Photo Documentation In Ocular Trauma
Shahid E1*, Rasool R2, Arshad S3, Nisar S4, Jaffery A5
1 Senior Registrar Ophthalmology, Abbasi Shaheed Hospital Karachi,Pakistan
2 Demonstrator, Forensic Medicine&Toxicology, Karachi Medical And Dental College, Pakistan
3 Professor And Head Of Department Ophthalmology, Abbasi Shaheed Hospital Karachi, Pakistan
4 Associate Professor, Ophthalmology, Abbasi Shaheed Hospital Karachi, Pakistan
5 Assistant Professor, Ophthalmology, Abbasi Shaheed Hospital Karachi, Pakistan
*Corresponding Author
Erum Shahid,
Senior Registrar Ophthalmology,
Abbasi Shaheed Hospital Karachi,
Pakistan.
Tel/Fax: 0321-2958058
E-mail: drerum007@yahoo.com
Article Type: Research Article
Received: July 14, 2014; Accepted: July 24, 2014; Published: July 26, 2014
Citation: Shahid E, et al. (2014). Photo Documentation In Ocular Trauma, Int J Ophthalmol Eye Res, 2(4), 49-53. doi: dx.doi.org/10.19070/2332-290X-140009
Copyright: Shahid E© 2014. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: Aim of the study is to photograph different cases of ocular trauma to ensure the safety of an ophthalmologist in giving prognosis and avoiding problems which are faced in court of law in criminal cases.
Study Design: Hospital based, Cross sectional descriptive study.
Place And Duration: Department of ophthalmology, Abbassi Shaheed Hospital, Karachi. From July 2013 to March 2014.
Material And Method: Hundred (100) Patients of ocular trauma were enrolled in the study on basis of nonprobability consective
sampling. Their photographs were taken with the help of camera Kowa Fx 50 R. Blunt and penetrating injuries were included. Anterior
and posterior segment findings were photographed. Comatose, younger than 6 years, corneal abrasions and corneal foreign bodies were
excluded from the study. Data was analyzed on SPSS version 16.
Result: Among 100 patients (72) were males with male to female ratio of 3:1. Close globe injuries were (64) and open globe injuries were
(36). lid cut 6%, subconjunctival hemorrhages 10%, corneal cut 28%, hyphema 10%, subluxated lens 4%, cataract 10%, traumatic aniridia
2%, Choroidal rupture 4%, Traumatic optic atrophy 2% and Commotio retinae 2%.
Conclusion: Ocular photographs are the best evidence to be used in medico legal cases and compensatory purposes. The new aspect to
be highlighted is to photograph every case of an ocular trauma to avoid unnecessary aggravation and harassment to the ophthalmologist
in different criminal medico legal and compensatory cases.
2.Introduction
3.Material And Method
4.Result
5.Discussion
6.Conclusion
7.References
Keywords
Ocular Trauma, Photography, Medico Legal Cases.
Introduction
Ocular trauma is a leading cause of visual morbidity world-wide. [1] It is associated with significant emotional stress as well as numerous emergency rooms and outpatient visits [2]. It accounts for about 50% of all eye fatalities admitted in developed countries. [3] The incidence of eye injuries may be higher in developing countries [4]. Despite the fact that the eyes represent only 0.27% of the total body surface area and 4% of the facial area, they are the third most common organ affected by injuries after the hands and feet.[5] Worldwide there are approximately 1.6 million people blind from eye injuries, 2.3 million bilaterally visually impaired and 19 million with unilateral visual loss; these facts make ocular trauma the most common cause of unilateral blindness.[1] Many eye injuries are related to particular occupations and certain cultures.[6]
The first Photography of the anterior segment of the eye was introduced by Drüner in 1900 [7]. The anterior segment of the eye is readily accessible for minute and delicate examination. Straightforward photography of the external eye is useful in maintaining a permanent record and in the assessment of small changes in lesion [7].Comprehensive knowledge of patient’s history and ocular examination is critical in the management of ocular injuries. Ocular imaging modalities add valuable information for the clinical and surgical care [8].
We want to highlight the significance of ocular photography since a picture carries a thousand words, to a through clinical examination for improving our understanding and methodology for managing ocular trauma. Aim of the study is to photograph different cases of ocular trauma for an ophthalmologist safety in giving prognosis after ocular trauma and avoiding problems which are faced in court of law in criminal medico legal cases.
Material And Method
This study was a hospital based, prospective and cross sectional descriptive study. It was conducted in the department of ophthalmology, Abbassi Shaheed Hospital, Karachi from July 2013 to March 2014. Patients were selected on basis of nonprobability consective sampling. Sample size was calculated [8] and total number of patients recruited was 100 to avoid type 2 error. Patients presenting in an eye OPD or admitted via emergency with ocular trauma were included in the study. Blunt trauma and penetrating injuries both were included in the study. Patients younger than 6 years of age, disoriented, comatose, immobile and not giving consent were excluded from the study. Minor injuries like bruises, corneal abrasions and corneal foreign bodies were excluded.
Detail history of every patient regarding trauma was taken. Nature of injury, object, duration and any first line treatments given were recorded. Visual acuity was evaluated using the Snellen’s chart for the literates and illiterate E chart for the illiterates. Anterior segment was examined with the help of slit lamp biomicroscope for sub conjunctival hemorrhages, corneal ulcers, corneal abcess, full thickness corneal, corneoscleral or scleral defects, hyphema, cells and flare in anterior chamber, iridodyalisis, cataract, lens subluxation, dislocation. Posterior segment was examined in cases of normal anterior segment with vision loss. Patients were informed about the study and only after written informed consent; photographs were taken on the day of presentation. Camera used for the study was Kowa Fx 50 R. Patients were asked to sit in front of the camera just like in front of slitlamp. Camera was held parallel to the frontal plane of the face and same horizontal level as the center of the face. Joystick was used for focusing and patient was asked to focus on a pointer for the shot required. After ensuring that the patient maintains this parallel position camera was clicked. Shifting from anterior segment to posterior segment was done by changing the lens power. Snaps were taken on two magnifications. Two to four photographs were obtained, allowing for selection of the best and rejection of substandard-quality and out-of-focus images. Necessary investigations like X -ray orbits, CT scan and B scan were requested where required for clinical correlation. Patients with blunt injuries were managed conservatively. Surgery was performed where necessary.
Data was then entered and analyzed on SPSS version 16.Mean age was calculated. Frequencies were calculated as percentage for gender, type of injuries, object of injuries, anterior segment and posterior segment signs.
Result
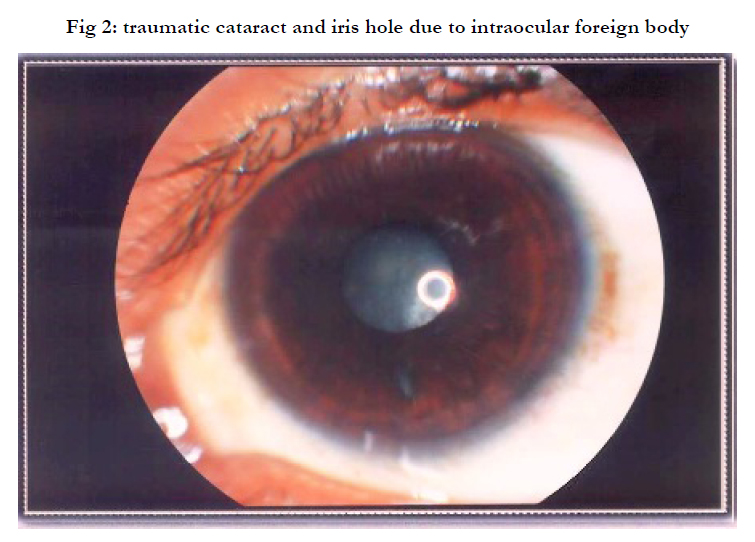
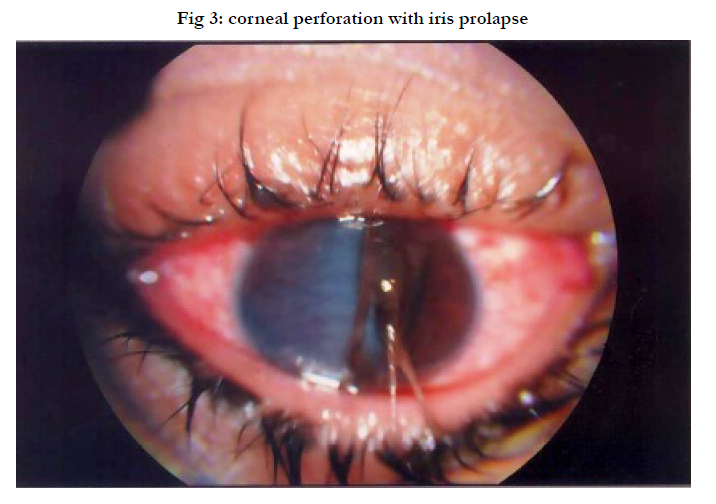
Among 100 patients (72%) were males and (28%) were females. The patients belonging to 6-15 years of age were [36%], between 16-40 years of age were [48%] and number of patients between 41-70 years of age were [16%]. Minimum age was 6 and maximum age was 83 years with mean age of???.Total numbers of cases photographed with close globe injury were (64%) and open globe injuries were (36%) (table 1) (fig 1). The common objects of injury were stone, metallic rod and wooden stick 14% (table2) (fig 2) each.
Different variety of injuries were photographed, lid cut 6%, subconjunctival hemorrhages 10%, corneal cut 28%, hyphema 10%, subluxated lens 4%, cataract 10%, traumatic aniridia 2%, Choroidal rupture 4%, Traumatic optic atrophy 2% and Commotio retinae 2% (table 3)(fig 3,4).
Discussion
Ocular photography and digital imaging are valuable practices that may assist in providing the best level of optometric care. They have application in clinical records, patient education, teaching and research, interoffice diagnostic opinions and community screening for diseases such as glaucoma and diabetic retinopathy [9,10].
Worldwide a lot of work has been done on ocular trauma but only few reported it with the help of photographs. The most common age group of our study representing trauma is 16-40 years of age which is 48%, with male preponderance. These results are comparable with results of other local [11,12]and international studies [13,14].Open globe injuries in our study are 64% and open globe injuries 36%.Close globe injuries are more common than open globe worldwide [14,15]. Open globe injuries were managed surgically.
Several technologies now exist for imaging anterior segment, including Optical Cohrence Topography (e.g. Visante, Carl Zeiss Meditec AG, Jena, Germany), scanning Scheimpflug (e.g. Pentacam, Oculus, Lynnwood, WA, USA), and scanning slit-lamp systems (e.g. Orbscan, Orbtek, Salt Lake City, UT, USA). Each method has its particular advantages and disadvantages. [16] Ultrasound Bio Microscopy has a valuable adjuvant role in identifying the presence of an underlying small foreign body not visible on slit lamp examination [17] and differentiating it from a nodular conjunctival mass [18]. Current imaging tools can monitor corneal wound healing, foreign body location, and if it is left in the cornea, foreign body migration [8]
Several Studies have established the validity and utility of fundus photography in the detection of ocular and systemic diseases in various non-Emergency Departments and research settings.[19] Few have recommended overcoming the inherent barriers to adequate ocular fundus examination through the use of teleophthalmology services in the care of Emergency Department patients. [20] Nonmydriatic fundus photography, has overcome many of the barriers to an adequate, routine funduscopic examination in the Emergency Department. Certainly, it is not only easier to look at a photograph than to visualize the ocular fundus with direct ophthalmoscopy, but the field of view is much larger with a nonmydriatic camera than with most direct ophthalmoscopes [21]. The use of nonmydriatic fundus photography is already gaining momentum for the screening of diabetic retinopathy in primary care settings. [22]
An examining ophthalmologist had to document the nature and extent of ocular injury carefully and accurately, including retinal photographs if possible. In court, it is the role of an ophthalmologist to be fair and balanced in the discussion of scientific evidence, and provide a reasoned explanation for his opinion, which can be understood by a lay audience [23].Ophthalmologist is a key contributor to the process required to make the diagnosis of inflicted traumatic brain injury (ITBI) precisely and on the basis of all the relevant evidence. Even though less than half of these cases proceed to a criminal trial [24].This is true not only for brain injuries but also for eye injuries in all medico legal cases. In our study it was easily accomplished with the help of ocular photographs which were taken at the time of trauma. These could also be used as evidence in cases where an ophthalmologist opinion is required for compensatory purposes.
Above discussed are diverse variations of ocular photography used for different purposes but it’s not being widely used in cases of ocular trauma. In visually dependent specialties like ophthalmology, clinical imaging is essential, especially, when evaluating ocular trauma. Images provide additional data to clinicians that may otherwise have not been known [8]. Preoperative and post-operative snapshots for penetrating injuries should also be captured and kept in records of the patient routinely rather than drawing and documenting. These should be easily retrievable for evidence in court. Last but not the least prognosis can be explained and guarded to the patient and their families on the basis of these photographs.
Limitation of our study is the model of the camera being used. Option of slit lamp photography was also not available in it to capture the depth of a corneal lesion, cells and flare in anterior segment. It cannot capture Relative Afferent Pupillary Defect (RAPD).
Conclusion
Ocular photography for clinical records, patient education, teaching and research, interoffice diagnostic opinions and community screening are all well-known advantages. Ocular photographs are the best evidence to be used in medico legal cases and compensatory purposes along with documentation and counselling. The new aspect to be highlighted is to photograph every case of an ocular trauma for the safety of an ophthalmologist and to explain grave prognosis to the family. This will avoid unnecessary aggravation and harassment to the ophthalmologist in different criminal medico legal and compensatory cases.
References
- Négrel AD, Thylefors B (1998) The global impact of eye injuries. Ophthalmic Epidemiol 5: 143-69.
- McGwin G, Owsley C (2005) Incidence of emergency department treated eye injury in the United States. Arch Ophthalmol 123: 662–666.
- Chiapella AP, Rosenthal AR (1985) One year in an eye casualty clinic. Br J Ophthalmol 69:865-70.
- Vats S, Murthy GVS, Chandra M, Gupta SK, Vashist P (2008) Epidemiological study of ocular trauma in an urban slum population in Delhi. Indian J Ophthalmol 56: 313–316.
- Nordber E (2000) Injuries as a public health problem in sub-Saharan Africa: Epidemiology and prospects for control. East Afr Med J 77:1-43.
- Mulugeta A, Bayu S (2001) Pattern of perforating ocular injuries at Manelik 11 hospital, Addis Ababa. Ethiop J Health Dev 15:131-137.
- Drüner L (1900) Ueber Mikrostereoskopie und eine neue vergrössernde Stereoskopcamera. Zeitsch Wiss Mikrosk 17:281-93
- Ryan DS, Sia RK, Colyer M, Stutzman RD (2013) Anterior Segment Imaging in Combat Ocular Trauma, JournalofOphthalmology.
- Yogesan K, Cuypers M, Barry CJ, Constable IJ, Jitskaia L (2000) Tele-ophthalmology screening for retinal and anterior segment diseases. J Telemed Telecare 6 (1):96-8s.
- Lee J (2003) Instrument Survey: O.D.s Add and Upgrade: O.D.s are investing in new instruments and harnessing office technology to improve diagnosis and disease management. Rev Optom 140:8.
- Jahangir T, Butt N H, Hamza U (2011) Pattern of Presentation and Factors Leading to Ocular Trauma. Pak J Ophthalmol 27 (2).
- Babar TF, Khan MN, Jan S (2007) Frequency and causes of bilateral ocular trauma. JCPSP 17: 679-82.
- Wong TY, Tielsch JM (1999) A population-based study on the incidence of severe ocular trauma in Singapore. Am J Ophthalmol 128: 345-51
- Khatry SK, Lewis AE, Schein OD (2004) The epidemiology of ocular trauma in rural Nepal. Br J Ophthalmol 88: 456-60.
- M Soylu, S Sizmaz, S Cayli (2010) Eye injury in southern Turkey: epidemiology, ocular survival, and visual outcome. International Ophthalmology April 30(2):143-148
- Nolan W (2008) Anterior segment imaging: ultrasound biomicroscopy and anterior segment optical coherence tomography. Curr Opin Ophthalmol 19:115–21.
- Deramo VA, Shah GK, Baumal CR (1998) The role of ultrasound biomicroscopy in ocular trauma. Tr Am Ophth Soc 96:355–367.
- Taherian K, MacKenzie JM, Atta HR (2002) Ultrasound biomicroscopy: fisherman’s tale. Br J Ophthalmol 86:1445.
- Wong TY, Klein R, Couper DJ (2001) Retinal microvascular abnormalities and incident stroke: the Atherosclerosis Risk in Communities Study. Lancet 358:1134–40.
- Kulshrestha M, Lewis D, Williams C, Axford A (2010) A pilot trial of teleophthalmology services in north Wales. J Telemed Telecare 16:196–7.
- Bruce BB, Lamirel C, Biousse V, Ward A, Heilpern KL, et al. (2011) Feasibility of Nonmydriatic Ocular Fundus Photography in the Emergency Department: Phase I of the FOTO-ED Study. Academic Emergency Medicine 18: 928–933.
- Chabouis A, Berdugo M, Meas T (2009) Benefits of Ophdiat, a telemedical network to screen for diabetic retinopathy: a retrospective study in five reference hospital centres. Diabetes Metab 35:228–32.
- Vincent AL, Kelly P (2010) Retinal haemorrhages in inflicted traumatic brain injury: the ophthalmologist in court. Clinical & Experimental Ophthalmology 38: 521–532.
- Kelly P, MacCormick J, Strange R (2009) Non-accidental head injury in New Zealand: the outcome of referral to statutory authorities.Child Abuse Negl 33: 393–502.