysis. J Am Acad Dermatol. 2021 Jun; 84(6): 1782-1791. PMID: 32828861.
- Fakoya AOJ, Omenyi P, Anthony P, Anthony F, Etti P, Otohinoyi DA, et al. Stevens - Johnson Syndrome and Toxic Epidermal Necrolysis; Extensive Review of Reports of Drug-Induced Etiologies, and Possible Therapeutic Modalities. Open Access Maced J Med Sci. 2018 Mar 28; 6(4): 730-738. PMID: 29731949.
- Fernando SL. Sifting through the history of the nosology of erythema multiforme, Stevens-Johnson syndrome, and toxic epidermal necrolysis and its clinicopathological relevance. Int J Dermatol. 2021 Jan; 60(1): 110-112. PMID: 33252777.
- Hasegawa A, Abe R. Recent advances in managing and understanding Stevens- Johnson syndrome and toxic epidermal necrolysis. F1000Res. 2020 Jun 16; 9: F1000 Faculty Rev-612. PMID: 32595945.
- Hsu DY, Brieva J, Silverberg NB, Silverberg JI. Morbidity and Mortality of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis in United States Adults. J Invest Dermatol. 2016 Jul; 136(7): 1387-1397. PMID: 27039263.
- Kaido M, Yamada M, Sotozono C, Kinoshita S, Shimazaki J, Tagawa Y, et al. The relation between visual performance and clinical ocular manifestations in Stevens-Johnson syndrome. Am J Ophthalmol. 2012 Sep; 154(3): 499- 511.e1. PMID: 22818907.
- Lerch M, Mainetti C, Terziroli Beretta-Piccoli B, Harr T. Current Perspectives on Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Clin Rev Allergy Immunol. 2018 Feb; 54(1): 147-176. PMID: 29188475.
- Paulmann M, Mockenhaupt M. Severe drug-induced skin reactions: clinical features, diagnosis, etiology, and therapy. J Dtsch Dermatol Ges. 2015 Jul; 13(7): 625-45. English, German. PMID: 26110722.
- Radcliffe Crocker H. Diseases of the skin, their description, pathology, diagnosis and treatment .... Lewis. 1903.
- Sinha A, Ma Y, Scherzer R, Hur S, Li D, Ganz P, et al. Role of T-Cell Dysfunction, Inflammation, and Coagulation in Microvascular Disease in HIV. J Am Heart Assoc. 2016 Dec 20; 5(12): e004243. PMID: 27998918.
- Stevens AM, Johnson FC. A new eruptive fever associated with stomatitis and ophthalmia: report of two cases in children. American journal of diseases of children. 1922 Dec 1;24(6):526-33.
- THOMAS BA. The so-called Stevens-Johnson syndrome. Br Med J. 1950 Jun 17; 1(4667): 1393-7. PMID: 15426760.
- Yetiv JZ, Bianchine JR, Owen JA Jr. Etiologic factors of the Stevens-Johnson syndrome. South Med J. 1980 May; 73(5):599-602. PMID: 7375977.
- Bastuji-Garin S, Rzany B, Stern RS, Shear NH, Naldi L, Roujeau JC. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol. 1993 Jan;129(1):92-6. PMID: 8420497.
- Ng PP, Sun YJ, Tan HH, Tan SH. Detection of herpes simplex virus genomic DNA in various subsets of Erythema multiforme by polymerase chain reaction. Dermatology. 2003; 207(4): 349-53. PMID: 14657624.
- Zhou D, Dai SM, Tong Q. COVID-19: a recommendation to examine the effect of hydroxychloroquine in preventing infection and progression. Journal of Antimicrobial Chemotherapy. 2020 Jul 1;75(7):1667-70.
- Davoodi L, Jafarpour H, Kazeminejad A, Soleymani E, Akbari Z, Razavi A. Hydroxychloroquine-induced Stevens-Johnson syndrome in COVID-19: a rare case report. Oxf Med Case Reports. 2020 Jun 25; 2020(6): omaa042. PMID: 32617169.
- Leckie MJ, Rees RG. Stevens-Johnson syndrome in association with hydroxychloroquine treatment for rheumatoid arthritis. Rheumatology (Oxford). 2002 Apr; 41(4): 473-4. PMID: 11961185.
- Chung WH, Hung SI, Yang JY, Su SC, Huang SP, Wei CY, et al. Granulysin is a key mediator for disseminated keratinocyte death in Stevens-Johnson syndrome and toxic epidermal necrolysis. Nat Med. 2008 Dec; 14(12): 1343-50. PMID: 19029983.
- . Wang CW, Yang LY, Chen CB, Ho HC, Hung SI, Yang CH, et al. Randomized, controlled trial of TNF-α antagonist in CTL-mediated severe cutaneous adverse reactions. J Clin Invest. 2018 Mar 1;128(3):985-996. PMID: 29400697.
- Gao X, Tang X, Ai L, Gao Q, Liao Q, Chen M, et al. Acute pancreatic injuries: A complication of Stevens-Johnson syndrome/toxic epidermal necrolysis associated with cytotoxic immunocell activation. J Am Acad Dermatol. 2021 Mar; 84(3): 644-653. PMID: 32561372.
- Shiohara T, Mizukawa Y, Aoyama Y. Monitoring the acute response in severe hypersensitivity reactions to drugs. Curr Opin Allergy Clin Immunol. 2015 Aug; 15(4): 294-9. PMID: 26110678.
- Ni F, Zhang Y, Peng X, Li J. Correlation between osteoarthritis and monocyte chemotactic protein-1 expression: a meta-analysis. Journal of Orthopaedic Surgery and Research. 2020 Dec; 15(1): 1-9.
- Zhao YC, Hu T, Chen Y, Du KT. Elevated Serum Levels of Monocyte Chemotactic Protein-1/Chemokine C-C Motif Ligand 2 are Linked to Disease Severity in Patients with Fibromyalgia Syndrome. Balkan Med J. 2019 Oct 28; 36(6): 331-336. PMID: 31486327.
- Lin J, Kakkar V, Lu X. Impact of MCP-1 in atherosclerosis. Curr Pharm Des. 2014;20(28):4580-8. PMID: 24862889.
- Lerch M, Mainetti C, Terziroli Beretta-Piccoli B, Harr T. Current Perspectives on Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Clin Rev Allergy Immunol. 2018 Feb; 54(1): 147-176. PMID: 29188475.
- Syed D, Iqbal O, Mosier M, Mitchell R, Hoppensteadt D, Bouchard C, et al. Elevated endocan levels and its association with clinical severity in Stevens-Johnson Syndrome and toxic epidermal necrolysis. Int Angiol. 2015 Oct; 34(5): 483-8. PMID: 25394955.
- Till SD, Iqbal O, Dharan A, Campbell E, Bu P. The roles of IL-33 and TGF-β1 in the pathogenesis of Stevens-Johnson syndrome/toxic epidermal necrolysis: potential biomarkers for disease severity. J Ophthalmol Eye Care. 2018; 1(1): 105.
- Sadek M, Iqbal O, Siddiqui F, Till S, Mazariegos M, Campbell E, et al. The Role of IL-13, IL-15 and Granulysin in the Pathogenesis of Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis. Clin Appl Thromb Hemost. 2021 Jan-Dec; 27: 1076029620950831. PMID: 33560872.