Willingness to Pay for Cataract Surgery Among Outreach Site Patients in South West Ethiopia: A Cross-Sectional Study
Gessesse GW, Demissie BS*
Department of Ophthalmology, Jimma University, Jimma, Ethiopia
*Corresponding Author
Berhan S. Demissie,
Department of Ophthalmology,
Jimma University, Jimma, Ethiopia,
E-mail: sberhan95@yahoo.com , girumgw@yahoo.com
Article Type: Research Article
Received: September 03, 2014; Accepted: September 16, 2014; Published: September 17, 2014
Citation: Gessesse GW, Demissie BS. (2014). Willingness to Pay for Cataract Surgery Among Outreach Site Patients in South West Ethiopia:A Cross-Sectional Study, Int J Ophthalmol Eye Res, 2(6), 65-69. doi: dx.doi.org/10.19070/2332-290X-1400012
Copyright: Demissie BS© 2014. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Cost recovery for cataract surgery will have significant input towards a sustainable eye care system; therefore it is important to assess the willingness to pay of patients with cataract blindness for cataract surgery.
Methods: A cross sectional survey was conducted in two outreach sites in South West Ethiopia to determine their willingness to pay for
cataract surgery. Consecutive patients who had mature senile cataract and came to two outreach program sites were included in the study.
Results: A total of 134 patients were included in the study. The mean age was 62.5years (SD=9.4). The majority, 86 (64.2 %), were males
making the male to female ratio 1.79:1. A total of 102 (76.1%) participants of the study said that they were willing to pay for their cataract
surgery. Males were more willing to pay as compared to females (83.7% vs. 62.5%, p=0.006). Those with low socio-economic conditions
were less willing to pay (p< 0.05). Willingness to pay was not associated with the age (p= 0.25), literacy (p=0.66), religion (0.3), or family size
(0.43) of the participants. On multiple logistic regression analysis, however, only being a female and also having a low socioeconomic status
were significantly associated with not willing to pay.
Conclusions: A good proportion of the rural residents were willing to pay for their cataract surgery. Being female and having lower socioeconomic
status are associated with not willingness to pay.
2.Background
3.Methods
4.Operational Definitions
5.Results
5.1.Willingness to pay
6.Discussion
7.Conclusions
8.List of abbreviations
9.Competing interests
10.Authors' contributions
11.Acknowledgements
12.References
Keywords
Cataract, Willingness To Pay, Jimma, Ethiopia.
Background
Age-related cataract is the most prevalent cause of blindness globally [1], and in Ethiopia alike [2]. The only effective treatment of cataract is surgery and it is widely known that cataract surgery is one of the most cost effective interventions in medicine [3,4].The amount spent for the surgery for restoring vision to the cataract blind is said to be a fraction of what can be lost from a cataract blind person in terms of his/her productivity.
The aim of cataract surgery is to rehabilitate blind or visually impaired people by restoring their sight to normal or as near to normal as possible. The cataract surgical rate in Ethiopia is one of the lowest in the world, about 360. There are numerous reasons why patients who are blind and visually impaired from un-operated cataract do not receive the surgical services they need. A recent study done in Central Ethiopia identified cost of surgery (91.8%), insufficient family income (78.1%) and the distance to hospital (47.9%) as the three major factors that delayed cataract surgery [5], while another study has found that the main barrier for seeking service is related to the indirect medical costs of the service [6]. Apart from the indirect costs, patient costs for cataracts include the costs of supplies and equipment related to the surgical procedures.
The major sources of funding for cataract surgeries in Ethiopia are donor organizations operating through governmental or nongovernmental institutions. The emphasis is in offering the service to the poor and it is either free of cost (in many cataract campaigns conducted in rural areas), or at a very low price (as in many governmental hospitals). Patient fees, as a source of financing the eye care program, are mainly the mode of delivery in private institutions in the country. There are very limited numbers of such institutions in the country and they contribute a little to the overall cataract surgical rate.
Identifying the total cost of delivering certain health care like cataract surgery and having a constant source of finance are key elements in ensuring sustainability of the program. This allows in devising means of providing the service in overall reduced cost and optimizing utilization of manpower and resources for the maximum output. While evaluation of the cost of delivery of a health care allows creation of solutions for effective cost control, knowledge of willingness of the public to pay and the amount they can afford, should serve as a directive to devise an appropriateapproach.A study done in rural Malawi [7] to assess the willingness to pay (WTP) for cataract surgery of cataract blind patients identified 64.2% to be willing to pay, while another study done in Kathmandu valley [8] found 42.3% to be willing.
There is no study which has looked into the willingness of the rural residents to pay for a cataract surgery in Ethiopia. Therefore, this study was undertaken to determine the willingness of adult patients with cataract blind to pay for the surgery and the factors associated with willingness to pay for the surgery. It will be the first of its kind in evaluating this issue and we assume that it will also give valuable information for planning on cataract blindness in our community.
Methods
A cross sectional survey was conducted in two outreach sites in South West Ethiopia to determine the willingness of patients with cataract blind to pay for the surgery among adults who underwent cataract surgery in August and October 2012 in Bedele and Limu Hospitals respectively. The hospitals are of same level with regard to patient care and service provision and both are located in Oromia regional state of Ethiopia. These areas are two of the regular outreach sites of Jimma University department of ophthalmology (JUDO) with a distance of 250 km (Bedele) and150 km (Limu) from the base hospital in Jimma.
A total of 134 consecutive patients who had blindness due to senile cataract and came to the hospitals for the outreach program in the first week of the schedule and were willing to participate in the study were included in the study. Subjects with ‘white cataract’ (initial acuity worse than 3/60 and this was explained by the presence of dense cataract) were eligible for the study. Only senile type of cataract was included to make possible generalizability of the study to this most common form of adult blindness in the country and the region.
The study was both qualitative and quantitative type. A structured questionnaire was designed for the purpose of the study. The questionnaire was administered by ophthalmic nurses and includes socio-demographic characteristics of persons with senile cataract blindness, their economic condition as well as enquiry on their willingness to pay for cataract surgery. Data were collected with face to face interview with the patients that required 5–10 minutes to administer. The questionnaire was administered after a diagnosis of white dense cataract was made and before they were subjected to pay for the surgery. Ethical clearance was obtained from Jimma University Research and Publications Committee and the study was done with adherence to the guidelines of the Declaration of Helsinki. The respondents were briefed about the survey by their local language and informed verbal consent on the willingness of each patient to participate in the study was obtained before interview. Data was analyzed using computer software SPSS version 16. Proportion of people willing to pay for the cataract surgery was calculated. It also includes analysis of socio-demographic and economic factors. Comparison of factors between cases (persons who are willing to pay) and non- cases (persons who are not willing to pay) was also done. P-values less than 0.05 were considered to be significant.
Operational Definitions
Blind- Those above 45 years of age presented with visual acuity of less than 3/60 due to cataract.
Outreach sites- Bedele and Limmu general hospitals
Senile cataract- Lens opacity resulting in visual reduction of less than 3/60 in those above 45 years of age.
Willingness to pay- Blind patients who agree to pay money for the cataract surgery they will get.
Results
A total of 134 adults were interviewed in this study, involving 70% of the participants during the study period. The mean age was 62.5years (SD=9.4) with a range of 45- 80 years. The majority (35.8%) were in the age group 45-54 years while 16.4% were aged 75 years and above. Eighty-six (64.2 %) were males making the male to female ratio 1.79:1 (Table 1). From all participants 86 (64.2 %) were married while 36 (26.9%) were widowers. The majority,114 (85.1%) were illiterates.
Table 1. Baseline characteristics of participants, with their willingness to pay for cataract surgery, Southwest Ethiopia
Eighty-two (61.2%) of the participants were farmers while 44 (32.8%) were housewives. The majority, 96 (71.6) were Christians while 38 (28.4%) were Muslims. The mean number of family size was 4 (with a range of 1- 10), out of which 62 (46.3%) had less than 4 family member (Table 1).
In a developing country like Ethiopia, it is very difficult to assess the economic status of individuals. Economic status was assessed indirectly by categorizing the participants in to three as category 1, 2 and 3 (based on whether they are employed or not, and financially dependent on others or not).The majority, 86 (64.2%) of them were not employed but not financially dependent while all the rest, 48 (35.8%),were not employed and also financially dependent on others. Among the study subjects there was no individual employed (category I).As the majority of the rural residents were farmers, we also questioned whether they have a farmland, and 100 (74.6%) of them said they have their own farmland.
A total of 104 (77.6%) participants said that they are responsible for decision making to seek medical care and attend surgery while 22.4 % said they cannot decide by themselves and either their spouse or children are the ones who would decide.
A total of 102 (76.1%) participants of the study said that they are willing to pay for their cataract surgery. While 70% of them were willing to pay 200ETB or less for one eye surgery, the smallest and largest amounts were 50 ETB and 1000 ETB respectively. The mean was 223.3 (SD= 138.4)
On univariate analysis, WTP was not associated with the age (p= 0.25), literacy (p=0.66), religion (0.3), or family size (p=0.43) of the participants.Males were more willing to pay as compared to females (83.7% vs 62.5%, p=0.006). Eighty-one percent of married individuals were WTP while 66.7% of singles were willing to pay though the difference between the two was not statistically significant (p= 0.05).
Those who own a farmland were more likely to be willing to pay than those without farmland (OR 4.67, 95 CI 1.98- 11.01). Based on the economic category of the patients, 83.7% of those in category II (not employed but not financially dependent) were willing to pay as compared to 62.5% of those in category III (not employed and financially dependent on others). This was also statistically significant (p=0.01).
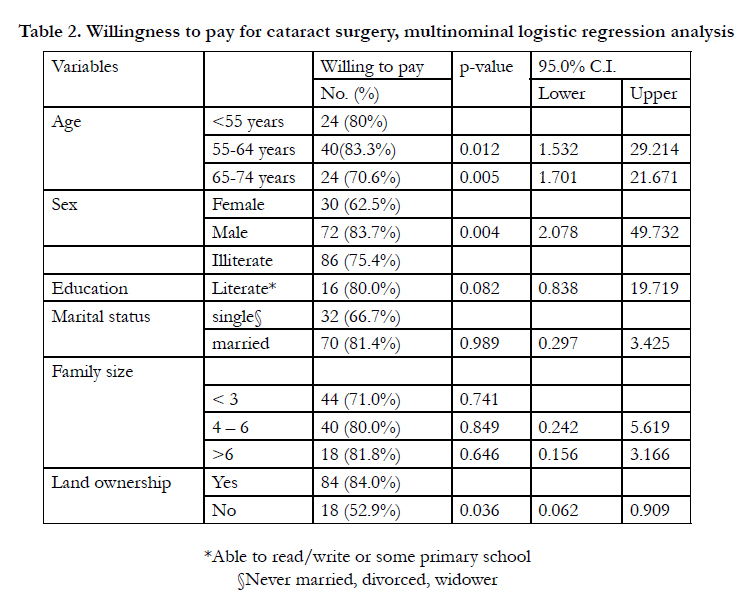
On multiple logistic regression analysis, however, only being a female and also having a low socioeconomic status were significantly associated with willingness to pay (table 2).
We also asked and evaluated whether the functional consequences as a result of cataract can matter on their WTP. Women who had difficulty cooking due to their poor vision were more likely to be willing than those without the difficulty (76.9% vs. 63.6%). However, this was not statistically significant (p= 0.3). Similarly, having difficulty identifying people from distance or on farming for both sexes were not associated with willingness to pay (p= 0.46, p= 0.8 respectively) (table 3).
Discussion
Having a constant source of finance is the key element in ensuring sustainability of a health care program and regular evaluation of the cost of delivery of a health care allows creation of solutions for effective cost control.
Cataract surgeries at outreaches are performed either free of charge or at a generally low cost which does not account the fixed cost, cost of consumables used like viscoelastics and intraocular lens as well as the provider costs.
Cataract surgery was provided to cataract blind people residing in JUDO outreach sites free of charge till two years back when patients were asked to pay about 100 Birr (5.31 USD) on average for one eye cataract surgery. Though patients pay before having the surgery, their actual willingness to pay for the service has not been evaluated. This study is therefore, the first of its kind in evaluating the willingness of the patients to pay for the surgery they get. We assume it will also serve as a starting point for a large scale study involving other geographic regions in the country.
In this study 76.1% of the study subjects were willing to pay for the cataract surgery. This is in comparison to 64.2% of patients in rural Malawi[7] and 64% in Kilimanjaro, Tanzania[9] were willing to pay something to the cataract surgery they get. Our study showed significant proportions of both males and females to be willing to pay.
Males showed more willingness to pay than females and this could be because in our society males still play significant role in decision making in family matters including health care services. It may also be related with economic condition as men earn and possess more money and wealth than women. In the Malawi study as well males were more willing to pay than females [7].
As one might imagine, low socioeconomic status of the family is also statistically significantly associated with less willingness to pay for cataract surgery service. In a similar study made in Nepal poverty and lack of family support together accounted for 73% of cases who were unwilling to pay for the service [8]. In another study at rural china, people with better sources of income would like to pay more money than those with low level of income [10].
People in the rural communities are farmers and largely depend on their farmland products and cattle raising as substantial sources of income for their livings. In these areas of the country where we did the study, coffee is the main product and source of income for the farmers and the larger the size of the land they own the bigger is the product and relatively wealthier they are compared to those without farmland. In this study those cataract patients who own farmland were more likely to pay for surgery compared to those without farmland. In the study done in Tanzania [9], wealth is significantly associated with willingness to pay at both sites of the study. In another study done in Malawi people who were willing to pay have got higher ownership of Maize crop [7]. In our study there were no statistically significant associations between willingness to pay and age, level of education, religion or family size.
We have not considered whether the visual acuity of patients could affect their willingness to pay. Indirectly, we assessed whether patients had functional consequence of their cataract and we have not found significant association of this with willingness to pay. Studies comparing visual acuity have shown mixed results; the China [10] and Kathmandu valley [8] studies found those with bilateral blindness to be more willing to pay than those with unilateral blindness, while a Malawi [7] study showed that pre-operatively blind patients were less willing to pay money towards the cost of their surgery compared to those with better visual acuity.
Cataract and poverty are interconnected. Cataract surgery can contribute to poverty alleviation, particularly among the most vulnerable members of society. Studies have shown that increased provision of cataract surgery to poor people with blindness may help to alleviate poverty and achieve the Millennium Development Goals [11]. Our study has clearly demonstrated that those with low socioeconomic status to be less willing to pay and should be addressed with special attention.
As the study area is one of the naturally prosperous regions in the country, known for the production of cash crops like coffee, the results of this studyhence cannot be generalized for the wholeof the country. Similar studies in other regions in the country are recommended
Conclusions
A significant proportion of patients who needed cataract surgery in these outreach sites were willing to pay for the surgery they get. Doing cataract campaigns free of charge in different areas in the country should be reconsidered as there appears to be potential of some cost recovery by the patients and this is helpful to create a sustained eye care program in the country.
List of abbreviations
JUDO: Jimma University Department of Ophthalmology.
WTP: Willingness to pay
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
Both BSD and GWG participated in the design of the study and coordination and helped to draft the manuscript. Both authors read and approved the final manuscript.
Acknowledgements
We would like to thank all the participants for their participation in the study. We would also like to thank the data collectors and the administrators of Bedele and Limu general hospitals.
References
- Resnikoff S, Pascolini D, Etya’ ale D, Kocur I, Pararajasegaram R, et al. (2002) Global data on visual impairment in the year 2002. Bull World Health Organ 82:844-51.
- Berhane Y, Worku A, Bejiga A, Adamu L, Alemayehu W, et al. (2007) Prevalence and causes of blindness and Low Vision in Ethiopia. Ethiop J Health Dev 21 (3):204- 210.
- Khadem M (1999) Outcomes of cataract surgery: Implications for the developing world. J Med Syst 23:281–289.
- Rob B, Mariame S, Silvio PM (2004) Cost-effectiveness analysis of cataract surgery: a global and regional analysis. Bull World Health Organ 82:338-345.
- Mehari ZA (2013) Barriers to Cataract Surgical Uptake in Central Ethiopia. Middle East Afr J Ophthalmol 20 (3): 229–233.
- Melese M, Alemayehu W, Friedlander E, Courtright P (2004) Indirect costs of eye care as a barrier to services as a barrier to service use in Ethiopia. Trop Med Int Health 9(3):426-31.
- Dean WH, Sherwin JC, Kumwenda S, Angeletti M, Wiehler U (2012) Willingness to Pay for Cataract Surgery in Post-operative Cataract Patients in Rural Malawi. Ophthalmic Epidemiology 19(5), 265–271.
- Shrestha MK, Thakur J, Gurung CK, Joshi AB, Pokhrel S,et al. (2004) Willingness to pay for cataract surgery in Kathmandu valley. Br J Ophthalmol 88(3):319–320.
- Lewallen S, Geneau R, Mahande M, Msangi J, Nyaupumbwe S, et al. (2006) Willingness to pay for cataract surgery in two regions of Tanzania. Br J Ophthalmol 90(1):11–13.
- He M, Chan V, Baruwa E, Gilbert D, Frick KD, et al. (2007) Willingness to pay for cataract surgery in rural Southern China. Ophthalmology 114(3):411–416.
- Kuper H, Polack S, Mathenge W, Eusebio C, Wadud Z, et al. (2010) Does Cataract Surgery Alleviate Poverty? Evidence from a Multi-Centre Intervention Study Conducted in Kenya, the Philippines and Bangladesh. PLoS ONE 5(11): e15431.