Amblyopia In Children 3-9 Years Old, With Refractive Anomalies During 2010-2011 In Prishtina
Shoshi MH1*, Shoshi A2, Agim X3, Fitore S4, Fjolla S5, Flaka S6
1 Eye Clinic University Clinical Center of Kosova, Kosova
2 Shoshi Polyclinic, Kosova
3 Eye Clinic University Clinical Center of Kosova, Kosova
4 University of Prishtina, Faculty of Medicine, Kosova
5 University of Prishtina, Faculty of Medicine, Kosova
*Corresponding Author
Mire Hoxha-Shoshi,
Eye Clinic University Clinical Center of Kosova,Kosova
Tel/ Fax: +37744240739
E-mail: mireshoshi@hotmail.com
Article Type: Research Article
Received: July 3, 2014; Accepted: July 23, 2014; Published: July 26, 2014
Citation: Shoshi MH,et al. (2014). Amblyopia In Children 3-9 Years Old, With Refractive Anomalies During 2010-2011 In Prishtina, Int J Ophthalmol Eye Res, 2(4), 39-48. doi: dx.doi.org/10.19070/2332-290X-1400010
Copyright: Shoshi MH© 2014. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Vision screening in schools has a long history, the reason of which was and continues to be, the treatment of refractive anomalies. Early detection of vision problems has many advantages in education and in everyday life.
Aim of the study: The screening of the refractive anomalies in pre-school and school age children (3-9 years), in the city of Pristina
aimed the determination of the prevalence of refractive anomalies.
Materials and method: This is a transversal project – cross sectional, which has been conducted during 2010-2011. For the data collection
we have designed a special questionnaire/form. We have selected the city of Prishtina for this work, Since the study was a zonal
type of study, we have selected the city of Prishtina for this work. Our research included 1027 children of age 3-9 years old.
Results: The prevalence of the eye refractive anomalies in children of age 3-9 years old results to be 11.7%, with variability from 9.7%
to 13.7%, for 95% accuracy. In children of age 3-9 years old, myopia was encountered in 3.4% (or 34/103) of the cases , with variations
from 2.3% up to 4.5%; hyperopia was found in 3.8% with variations from 2.6% up to 5.0%; astigmatism in 4.5%, with variations from
3.2% up to 5.8%, without significant differences based on age or gender.
Conclusions: After a thorough analysis of the results, we came to the conclusion that screening of the refractive anomalies in children
of age 3-9 years old is very important since their prevalence is apparent.
2.Background
3.The Aim of The Study
4.Materials and Working Methodology
4.1.The way of obtaining the data of the study
4.2.Statistical data processing
5.Results
6.Discussion
7.Conclusions
8.Conflict of Interest
9.References
Keywords
Screening, Refractive Anomalies, Children 3-9 Years Old, Prishtina.
Background
Due to their biological and social characteristics, school age children make up a special group of population therefore they require special health care.[1] The health of the children is a strong indicator of the general health condition of the population.[2] The basic biological characteristic of the school children is their growth and development. Therefore, the care for child health includes, as a main pillar, the care towards their growth and psychophysic development and as such composes one of the main tasks and priority obligations of health.[3].
Refractive anomalies are the main factors that cause many visual disorders, blindness and a high rate of poor visual acuity all over the world.
[4] School children are considered as the most endangered group because the untreated refractive anomalies can seriously affect their learning ability and their physical and mental development. Studies in many countries of the world related to the prevalence of the refractive anomalies have shown significant differences.[7-23] Studies based on population regarding the prevalence of the refractive anomalies in Kosovo are limited.
The Aim of The Study
The screening of eye refractive anomalies in children of preschool and school age (3-9 years old), in the city of Prishtina, aimed the following:
• Identification of the most common refractive anomalies at this age of childhood.
• Determination of the prevalence of the refractive anomalies.
• Determination of pathology-specific prevalence compared to the group ages considered in the study.
• Treatment of these refractive anomalies and evaluation of the close and distant results after the treatment by our methods.
• Comparison of the found prevalence and the prevalence in the world.
• Influence of socio-economic factors in the prevalence of amblyopia and strabismus.
• The influence of heredity in these refractive anomalies
Materials and Working Methodology
This work is transversal – cross sectional, and has been completed during 2010-2011. For the data collection, a special questionnaire/ form was designed by the author of this work. This form contains general data of the child and the most important parameters of their ocular health. The refractive anomalies are the dependent variables, while as non-dependent variables are a series of factors influencing the discovery of these refractive anomalies such as : heredity, medical culture and socio-economic status of the parents, the lack of visible signs, early age of children, conditions of ophthalmological services in this area, etc. In our study, we selected the city of Prishtina, since the study was a zonal type of study, consisting of the presentation of the situation in the refractive anomalies in children of age 3-9. This type of study was the first one conducted in Prishtina until now. The subject of this study are preschool and school children from 3-9 years old. This was the group age that allowed a complete and accurate examination, with higher treatment possibilities.
The selection of 1027 children includes subjects of every age between 3 and 9 years old:
3 years old: 142 children
4 years old: 151 children
5 years old: 169 children
6 years old: 196 children
7 years old: 131 children
8 years old: 115 children
9 years old: 123 children
TOTAL: 1027 children
The way of obtaining data for our study was based in two stages: First stage: consisted of data collection from the questionnaire that was distributed earlier (these are subjective data), as well as the data collected from clinical examination in above mentioned classes, representing objective data.
The tools used in the first stage were very simple. This examination consisted of a table with the letter “E”, a table that was set in a distance of 5 meters from the child to be examined, occluder, nurse, teacher and the ophthalmologist (the examiner).
The measurement of the visual acuity was done in a 5 meter distance correctly measured in the classroom, with sufficient lightening allowing the clear vision of the table. The nurse would stand by the child, closing of his eye with occluder, while the ophthalmologist would stand by the side of the table facing natural light and pointing the lines of the table.
Every child was individually examined in front of the table, without the presence of other children, this being an important moment determined by us, in avoiding the so called bias phenomena of information.
All the data collected from clinical examination, like: visual acuity, eye movement, pupillary reflex, covering method for close and far positions, together with the subjective data, were registered for every child in individual folders.
Stage two: consisted of data collected from the questionnaire and the clinical examination in the ophthalmology department, registered in a special field prepared by our side and approved by the Ophthalmology Department of the UCCK, for all the children with the decreased vision under 1.0 that resulted abnormal in the first stage of study.
We checked the eye movement close and far, and also the binocular vision (titmus stereo) was determined. The red reflex was checked, whether it was normal, abnormal, or asymmetrical. We used cycloplegic examination with cyclogyl (cyclopentolate hydrochlorid 1%) two drops for each eye, and after 5 minutes the drops were repeated. After 20-30 minutes, skiascopy was done and retinal examination directly with ophthalmoscope. Two days later the refraction examination was repeated.
In the majority of cases, children were sent in UCCK to repeat the examination, where a second skiascopy was done. All the data were compared using refraction which gave a better visual acuity, lowering to the maximum the refractive error in prescribing lenses to the subjects with refractory pathology.
The data were processed with statistical package SPSS 12.0, and the results are presented by tables and graphs. Out of statistical parameters, we have calculated structural index, arithmetic mean, standard deviation, minimal and maximal values.
For the verification of the statistical importance of the differences between parameters at the parametric data, we have done the T-test, while to test the differences between non- parametric data, we have used T-test of proportion (value – Z), X2-test and Fisher’s test. Verification of tests was done for the confidence level for p<0.05 and p<0.01.
Every prevalence value (p) obtained underwent the statistical test “Z” (with Yates correlation), based on the following formula:
Zc= ( | P – Pe | - 1/2 n ) / Se (P)
Where : Se (P) = √ (P ( 1-P) / n)
(P – our prevalence; Pre-expected prevalence; n- number of selection) for determination of the gained results, α or p, means for determination or not of statistical significanceResults
This study included 1027 children of the age 3-9 years old, out of which 536 or 52.2% were boys, and 491 or 47.8% were girls. With the X2 test we have not obtained important significant difference in the number of the children involved in screening based on gender (X2-test=1.97, SHL=1, P=0.16 therefore, P>0.05).
Based on age, we had a higher participation of the 6 year-old children (19.1%) , compared to other ages. With the distribution of the data based on age and gender, we have gained a similar structure. Average age of the children included in the screening was 6.25 years old (SD±1.9 years). Average age of boys included in screening was 6.2 years old (SD±1.9 years), while girls was 6.3 years (SD ±1.8 years). With T-test of average, we did not obtain important significant statistical difference between the average age of boys and girls included in screening (T=0.86, P=0.387).
Out of the total number of children involved in screening (n=1027) 168 or 16.4% were with refractive anomalies. Based on age, the prevalence of the refractive anomalies is 9.9% in children of the age 3 and 21.4% in children of the age 7. In the second visit were foreseen 168 children, but only 138 or 82.1% of the children came. The number of the examined children during the second visit based on age and gender is presented on the Table 1. Out of 138 children, 77 or 55.8% were boys and 61 or 45.2% girls. With X2-test we did not gain significant statistical difference in the number of children included in screening based on gender (X2-test=1.92, SHL=1, P=0.217 therefore, P>0.05).
Based on gender, most children were of age 6 (23.2%) and 7 years (16.7%).
With the distribution of children by age and gender, we have retrieved a similar structure. Average age of children foreseen for the second visit was 6/0 years old (SD±1.8 years). Average age of boys included in the screening was 6.1 years (SD±1.9 years), while the age of the girls included in the screening was 6.0 years (SD±1.7 years). With T-test of average we did not have any difference with significant statistical importance between the average age of boys and girls. The second stage of examination was based on the individual file (detailed research of subjects that resulted with visual abnormalities in the first stage of the study). This individual file was more detailed since every child that came to the department was accompanied by the parents, we also obtained the family anamnesis on refractive anomalies and earlier examinations results. The visual accuracy was measured with the occluder with and without hole, papillary reflex, eye movement close and far, titmus stereo, examination of retina with ophthalmoscope (fundos ovuli), skiascopy for every child , and at the end we would repeat viewing with refraction. See the schedule below.
Out of 138 examined children in the second visit, 114 children resulted with refractive anomalies, 4 with eye pathologies and 20 did not have neither refractive anomalies nor eye pathologies. Out of 114 cases with refractive anomalies, 33 cases (3.4%) belonged to Myopia, 37 cases (3.8%) Hyperopia and 44 cases (4.5%) belonged to astigmatism. Levels of myopia from 3.4% (or 34/103), of hyperopia from 3.8% (or 38/103 ), and astigmatism from 4.5% (45/103) are statistically significant (P<0.0001), therefore we can do their generalization for all children of age 3-9 years. At the end, it results that in the children of ages 3-9 myopia is encountered in 34/3 (95%CI 23/103 up to 45/103); hyperopia in 38/3 (95%CI 26/103 up to 50/103); astigmatism 45/103 (95%CI 32/103 up to 58/103).
All the cases with visual acuity less than normal (118 cases) have undergone this treatment: lenses in all cases, accompanied with healthy eye occlusion therapy for 4 weeks. Visual acuity before the treatment is separated in four stages:
1. Profound Amblyopia (visual acuity<0.1);
2. Medium Amblyopia (visual acuity 0,1 – 0,3);
3.Light Amblyopia (visual acuity 0,4 – 0,8) and
4. No Amblyopia (visual acuity >0,8).
Out of 236 examined eyes, in half of them (50%) visual acuity was above 0.8 (meaning without amblyopia), in 87 or 36.9% was 0.4-0.8, then in 25 or 10.6% was 0.1-0.3 and in 6 or 2.5% was under 0.1. with the distribution of cases based on visual sharpness and eyes, we have achieved a similar structure (Table 2). After the treatment (lenses and occlusion) out of 236 examined eyes, in 204 or 86.4% visual sharpness was above 0.8, in 24 or 10.2% was 0.4-0.8, then in 6 or 2.5% was 0.1-0.3 and in 2 or 0.8% was under 0.1. With the distribution of cases based on visual sharpness and eyes, we have achieved similar (Table 3).
After the treatment, we had improvement of visual sharpnesswith significant difference (X2=72.3m SHL=2, P<0.0001), (Graph.1) Therefore, compared with 50% of the eyes without amblyopia before the treatment, after the treatment we had 86.4% of nonamblyopic eyes.
Graph 1. Comparison of visual sharpness in children with refractional anomalies before and after treatment.
Before the treatment, Myopia caused amblyopia in 24 eyes, or 36.4% of the myopic eyes. Hyperopia gave amblyopia in 43 eyes, or 58.1% of hyperopic eyes. Astigmatism gave amblyopia in 43 eyes, or 48.9% of astigmatic eyes. Non refractory pathologies in all cases were accompanied by amblyopia. After the treatment, Myopia gave amblyopia in 7 eyes or 10.6% of the myopic eyes. Hyperopia resulted with amblyopia in 12 eyes or 16.2% of hyperopic eyes. Astigmatism gave amblyopia in 13 eyes or 14.8% of astigmatic eyes. Non refractory pathologies after the treatment gave amblyopia in 4 eyes, or 50.0% of the eyes with non refractory pathologies. The percentage of subjects with amblyopia after the treatment is significantly lowered (Graph. 2).
As we can see from the table 4, before the treatment amblyopia resulted in 7 eyes or 70.0% of the eyes of persons with myopic astigmatism combined with myopic components. The common myopic astigmatism gives amblyopia in 15 eyes, or 57.7% of eyes with this pathology. Common hyperopic astigmatism gives amblyopia in 16 eyes or 53.3% of eyes of 13 persons with this pathology. Hyperopic astigmatism combined with myopic components gives amblyopia in 2 eyes or 50% of eyes of 2 persons with this pathology. Myopic astigmatism combined with hyperopic components gives amblyopia2 eyes or 50% of eyes of 2 persons with this pathology. Hyperopic astigmatism combined with hyperopic component gives amblyopia in 6 eyes or 42.9% of seven persons with this pathology.
As it can be seen from the table 5, after the treatment, hyperopic astigmatism combined with myopic component gives amblyopia in 1 eye or 25% of eyes of subjects with this pathology. Hyperopic astigmatism combined with hyperopic component gives amblyopia in 2 eyes, or 14.3% of the eyes of 7 subjects with this pathology. Common myopic astigmatism gives amblyopia in 1 eye or 3.8% of eyes with this pathology. Common hyperopic astigmatism gives amblyopia in 1 eye, or 3,3% of eyes of 15 subjects with this pathology. The two other forms of astigmatism, after treatment, did not give any amblyopia. As we can see from the (graph 3), amblyopia in all forms of astigmatism has been reduced after treatment. Before the treatment, prevalence of amblyopia was found in 6.0%: ( P = 118/1954 = 6.0% ) in the total number of our cases (95% CI 46/103 up to 66/103).
Graph 3. Percentage of subjects with amblyopia before and after treatment based on types of astigmatism
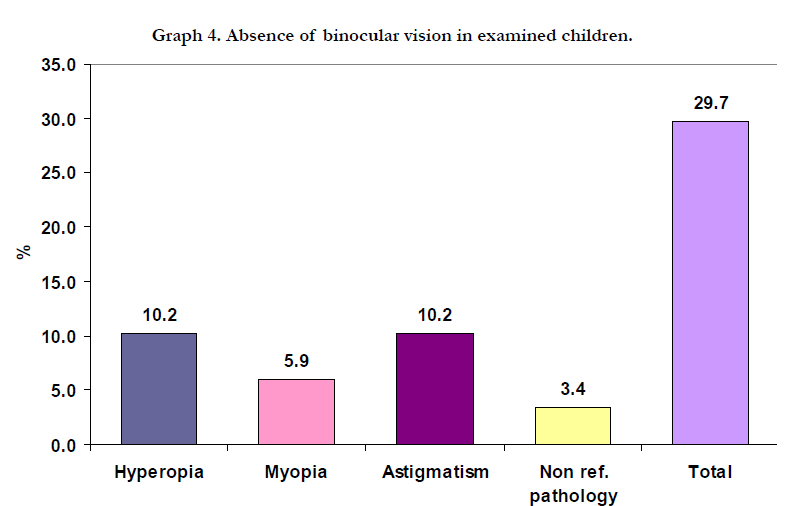
After the treatment with lenses and occlusion, the prevalence of amblyopia resulted in 36 eyes ( P = 36/1954 = 1.8% ) with variations 11/103 in 22/103 for 95% CI. Out of 118 children involved in research with eye pathology, 114 or 96.6% were with refractory pathology, and 4 or 3,4% with non refractory pathology. Out of four cases with non refractory pathologies, 2 cases or 1.7% were with congenital strabismus, one or 0.8% was with unspecified retinal pathology, and one or 0.8% was in a stage after Arteria hyolidea persistens Esotropia sec. Out of refractory anomalies, the most common one was Astigmatism, with 44 cases or 37.3%, Hyperopia with 37 cases or 31.4%, Myopia with 33 cases or 28.0% (Graph 4).
The presence and absence of binocular view in our subjects with eye pathology, based on the type of pathology is presented in table 9. Out of 4 cases with non refractive anomalies, in all of them we had the absence of binocular view. From refractive anomalies the absence of the binocular view was the highest in Hyperopia with 32.4%, then Astigmatism with 27.3% and Myopia with 21.2%.
From our study, it resulted also the deviation in 80 eyes of the subjects with a prevalence level in the whole contingent taken for study (1027-50=977 subjects) from 4.1% (P=80/1954 = 4.1%), meaning that deviations in children age 3-9 years old are encountered with a prevalence of 41/3 with variations from 35/3 in 47/3 for 95% accuracy. Out of 118 cases with refractive anomalies, 55 or 46.6% of subjects were with strabismus, and 63 or 53.4% without it. (Table 6).
Out of 44 subjects with astigmatism, 14 of them resulted with deviation or 11.9% of the total number of children with refractive anomalies. Out of 30 subjects with myopia, 8 of them resulted with deviation, 6.8% of the total number of children with the refractive pathologies. Out of 37 subjects with hyperopia, 30 of them resulted with deviation, or 25.4% of the total number of children with refractive anomalies. Astigmatism accompanied by strabismus was encountered in 11.9% of cases. Myopia accompanied by strabismus in 6.8%, Hyperopia with strabismus in 25.4%, congenital strabismus and amblyopia in 1.7%, and unspecified retinal pathology in 0.8% (Table 6). Cases with astigmatism and Myopia have been less accompanied with strabismus.
The report of the subjects with strabismus and those without strabismus in refractory anomalies was: Myopia 1: 3 :1 ; Hyperopia 4.3 : 1 ; Astigmatism 1 : 2.1.
Out of totally 66 eyes of subjects with Myopia, we had 57 or 86.4% of eyes without deviation and 9 eyes or 13.6% with deviation where 5 or 7.6% were Exo-deviation and 4 or 6.0% were Esodeviation (Table 7).
Out of 74 eyes of 37 subjects with Hyperopia, we encountered 41 or 55.4% of eyes without deviation and 33 eyes or 44.6% with deviation where 4 or 5.4% were Exodeviation and 29 or 39.2% were Esodeviation (Table 8).
Out of totally 88 eyes of 44 subjects with astigmatism we had 74 or 84.1% of eyes without deviation and 14 eyes or 15.9% with deviation where 3 or 3.4% were Exodeviation and 11 or 12.5% were Esodeviation (Table 9).
Out of 8 eyes of 4 subjects with non refractory pathology, we had 4 or 50% of eyes without deviation and 4 eyes or 50%with deviation where 1 or 12.5% were Exodeviation and 3 or 37.5% were Esodeviation.
More than half of pathologies, 52.5% were not examined before. Out of 33 cases with Myopia, 18 or 54.5% were examined for the first time during screening, and out of 37 cases with Hyperopia 20 or 54.1%, and from 44 cases with astigmatism 24 or 54.5% were examined for the first time during screening. Meanwhile, out of four cases with non refractory anomalies, all of them were examined earlier (Table 10). 67% of children with refractory pathology had genetic predispositions (Table 12).
Table 10. Subjects with respective pathology examined before the start of the study and those examined for the first time.
Discussion
Refractive anomalies, in particular myopia is one of the five causes of visual acuity disorders all over the world. [24] It is considered that by year 2020, around 1/3 (2.5 billion) of population will be affected from myopia. [25] Prevalence of the refractive anomalies, particularly in children 6-7 years old has been evaluated in a limited number of studies based on population.
Pediatric studies that explore the eye pathologies have provided important clues to the early development of refractory anomalies.[26-28] Studies in Australia and new zealand have shown that the prevalence of myopia in children 8 years old or younger is low (5%). [29-31] However, comparing to Australia and new zealand, studies in some Asiatic countries have shown a much higher prevalence of myopia. A study in Taiwan including 10000 school children showed a prevalence of myopia of 6% in 6 years old children. [37]In a research by Chung and coworkers [32] the prevalence of myopia in Chinese students between 6-12 years old was 37.0% and 50.0% in students between 13-18 years old. In the suburb Ibipora in Brazil during 1989-1996, 13471 or 14.59% of the children were referred for an ophthalmic examination. [33] We have not observed any increase on the prevalence of the refractive myopia accordingly with the age. However, data published by a research based on population that was conducted in Singapore with children and teenagers, has shown that the prevalence of myopia has increased from 29% in the age of 7 to 35% in the age of 8 and to 43% in the age of 9.
[35]Another research conducted in Singapore including 3009 children of the age 3-6 years old, showed that the prevalence of myopia was approximately 15% ( at least -50D). In the 3 years old children the prevalence was 6.4% and in 6 years old children 8.6 %. Prevalence of hyperopia in children with at least 3.00 D was 1.35% and the prevalence increases at 7.8% in children with at least 2.00D. [35] In these children the change in the prevalence of myopia, hyperopia and astigmatism based on gender was not significant.[34]In a research by Sounouvou and coauthors (92) including 1057 school children from Benin, France from 4 to 16 years old showed that the prevalence of the refractive pathologies was 10.6%. The most frequent refractive anomaly was astigmatism (91.9%).Myopia was associated with astigmatism in 29.4% of the cases, while hyperopia was associated with astigmatism in 16.1% of the cases.No corelation was noticed between the refractive anomalies, age and gender.
In a research that was conducted in Shiraz, Iran [36] and included 1872 school children, the prevalence of myopia (at least -50D) was 4.35%,(95% CI 2.89% - 5.82%),of hyperopia (≥+2.0 D ) was 5.04% (95%CI 3.5% - 6.58%) and of astigmatism (≥ 0.75 D) was 11.27% (95%CI 9.81%-12.74%).
In our study, for the first time in the city of Prishtina- Kosova, were studied the refractive anomalies in children 3-9 years old.For our study we have chosen the subsectional type, that is a prevalence study.Through this study we have studied some indexes and indicators such as: visual abnormalities, eye pathologies in group, myopia,hyperopia,astigmatism,amblyopia and deviations. Therefore after the second visit the prevalence of the eye grouppathologies in children 3-9 years old is 11.8% (118/103) with fluctuations from 9.8% ( 98/103) to 13.8% ( 138/103)and with a certainty of 95%. While, the prevalence of eye refractive-group anomalies in children 3-9 years old, results in 11.7% (117/103) with fluctuations from 9.7% (97/103) to 13.7% ( 137/103) with a certainty of 95%. In children 3-9 years old myopia is encountered in 3.4% of the cases with fluctuations from 2.3% ( 23/103) to 4.5% (45/103); hyperopia in 3.8% (apo 38/103) with fluctuations from 2.6% (26/3) to 5.0% (50/3); astigmatism in 4.5% (45/3) with fluctuations 3.2% (32/3) to 5.8% (58/3) with no significant changes according to age and gender.This level of the prevalence of the visual abnormality is high but can be compared studies form authors Leonard and Nelson, in a prevalence level of 15.2 % and Tonuzi in a prevalence level of 18.2%. Results of our study are similar to the results of the study of the eye pathologies in Dibra, Albania by the author Ali Tonuzi. [37].
Conclusions
1. 1027 children were studied; age 3-9, from the city of Prishtina, randomly selected during 2010-2011.
2. Prevalence in encountering of group pathologies of eye in children age 3-9 was 11.8% (or 118/3) with variations from 9.8% (or 98/3) up to 13.8% (or 138/3).
3. Prevalence of eye pathologies group refractory in children age 3-9 results to be 11.7% or 117/3 with variations from 97/3 in 137/3 for 95% accuracy.
4. Prevalence of Myopia resulted in 3.4% or 34/3 varying from 23/3 up to 45/3 for 95% CI in the whole population of the group age 3-9 years old.
5. Prevalence of Hyperopia resulted in 3.8% or 38/3 varying from 26/3 up to 50/3 for 95% CI in the whole population of the group age 3-9 years old.
6. Prevalence of astigmatism resulted in 4.5% or 45/3 varying from 32/3 up to 58/3 for 95% CI in the whole population of 3-9.
7. Prevalence of Amblyopia before the treatment resulted with prevalence 6.0% varying from 46/3 up to 66/3 for 95% CI and after treatment resulted with 1.8% with variation 11/3 in 22/3 for 95% CI.
8. Deviations in children’s age 3-9 are encountered with a prevalence of 4.1% or 41/3 with variations from 35/3 in 47/3 for 95% accuracy.
9. Children with ocular pathology discovered for the first time from our screening, resulted in 52.5%, while 47.5% were examined earlier.
10. Hereditary data had 67% of children with refractory pathology.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- American Association for Pediatric Ophthalmology and Strabismus (AAPOS) (2001) Policy statement: Vision screening for infants and children. San Francisco, CA: American Academy of Ophthalmology.
- Pizzarello L, Tilp M, Tiezzi L, Vaughan R, McCarthy J (1998) A schoolbased program to provide eyeglasses: Childsight. Journal of the American Association for Pediatric Ophthalmology and Strabismus 2(6):372-374.
- Proctor S. E (2005) To see or not to see: Screening the vision of children in school. Castle Rock, CO: National Association of School Nurses.
- Dandona R, Dandona L (2001) Refractive error blindness. Bull World Health Organ 79:237–43.
- Lutaj P (1998) Oftalmologjia. Tiranë 51-55; 57-63.
- Negrel AD, Maul E, Pokharel GP (2000) Refractive error study in children: sampling and measurement methods for a multi-country survey. Am J Ophthalmol 129:421–6.
- Gilbert C, Foster A (2001) Childhood blindness in the context of VISION 2020—the right to sight. Bull World Health Organ 79:227–32.
- Zhao J, Pan X, Sui R (2000) Refractive error study in children. Am J Opthalmol 129:427–35.
- Pokharel GP, Negrel AD, Munoz SR (2000) Refractive error study in children. Am J Ophthalmol 129:436–44.
- Maul E, Barroso S, Munoz SR (2000) Refractive error study in children. Am J Ophthalmol 29:445–54.
- Dandona R, Dandona L, Srinivas M (2002) Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci 43:615–22.
- Murthy GV, Gupta SK, Ellwein LB (2002) Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci 43:623–31.
- Naidoo KS, Raghunandan A, Mashige KP (2003) Refractive Error and Visual Impairment in African Children in South Africa. Invest Ophthalmol Vis Sci 44:3764–70.
- He M, Zeng J, Liu Y, Xu J (2004) Refractive error and visual impairment in urban children in southern China. Invest Ophthalmol Vis Sci 45:793–9.
- Goh P, Abqariyah Y, Pokharel GP (2005) Refractive Error and Visual Impairment in School-Age Children . Ophthalmology 112:678–85.
- Junghans BM, Crewther SG (2003) Prevalence of myopia among primary school children. Clin Exp Optom 86:339–45.
- Wedner SH, Ross DA, Todd J (2002) Myopia in secondary school students the need for a national screening programme. Br J Ophthalmol 86:1200–6.
- Lithander J (1999) Prevalence of myopia in school children in the Sultanate of Oman: a nation-wide study of 6292 randomly selected children. Acta Ophthalmol Scand 77:306–9.
- Khandekar RB, Abdu-Helmi S (2004) Magnitude and determinants of refractive error in Omani school children. Saudi Med J 25:1388–93.
- Lin LLK, Shih YF, Hsiao CK (2004) Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singapore 33:27–33.
- Villarreal MG, Ohlsson J, Abrahamsson M (2000) Myopisation: the refractive tendency in teenagers. Prevalence of myopia among young teenagers in Sweden. Acta Ophthalmol Scand 78:177–81.
- Mavracanas TA, Mandalos A, Peios D (2000) Prevalence of myopia in a sample of Greek students. Acta Ophthalmol Scand 78:656–9. [23] Robaei D, Rose K, Ojaimi E (2005) Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology 112:1275–82.
- Pararajasegaram R (1999) VISION 2020-the right to sight: from strategies to action. Am J Ophthalmol 128(3):357–358.
- Kempen JH, Mitchell P, Lee KE, Tielsch JM (2004) The prevalence of refractive errors among adults in the United States, Western Europe, and Australia.Arch Ophthalmol 122(4):495–505.
- Gwiazda J, Scheiman M, Mohindra I, Held R (1984) Astigmatism in children: changes in axis and amount from birth to six years. Invest Ophthalmol Vis Sci 25:88–92.
- Howland HC, Sayles N (1984) Photorefractive measurements of astigmatism in infants and young children. Invest Ophthalmol Vis Sci 25:93–102.
- Dobson V, Fulton AB, Sebris SL (1984) Cycloplegic refractions of infants and young children: the axis of astigmatism. Invest Ophthalmol Vis Sci 25:83–87.
- Mayer L, Hansen RM, Moore BD, Kim S, Fulton AB (2001) Cycloplegic refractions in healthy children aged 1 through 48 months. Arch Ophthalmol 119:1625–1628.
- Young FA, Beattie RJ, Newby FJ, Swindal MT (1954) The Pullman Study:a visual survey of Pullman schoolchildren. Part II. Am J Optom 31:192–203.
- Junghans BM, Crewther SG (2003) Prevalence of myopia among primary school children in eastern Sydney. Clin Exp Optom 86(5):339–345.
- Chung KM, Mohidin N, Yeow PT, Tan LL, O'Leary D (1996) Prevalence of visual disorders in Chinese schoolchildren. Optom Vis Sci. 73(11):695-700.
- Heukelbach J, Wilcke T, Winter B, Feldmeier H (2005) Epidemiology and morbidity of scabies and pediculosis capitis in resource-poor communities in Brazil. Br J Dermatol 153(1):150-6.
- Saw SM, Hong CY, Chia KS, Stone RA, Tan D (2001) Nearwork and myopia in young children. Lancet 357(9253):390.
- Dirani M, Chan H, Gazzard G (2010) Prevalence of Refractive Error in Singaporean Chinese Children: The Strabismus, Amblyopia, and Refractive Error in Young Singaporean Children (STARS) Study. Investigative Ophthalmology & Visual Science 51(3):1348-55.
- Yekta A, Fotouhi A, Hashemi H, Dehghani C, Ostadimoghaddam H (2010) Prevalence of refractive errors among schoolchildren. Clin Experiment Ophthalmol. 38(3):242-8.
- Tonuzi A (2001) Depistimi i patologjive të syve në fëmijët e moshave parashkollore dhe shkollore (3-9 vjec) ne rrethin e Dibrës. Punim doktorature, Tirane.