Short-Term Study Of IOL Position Changes using Ultrasound Biomicroscopy in High Myopia
Fayed AAE*
Assistant Professor, Ophthalmic Department, Banha University, Egypt.
*Corresponding Author
Ayser Abd EL-Hameed Fayed MD,
Assistant Professor, Ophthalmic Department, Banha University, Egypt.
Tel: 01005007489
E-mail: ayserfayed@yahoo.com
Received: April 07, 2017; Accepted: May 22, 2017; Published: May 23, 2017
Citation: Fayed AAE (2017) Short-Term Study Of IOL Position Changes using Ultrasound Biomicroscopy in High Myopia. Int J Ophthalmol Eye Res. 5(5), 316-321. doi: dx.doi.org/10.19070/2332-290X-1700065
Copyright: Fayed AAE© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To study the performance of the implanted both one-piece and three-piece IOLs in relation to the enlarged diameters of the capsular bags of the highly myopic eyes.
Subjects and Methods: Patient were randomly divided into two groups; group (A), included 25 eyes that underwent phacoemulsification with implantation of one-piece IOLs, Group (B) included 25 eyes that underwent phacoemulsification with implantation of three-piece IOLs. All patients include in this study were high myopes with axial length greater than 26.5 mm. All eyes were planned for clear lens extraction or cataract extraction.
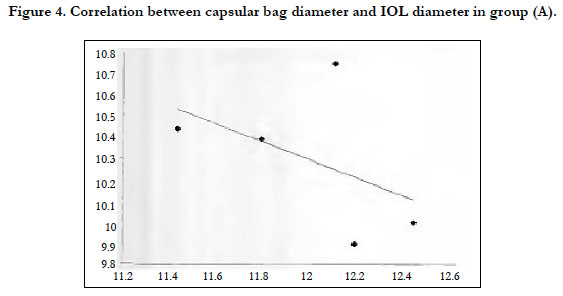
Results: In group (A), a statistically significant negative correlation was found between the diameters of the capsular bags and the diameters of the implanted on – piece IOLs. The correlation coefficient (r) is – 0.56. In group (B), a statistically significant positive correlation was found between the diameters of the capsular bags and the diameters of the implanted three-piece IOLs. The correlation coefficient (r) is 0.88.
Conclusion: The study of this correlation is to help in answering an important question, that is, does one diameter IOL fit every capsular bag? The statistical analyses in both groups point to statistically significant correlation between the diameters of the capsular bags and the diameters of the implanted IOLs i.e. focuses to the divergence between the size of the IOLs and that of the capsular bag.
2.Subjects and Methods
2.1 Exclusion Criteria
2.2 Preoperative Examination for All Patients Included
3.3 Postoperative Ultrasound Biomicroscopy
3.Results
4.Discussion
5.References
Introduction
Ultrasound is basic device in therapeutic imaging and has a critical part in ophthalmologic diagnoses. Conventional B-scan examinations produce two-dimensional cross-sectional views of the eye and orbit. This strategy for imaging is the most vital examination system for intraocular lesions, particularly in the presence of anterior segment opacities; be that as it may, there are confinements to ordinary ultrasound [1].
UBM gives images in living eyes without influencing the internal relationship of the imaged structures. It provides information that was unobtainable by other non-invasive approaches. It now allows structural details of the angle, visualization of the area posterior to iris and ciliary body; and to evaluate unequivocally anatomic relations among the anterior segment structures [2].
UBM provides a unique technique to test the e-act IOL location and its relationship to adjacent ocular structures. Moreover, UBM provides reproducible measurements of the distances between the IOL and these structures. It produces short wavelengths, that provide higher solution and accurate measurement but at the expense of penetration [3].
Most IOL organizations make a given IOL model with one diameter for implantation in the capsular bag, considering a certain uniformity of the capsular bags receiving these IOLs. The measurement of the crystalline focal point is not the same in everyone's eyes; however, in any case, a solitary IOL distance across may not in a perfect world fit every capsular bags. Notwithstanding individual variety, axial length and age are additionally outstanding components in deciding crystalline lens diameter. This variability in the extent of the capsular bag can be a reason for postoperative IOL complication including decentration, tilt and refractive insecurity [4]. Postoperative refraction deviations may develop through the postoperative axial movement of the optic; tilt and /or decentration of the IOL [5, 6].
In myopic eye with a larger capsular bag, the use of the same IOL size could lead to an insufficient capsular tension, resulting in asymmetrical IOL fixation, capsular fold and an increased likelihood of PCO [7]. This circumstance prompts to various inquiries, what is the anatomical position of the IOL and capsular bag in in various sized eyes embedded with IOLs of a similar diameter? Could increasing IOL diameters, as a function of the increasing axial length of the eye, improve the anatomical and functional results of bag implantation? Could experimentation enhance the flexibility of such an IOL system? [4].
Subjects and Methods
Patients were arbitrarily divided into two groups; group (A) and group (B). Group (A) included 25 eyes that underwent phacoemulsification with implantation of one-piece IOLs (Corneal IOLs, Optic diameter = 6.00 mm, overall diameter = 12.00 mm). The mean age was 47.07 years (SD +22.03). Group (B) included 25 eyes that underwent phacoemulsification with implantation of three-piece IOLs (Acrysof IOLs, optic diameter = 6.00mm, overall diameter = 13.00mm). The mean age was 50.47 years (SD + 15.72).
All patients include in this study were high myopes, with axial length greater than 26.5 mm . The spherical equivalent in all patients was more than – 6 D. they were patients who planned for clear lens extraction or cataract extraction with no other ocular pathology. The patients were recruited from the outpatient clinic of the ophthalmology department of Benha University Hospitals through the period since December 2008 till January 2015. The Institutional Review Board of the College of Medicine University of Banha, approved the study protocol, and Informed assent was obtained by all patients settled upon consideration.
Any ocular pathology (other than cataract), included, corneal opacities, History of previous ocular surgery, Lens subluxation and pseudoexfoliation syndrome, any surgical complications, such as, ruptured posterior capsule, cases that had sutured wounds and cases that didn't show in the bag implantation of their IOLs during the postoperative follow-up.
Full medical history, refraction whenever possible, best corrected visual acuity, IOP measurement by applanation tonometry, slit lamp examination for conjunctiva, cornea, anterior chamber, iris and lens. Fundus examination by indirect opthalmoscope, whereas, ultrasonography was restored to access fundus in opaque media, Ultrasonic measurement of the axial length of the eye, A-scan biometry for IOL power calculation in which the SRK-T formula was used to calculate the IOL power as the targeted postoperative refraction was-1D, Ultrasound biomicroscopy were done for the patients. Preoperative ultrasound biomicroscopic measurement using UBM model (DICON, UBM plus, Model 45, Paradigm® Medical Industries Inc.) Included, central anterior chamber depth (ACD): distance between the center of the posterior corneal surface (corneal endothelium) and the anterior lens capsule, angle opening distance 500um from the scleral spur (AOD 500um): which is the degree of anterior chamber angle opening. It was measured in the four quadrants of the angle (nasal temporal, superior and inferior quadrants) and Trabecular - iris angle (TIA), which was also measured in the temporal, quadrants).
Postoperative ultrasound biomicroscopy was done. The following parameters were measured to be compared with the corresponding preoperative values.
Anterior chamber depth (ACD), Angle opening distance 500um from scleral spur (AOD 500um), Trabecular-iris angle (TIA), Diameters of the capsular bag, was, measured from the equatorial edge of the capsular bag, Diameters of the implanted intraocular lens diameter, was measured from the end of one haptic to the end of the other haptic and White to white distance, was measured from the outer aspect of the corneo-junction on one side to the opposite side.
The obtained measurement were then statistically analyzed and correlated together in each group of patients in order to be used in the study of the relationship between the diameters of the capsular bags of the highly myopic eyes and the diameters of the implanted IOLs (including one-piece and three-piece IOLs).
Comparison of quantitative variables between the 2 groups was done using Student t test. Comparison between pre and postoperative data was done using paired t test for comparing categorical data. Chi square (X2) test was performed. The association between two variables was done using correlation coefficient. A probability value (P value) less than 0.05 was considered statistically significant. P value less than 0.001 was considered statistically highly significant. P value more than 0.05 was considered statistically non-significant. All statistically calculations were done using SPSS version 16 (Statistical Package for the Social Science; SPSS inc., IL, USA) program.
Results
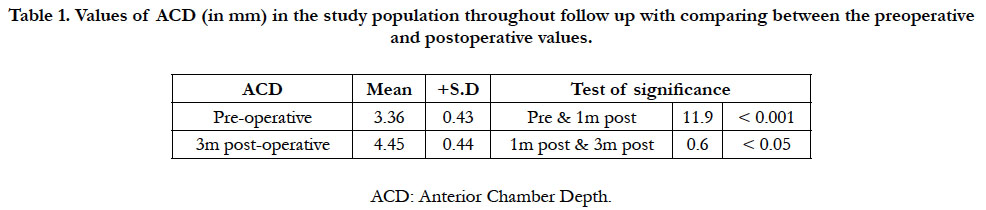
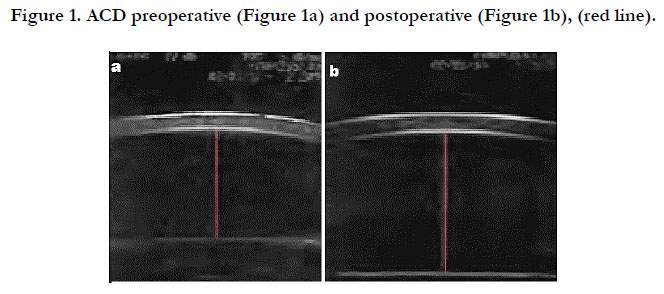
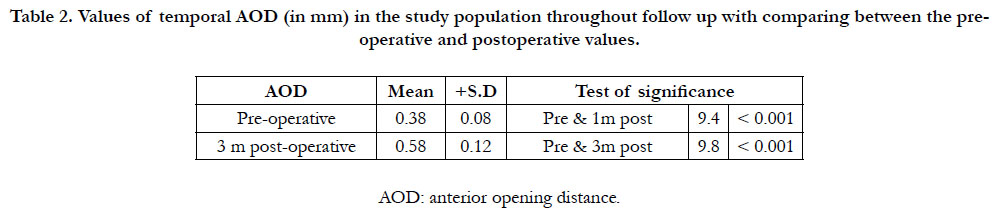
In 30 patients, 11 women (36.6%) and 19 men(63.3%) with a mean age of 49.07 years, 50 eyes were examined who are high myopes. The patients were divided into two groups; group (A), included the patients who underwent implantation of one-piece IOLs where group (B) included the patients who underwent implantation of three-piece IOLs. Detailed statistical analysis of each of the measured parameters was done with comparing the preoperative values to the postoperative values. The mean increase in ACD was 1.1 mm, approximately 32% deeper than before surgery, represented in Table (1), Figure (1a, b). AOD 500um significantly increased postoperatively in four cardinal quadrants of the globe, with highly significant correlation, Table (2).
Table 1. Values of ACD (in mm) in the study population throughout follow up with comparing between the preoperative and postoperative values.
Table 2. Values of temporal AOD (in mm) in the study population throughout follow up with comparing between the preoperative and postoperative values.
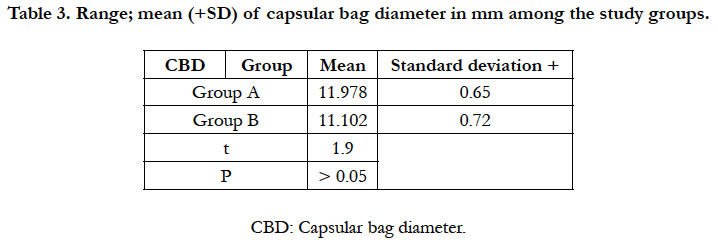
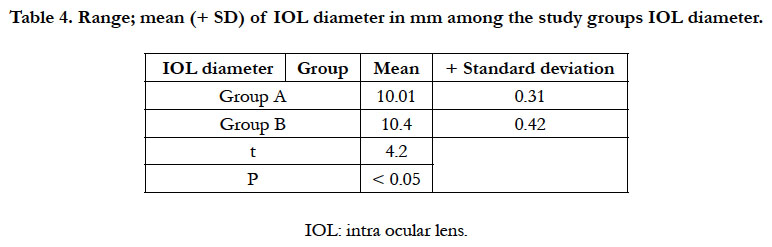
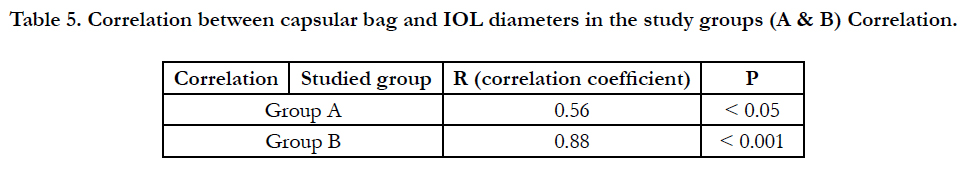
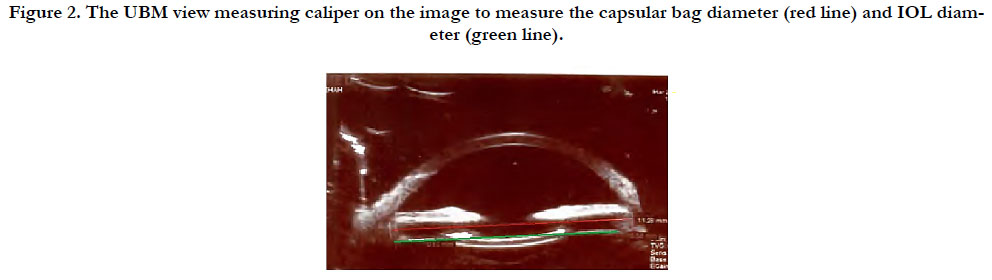
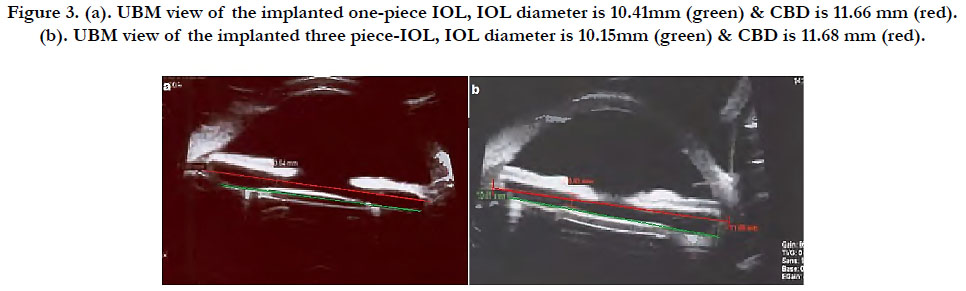
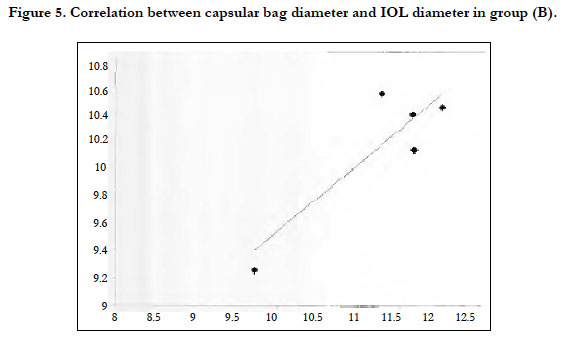
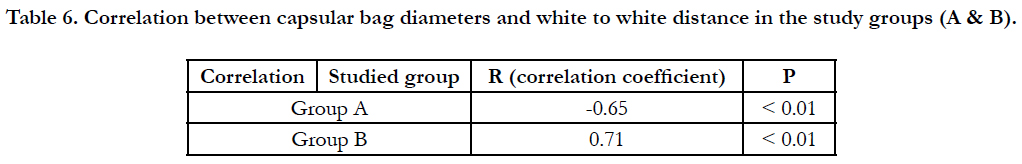
Postoperatively, the diameters of the capsular bags and those of the implanted IOLs were measured in either group then the measured values were statistically analyzed & correlated together, Table (3, 4, 5), Figuer (2). The measured values of the capsular bag diameter in groups (A) & (B) were not statistically different, whereas, comparing CBD in relation to the implanted IOL diameter, In group (A), a statistically significant negative correlation was found between the diameters of the capsular bags and the diameters of the implanted on – piece IOLs. The correlation coefficient (r) is – 0.56, Table (5) Figure (3a, 4). In group (B), a statistically significant positive correlation was found between the diameters of the capsular bags and the diameters of the implanted three-piece IOLs. The correlation coefficient (r) is 0.86, Table (5), Figure (3b, 5). In both groups; a statistically significant positive correlation was found between the capsular bag diameter and the white to white distance, Table (6).
Table 5. Correlation between capsular bag and IOL diameters in the study groups (A & B) Correlation.
Figure 2. The UBM view measuring caliper on the image to measure the capsular bag diameter (red line) and IOL diameter (green line).
Figure 3. (a). UBM view of the implanted one-piece IOL, IOL diameter is 10.41mm (green) & CBD is 11.66 mm (red). (b). UBM view of the implanted three piece-IOL, IOL diameter is 10.15mm (green) & CBD is 11.68 mm (red).
Table 6. Correlation between capsular bag diameters and white to white distance in the study groups (A & B).
Discussion
An important aim of this thesis is to identify and quantify the changes in the anterior segment configuration of the highly myopic eyes after phacoemulsification and foldable intraocular lens (IOL) implantation, by means of ultrasound biomicroscopy (UBM). Thus, UBM was performed to measure the anterior segment parameters both preoperatively and at the first and third postoperative months. In the present study, the mean postoperative ACD was 4.48 mm (SD + 0.42) at the first postoperative month, and was 4.45 mm (SD + 0.44) at the third postoperative months, comparing to the mean preoperative ACD of 3.36 mm (SD + 0.49). So, the mean difference in ACD was 1.1 mm, approximately 32% deeper than before surgery, which is statistically highly significant (P value < 0.001).
Similarly, AOD 500um significantly increased postoperatively in four cardinal quadrants of the globe, with highly significant. As for the TIA, the present study revealed the difference between preoperative and postoperative was statistically highly significant. The above mentioned result of the present study are supported by similar results reported by other studies [8-10].
The present review was an endeavor in answering critical question, that is, does one - diameter IOL is suitable for every capsular bags? For this purpose, two different IOL types with different overall diameters were used in this study and the selected patients were high myopes with axial length greater than 26.5 mm. The spherical equivalent in all patients was > -6 D. the diameters of the implanted IOLs and those of the capsular bags were measured in all eyes then statistically analyzed and correlated together in each group.
In group (A) in which one – piece IOLs (with overall diameter of 12 mm) were implanted, the mean diameter of the implanted one-piece IOLs was 10.01 mm. The correlation between the measured IOL and capsular bag diameters in this group was found to be statistically significant (P < 0.05). Moreover, this correlation was found to be negative (r = -0.56). This means that from the statistical point of view, the larger the capsular bag diameter was, the smaller the IOL diameter was.
In group (B) in which three-piece IOLs (with overall diameter of 13 mm) were implanted; the mean diameter of the implanted three-piece IOLs was 10.4 mm. The correlation in this group between the measured IOL and capsular bag diameters was additionally statistically highly significant (P < 0.001). It is a positive correlation in which the correlation coefficient r is 0.81. So from the statistical point of view the larger the capsular bag diameter was, the larger the IOL diameter was.
On looking at the estimations of the measured diameters of the implanted on-piece and three-piece IOLs, a statistically significant difference was found between the two IOLs types (P < 0.05). The statistical analyses in both groups point to statistically significant correlation between the diameters of the capsular bags and the diameters of the implanted IOLs in both groups (A & B), demonstrates absence of fitting of both sorts of IOLs in relation to the enlarged capsular bags of the highly myopic eyes i.e. focuses to the divergence between the size of the IOLs and that of the capsular bag.
Additionally, on comparing the two IOL types together, the three piece IOLs appear to show better anatomical fitting in the capsular bags than the one-piece IOLs. This is attributed to the negative correlation found in group (A) between the diameters of the capsular bags and those of the one-piece IOLs in contrast to the positive correlation found in group (B) between the diameters of the capsular bags and those of the three-piece IOLs and is also attributed to the statistically significant difference found between groups (A) & (B) regarding the measured values of the IOL diameters.
On the premise results found out by this thesis speak to an endeavor to answer an important question mentioned above, that is, does one diameter IOL fit all capsular bags? Actually the answer of this question is not known yet and even the studies attempting to answer it are still very few.
In 2009 an experimental study was performed by Sourdille [4] to analyze 25 eyes in which phacoemulsification was done and the capsular bags were implanted with different IOLs of different diameters (including one-piece and three-piece designs) then the modifications that were incited in the shape and size of the capsular bags were measured with the guide of high-frequency ultrasound. Three of the implanted three-piece IOL models reliably expanded and ovalized the capsular bags, frequently causing central capsular folds and these IOLs likewise moved the bag into a retrociliary position. On the other hand, the one-piece IOLs implanted in this study caused no fold and no ovalization of the capsular bags, presumed that an IOL fabricated with only a solitary measurement did not anatomically fit every capsular bags.
He also concluded that the concept behind the lens which expresses that high axial myopic eyes need larger IOL diameters and shorter eyes get shorter IOL diameters enhances the anatomical circumstance and may maintain best refractive results. These finding were clinically attested in another late propective randomized bilateral clinical study [5].
All the above mentioned results point to the importance of the adaptability of the IOL diameter to the different bag sizes and the correlations of the IOL diameter with the dioptric power and the axial length of the eye should result in better capsular bag fitting. Moreover the difference in the capsular bag size of the highly ammetropic eyes may result in unpredicatable IOL position with inaccurate refractive outcome.
The measured values in this thesis were used to calculate a stepwise multiple regression analysis which was computed with capsular bag diameter as the dependent variable. This formula used the white to white distance of the eye to calculate the CBD. It is as follows; Capsular bag diameter = 1.023 X white to white distance -0.839. This formula represents an attempt to find an accurate method for predicting the capsular bag diameter.
The statistical analyses performed in this study point to lack of fitting of both types of IOLs in relation to the enlarged capsular bags. It also shows that 3-piece IOLs appear to be better anatomically fitting in the capsular bags than the 1-piece IOLs. Does onediameter IOL is suitable for every capsular bags? is an important question which needs many future studies with large number of high ammetropia and different design of IOL needed to be answered correctly.
References
- Pavlin CJ, Harasiewicz K, Sherar M, Foster F (1991) Clinical use of Ultrasound Biomicroscpy. Ophthalmol. 98(3): 287-295.
- Pavlin CJ, Foster FS (1995) Basic consideration. Ultrasound Biomicroscopy of the eye. (1st edn), New York ; Springer Verlag . 3-60.
- Jimenez-Alfaro I, Gracia-Feijio J, Perez –Santonja J, Cuina R (2001) Ultrasound biomicroscopy of ZSAL-4 anterior chamber phakic intraocular lens for high myopia. J Cataract Refract Surg. 27(10): 1567-1573.
- Sourdille P (2009) Relationship between lens and capsular bag size. J CRST Europe. 21-24.
- Vass C, Menapace R, Schmetterer K, Findl O, Rainer G, et al., (1999) Prediction of pseudophakic capsular bag diameter based on biometric variables. J Cataract Refract Surg. 25(10): 1376- 1381.
- Koeppl C, Findl O, Kriechbaum K, Sacu S, Drexler D (2005) Change in IOL position and capsular bag size with an angulated intraocular lens early after cataract surgery . J Cataract Refract Surg. 31(2) : 348-353.
- Georgopoulos M (2009) Can variable IOL diameter result in improved fitting influence on IOL axial position , centration and incidence of PCO? Ophthalmology Time Europe.
- Pereira FA, Cronemberger (2003) Ultrasound Biomicroscopic Study of Anterior Segment Changes after Phacoemulsification and Foldable Intraocular Lens Implantation . Ophthalmology. 110(9): 1799-1806.
- Kurimoto Y, Park M , Skaue H, Kondo T (1997) Changes in the anterior chamber configuration after small incision cataract surgery with posterior chamber intraocular lens implantation. Am J Ophthalmol. 124(6): 775-780.
- Guo XP, Gao Y, Chen G, Liu XL (2004) Quantitative study of anterior chamber angel with ultrasound biomicroscopy after cataract surgery with phacoemulsification and foldable intraocular lenses implantation. Zhonghua Yan Ke Za Zhi. 40: 94-6.