Effectiveness Of Verbal, Verbal-Written and Video Instructions on Gingival Health of Patients with Fixed Appliances
Cheong Joo Ming1*, Norul Madihah M. Ashaari2, Razan Hayani Mohamad Yusoff2, Siti Marponga Tolos3
1 Department of Orthodontics, Kulliyyah of Dentistry, International Islamic University Malaysia, Jalan Sultan Ahmad Shah, Bandar Indera Mahkota, 25200 Kuantan, Pahang, Malaysia.
2 Kulliyyah of Dentistry, International Islamic University Malaysia, Jalan Sultan Ahmad Shah, Bandar Indera Mahkota, 25200 Kuantan, Pahang, Malaysia.
3 Department of Computational and Theoretical Sciences, Kulliyyah of Science, International Islamic University Malaysia, Jalan Sultan Ahmad Shah, Bandar Indera Mahkota, 25200 Kuantan, Pahang, Malaysia.
*Corresponding Author
Cheong Joo Ming,
Department of Orthodontics, Kulliyyah of Dentistry, International Islamic University Malaysia, Jalan Sultan Ahmad Shah, Bandar Indera Mahkota, 25200 Kuantan, Pahang,
Malaysia.
Tel: +609 5705484
Fax: +609 5705580
E-mail: alvinjooming@iium.edu.my
Received: February 09, 2022; Accepted: April 18, 2022; Published: April 21, 2022
Citation: Cheong Joo Ming, Norul Madihah M. Ashaari, Razan Hayani Mohamad Yusoff, Siti Marponga Tolos. Effectiveness Of Verbal, Verbal-Written and Video Instructions on Gingival Health of Patients with Fixed Appliances. Int J Dentistry Oral Sci. 2022;9(4):5282-5287. doi: dx.doi.org/10.19070/2377-8075-220001058
Copyright: Cheong Joo Ming©2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Orthodontic treatment causes detrimental effects on periodontal health due to the accumulation of dental
plaque. This problem can be prevented by implementing effective oral hygiene instructions (OHI).
Aim: Tocompare the effectiveness between verbal, verbal-written and video methods of OHI on the gingival health of patients
with fixed appliances. The best method in providing OHI to patients wearing fixed appliances was also assessed.
Materials and Methods: 39 patients with a mean age of 16.9 wearing upper and lower fixed appliances were divided into
three OHI groups (verbal, verbal-written and video) with five minutes standardized time allocation for each technique. Gingival
health was assessed using plaque index (PI), gingival index (GI), and bleeding on probing (BOP). The mean percentage
difference between pre- and post-OHI was calculated and analysed after 6 weeks. Data were analyzed using paired sample
t-test and one-way ANOVA.
Results: All periodontal parameters showed a reduction in their mean % in all OHI groups after 6 weeks, with significant decrease
in verbal-written and video groups (p<0.05). Verbal group showed significant reduction for PI after 6 weeks (p=0.012).
Overall, there was no significant difference between the effectiveness of the three OHI groups in the mean % reduction of
PI, GI and BOP.
Conclusions: Whilst verbal method was effective in improving the PI, verbal-written and video methods were effective in
improving all aspects of gingival health (PI, GI and BOP) in patients wearing fixed appliances. However, there was no single
best method in delivering OHI to patients with fixed appliances.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Oral Hygiene; Orthodontic Appliances; Gingival Diseases.
Introduction
A significant increase in the demand of orthodontic treatment
can be seen in recent years due to the growing concern of dental
and smile aesthetics.[1] Although orthodontic treatment improves
dento-facial appearance, it may cause regression of periodontal
health by enhancing the colonization of microorganisms and dental
plaque accumulation. Klukowska et al [2] found that the plaque
coverage in orthodontic patients was two to three times higher
than the levels observed in high plaque-forming adults without
appliances, presumably due tothe various attachments used
in fixed appliances which served as plaque retentive factor that
complicate cleaning. In a study conducted amongst adolescent
patients, the value of periodontal indices increased significantly
during orthodontic treatment, but were not associated with attachment
loss.[3]
Plaque accumulation contributes not only to the inflammation
of periodontal tissues, but may give rise to white spot lesions, decalcification and cavity formation. It is therefore important to
have proper plaque control as a preventive step to eliminate dental
plaque. Oral hygiene instruction (OHI) is proven to benefit the
patients’ oral hygiene significantly by resulting in reduced plaque
score and improved gingival condition.[4]
Verbal, written and video forms are the most common methods
used to give oral hygiene advice in dentistry. [5] All these instructional
methods given professionally by dental professionals improved
gingival conditions to a certain extent. However, there
was not enough evidence to support one method is better than
the other instructional methods. [6, 7] These could be due to
the methodological heterogeneity in these studies; Lee and Rock
(2000) spent thirty minutes for each verbal OHI session, but eight
minutes using video OHI methods.[6] Meanwhile, other studies
limited the assessment of the dental plaque to two third of the
teeth surface only. [8] Furthermore, the incorporation of single
arch assessment only as compared to upper and lower arches
across different studies may made the comparison of OHI methods
difficult.
Thus, the present study aimed to address these shortcomings in
the literature and primarily compared the effectiveness between
verbal, verbal-written and video methods of oral hygiene instruction
on the gingival health of patients with fixed appliances and
to assess the best method in providing oral health instructions to
patients wearing fixed appliances.
Materials And Methods
Study design
This was a prospective study with ethical approval obtained from
IIUM Research Ethics Committee (IREC) [Registration number:
IREC 2019-025].
Subjects
39 patients (31 females, 8 males) from 13 to 22 years old with a
mean age of 16.9 who were undergoing fixed orthodontics treatment
were recruited. Sample recruitment was done from March
2019 to January 2020. Inclusion criteria were patients who have
had extraction or non-extraction treatment and had been fitted
with upper and lower pre-adjusted edgewise fixed appliances
(MBT prescriptions, 0.022” x 0.028” slot size) on buccal and labial
surfaces during the previous 3 months, and had gingivitis on
at least half the number of total teeth erupted. Exclusion criteria
were subjects with impairment in hearing and vision, illiterate and
patients with craniofacial syndromes.
Information leaflet and consent
Information leaflet was prepared and patient was given time to
read the study design. Written consent form was given and signed
by the subjects. For subjects below 18 years old, parental consent
was recorded.
Oral hygiene instruction (OHI)
Group 1: A 5-minute OHI was given verbally by referring to a
written script. This verbal OHI was aided by the use of a model,
a toothbrush and an interdental brush.
Group 2: A 5-minute verbal instruction supplemented with a patient
information leaflet specially designed for this study was delivered.
The leaflet had similar information with Group 1.
Group 3: Participants were instructed to watch a specially designed
5-minute long video at chairside with the same amount
of information as in Group 1 and 2, but was presented in audiovisual
format.
Each session was restricted to five minutes and subjects were given
additional two minutes at the end of the session should there
be any questions.
Each OHI was introduced with five sections. First, subjects were
advised to use soft bristle toothbrush and fluoridated toothpaste.
The second section was to emphasize on the duration of tooth
brushing which was two minutes per session for twice a day. Next
was to teach comprehensive brushing technique by using modified
Bass technique to ensure no surfaces were left out. The participants
were instructed to focus on cleaning on the gingival third
and the area surrounding the brackets. The fourth section was on
interdental brushing using interdental brushes to clean the area
surrounding the orthodontic brackets for at least once per day.
The last section was on dietary advice which focused on reducing
the sugar amount and acidic food or beverage intake.
Calibration
Inter-examiner calibration was done to achieve synchronized
agreement between the two clinicians (N.M. and R.H.) in terms
of periodontal parameters measurements. Calibration was also
done to standardize the OHI delivery of all three methods.
Clinical procedure
At the start of the study and before the instructional methods
were given, each subject was examined for plaque index (PI),
gingival index (GI) and bleeding on probing (BOP) on six index
teeth: all second premolars (5’s), upper right central incisor (11)
and lower left central incisor (31). In the absence of 5’s, first premolars
(4’s) were used. Patients were seen six weeks later and the
periodontal parameters (PI, GI and BOP) were repeated for the
six index teeth.
Plaque index (PI)
The index tooth was divided into eight boxes by putting imaginary
lines dividing three parts of the tooth vertically and horizontally
with the bracket in the centre (Figure 1).
Plaque disclosing dye (Rondell Disclosing Pellets, Directa Dental
Company, Sweden) was applied on buccal and labial surfaces of
the six index teeth. Subjects were then asked to rinse their mouth
and the clinicians recorded the presence of plaque by placing a
tick into the respective boxes in a data collection form. Plaque was
scored corresponding to the eight boxes.
The maximum score for each patient was 48 ticks (8 ticks X 6
teeth). Score was calculated by adding the number of ticks on the
index teeth and divided by 48. The score was then multiplied by 100 to get the number in percentage.
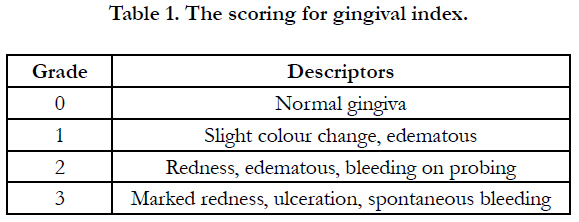
Gingival index (GI)
Gingival index was based on Loe and Silness (1963)[9] with a
scoring of 0 to 3. The grading used for gingival index was described
in Table 1.
William’s periodontal probe (Periodontal Probe 546/1, Medesy
Srl, Italy) was used with gentle pressure on the same index teeth
evaluated for plaque index. The tooth was examined on the buccal
and labial surfaces and it was divided into three sites (mesial,
mid and distal).
The maximum score for a site was 3 thus the maximum score for
a tooth was 9. The maximum sum for all the teeth was 54 (score 9
x 6 teeth). Therefore, gingival index was calculated by adding the
score for all sites and divided by 54. The score was then multiplied
by 100 to get the number in percentage.
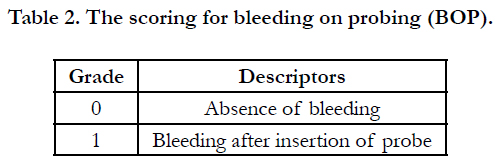
Bleeding on probing (BOP)
Bleeding on probing was also examined on buccal and labial surfaces
of the six index teeth and it was again divided into 3 sites
(mesial, mid and distal). William’s periodontal probe (Periodontal
Probe 546/1, Medesy Srl, Italy) was used with gentle pressure to
evaluate the BOP.Presence of bleeding was checked after a minimum
of ten seconds. The score was given based on the criteria
described in Table 2.
Maximum score for one site was 1, hence the maximum score
for 1 tooth was 3. The maximum scoring for all six teeth was 18
(score 3 x 6 teeth). Thus, BOP was calculated by summation of
the score for all sites and divided by 18. Percentage was then calculated
after multiplying the score by 100.
Statistical Analysis
Descriptive statistic was used to summarize the demographic
backgrounds of the subjects. As the data was normally distributed,
parametric tests were used to analyse the result. Paired sample
t-test was used in Statistical Package for the Social Sciences
software (SPSS version 20.0, IBM Corporation, United States of
America) to measure if there was any statistically significant difference
between pre and post-OHI in each group. Next, one-way
analysis of variance (ANOVA) was ran to compare if there was
any statistically significant difference between the verbal, verbalwritten
and video methods. P-value was set at less than 0.05 to
indicate statistical significance.
Results
39 subjects consisting of 31 females (79.5%) and 8 males (20.5%)
were analysed. The mean age of the participants was 16.9 ± 2.3
and ranged from 13 to 22 years old.
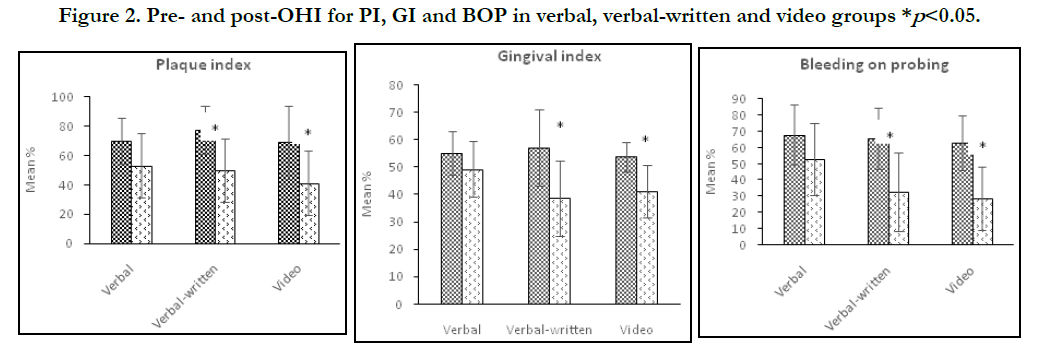
Reduction of PI, GI and BOP in each group
There was a reduction in the mean percentage of PI, GI and BOP
in all three groups. The t-test revealed that the reduction in verbal
group was statistically significant only for plaque index (p=0.012).
Gingival index (p=0.085) and bleeding on probing (p=0.062) did
not have statistical significant reduction in the verbal group. For
verbal-written and video groups, the changes in the mean percentage
were much larger and the reduction of all periodontal parameters
were statistically significant (Figure 2).
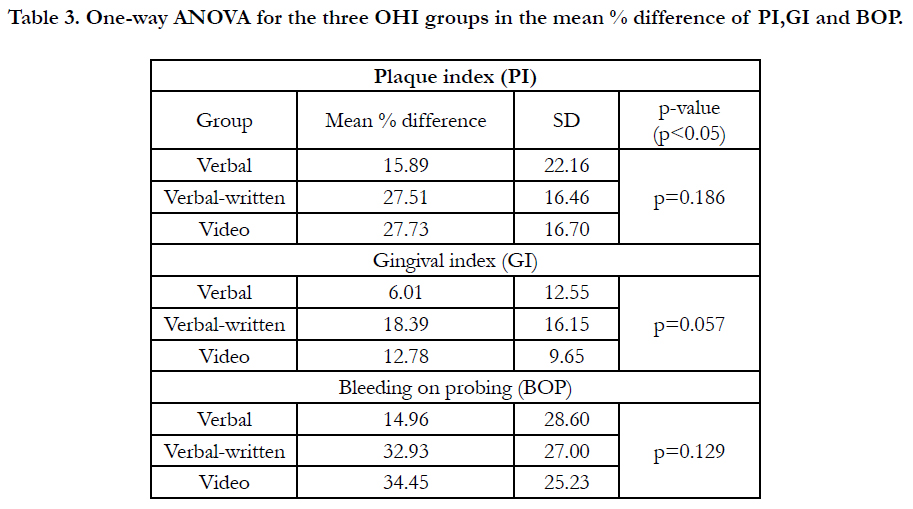
Comparisons of PI, GI and BOP between groups
One-way ANOVA revealed no statistically significant difference
between the three groups, although the improvement in GI had
p=0.057, a value that was very close to significance (Table 3).
Discussion
Patients wearing fixed appliances are highly associated with the
deterioration of gingival health due to the increase in plaque retentive
factor which enhances the accumulation of harmful microorganisms.[
3, 10] In accordance with that, proper OHI to patients
is very crucial to avoid the worsening of periodontal health
and therefore the best technique of OHI must be properly studied
to improve periodontal health.
The OHI given in this study emphasized on brushing with modified
Bass technique, using soft bristle toothbrushes and fluoridated
toothpaste for two minutes as they were proved to improve
oral hygiene and gingival health of orthodontic patients.[11] Interdental
brushing and reduction in dietary sugar intake were also
recommended to maximise the beneficial effects on periodontal
health. Interdental cleaning improves the effectiveness of eliminating
plaque interdentally which contributes to inflammation of
gingiva,[12] and controlled sugar may reduce the formation of the
plaque itself.[13]
Three periodontal parameters used in this study were PI, GI and
BOP. All three parameters were non-invasive, and were indicators
of different aspects of periodontal health. Plaque index was
analysed because dental plaque is the main predisposing factor
for gingivitis and periodontitis.[14] Meanwhile, gingival index assessed
the degree of inflammation at the marginal gingiva area
and bleeding on probing was used to indicate the gingival condition
at the base of the sulcus.[15]
Subjects in the verbal-written group exhibited significant improvements
in their periodontal parameters (PI, GI, BOP). Our
finding is parallel with the findings from Johnson and Sandford
[16] and Zuhal et al [17] who found that health instructions given
both verbally and written were more effective than verbal only.
In our study, standardization was a crucial key in the effectiveness
of the OHI as the information can be disseminated evenly
supplemented with written materials. Our research contrasts with
that of Lees and Rock [6] who argued that written information
resulted in the least improvement in the gingival health of patients
wearing fixed appliances when compared to verbal and
video techniques. The difference could be explained by the fact
that their subjects brought the illustrated instructions home without
any verbal component. It is also unclear whether the patients
actually took the initiative to read the written materials provided.
Therefore, it would appear that verbal OHI when given with written
materials could increase the effectiveness of information delivery
when compared with verbal or written instructions alone.
Shah et al [18] and Moshkelgosha et al [8] pointed out that subjects receiving video OHI had significant improvement in their gingival
health, similar to that found in our study. A likely explanation
is that standardization of information could be implemented via
audio-visual format and that the instructions could be replayed
as many times as required.[18] Although participants who were
illiterate were excluded, video OHI might be better appreciated by
this group of patients in real world due to its dynamic, interesting
and lively characteristics. It was interesting to highlight that in
our clinical observations, patients who received video-type OHI
were more engaged in the advices given, most probably stems
from the animation and illustration as well as the usage of various
colours which attracted their attention. Thus, verbal instructions
supplemented by visuals or written instructions helped improve
the gingival health of fixed appliance patients in our study.
On another side, our result contradicted with Lees and Rock [6]
who found that verbal OHI method resulted in the most improvement
in periodontal health. Their instructions given to the subjects
were not standardized especially in the duration, which lasted
up to thirty minutes in some subjects. The long OHI duration was
not employed in our study due to the possibility of low attention
span in adolescent group. The different method in obtaining the
plaque index in which they excluded the incisal/occlusal third of
the index tooth may also affect the result. Although they believed
that fixed appliance components only affected cleansing at the
gingival two-thirds, our opinion and findings differ as the incisal
part of the bracket was also a plaque retentive site. The presence
of plaque at the incisal third was particularly common. Subjects
were also more likely to lose interest during verbal OHI due to the
lack of visual aids, and verbal-only information did not help with
information retention among adolescents.[19] It was also noteworthy
to point that only plaque index showed improvement for
verbal group. From our perspective, due to the lack of attention
given by the patients during verbal OHI, they might be less proactive
in practicing the advices given. Since changes in the state
of gingival inflammation (reflected by GI and BOP) need longer
duration to manifest,[20] only plaque index showed significant
improvement in our study.
Our study did not find any significant differences between the
effectiveness of the three groups. This may be caused by other
factors apart from the techniques of delivering the advices. From
the ten social determinants of health outlined by World Health
Organization (WHO), the factors which are relevant to oral health
are dietary style and social gradient,[21] which might play a role in
the patients’ oral health condition, despite the success of various
OHI techniques delivered.
Excessive sugar intake is harmful for oral health as it may contribute
to the formation of dental plaque and cause oral diseases.
[13] Although advices on dietary sugar intake was included in
our OHI, its relation to the gingival health was not assessed. For
instance, verbal group might have more subjects who have high
sugar intake than the video group and as a result, the improvement
of oral hygiene of patients receiving verbal OHI might be
less remarkable than the video OHI group.
Next, people who are lower down the social hierarchy are two
times more likely to have serious diseases due to unfavourable
social surrounding and economical factor.[21] This is significant
since subjects with lower socioeconomical status tend to have
higher sugar intake and have less exposure to effective oral hygiene.[
22] Therefore, participants having different lifestyle might
not have the same level of motivation in improving their oral hygiene
practices albeit similar information delivered during OHI.
Changes in patients’ oral health is very dependent on the level
of knowledge and attitude exhibited by the individuals. This can
be understood through the ‘knowledge, attitude, practice’ (KAP)
theory by Pine and Harris.[23] A health education must follow the
KAP route to ensure success in patient’s attitude and behavioural
change. This model implies that practice is a patient’s response
to the information given, and therefore factors affecting the level
of knowledge and attitude of the person affect significantly their
level of application. The knowledge component was given in our
study by delivering the OHI through the three different methods.
However, the ability of the participants to truly understand and
practise the advices given were not objectively assessed.
The findings of this study might be helpful in facilitating the clinicians
and dental hygienist when emphasizing on the importance
of proper plaque control in patients wearing fixed appliance. Although
it did not indicate one specific OHI method is better than
the other, the results revealed that oral hygiene instructions still
play a very important role in maintaining good gingival health
throughout the fixed appliance treatment regardless of the methods
of delivery. The visual aids and leaflets used in the study have
the potential to be used as powerful educational tools during OHI
and orthodontic consent process.
Studies with longer duration of follow-up could be done because
the rate of gingival health improvement may vary from patients to
patients, and their long-term compliance to the instructions could
be assessed. In addition, studies to focus onpatient’s challenges in
practising the oral health instructions could be done.
In conclusions, whilst verbal method is effective in improving the
plaque index, verbal-written and video methods were effective in
improving all aspects of gingival health (plaque index, gingival
index and bleeding on probing) in patients wearing fixed appliances.
There is no single best method in delivering oral hygiene
instructions to patients with fixed appliances.
Financial support and sponsorship
This research was funded by IIUM Research Acculturation Grant
Scheme (IRAGS) 2018 from International Islamic University Malaysia
(IRAGS18-045-0046).
References
-
[1]. Al-Mobeeriek A, AlDosari AM. Prevalence of oral lesions among Saudi dental
patients. Ann Saudi Med. 2009 Sep-Oct;29(5):365-8. PubMed PMID:
19700894.
[2]. dos Santos Júnior J. Occlusion: Principles and Treatment. Quintessence Publishing (IL); 2007.
[3]. Firestone AR, Scheurer PA, Bürgin WB. Patients' anticipation of pain and pain-related side effects, and their perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1999 Aug;21(4):387-96. PubMed PMID: 10502901.
[4]. Majorana A, Bardellini E, Flocchini P, Amadori F, Conti G, Campus G. Oral mucosal lesions in children from 0 to 12 years old: ten years' experience. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 2010 Jul;110(1):e13-8. PubMed PMID: 20452255.
[5]. Köse O, Güven G, Özmen I, Akgün ÖM, Altun C. The oral mucosal lesions in pre-school and school age Turkish children. J EurAcadDermatolVenereol. 2013 Jan;27(1):e136-7. PubMed PMID: 22188486.
[6]. Kramer IR, Pindborg JJ, Bezroukov V, Infirri JS. Guide to epidemiology and diagnosis of oral mucosal diseases and conditions. World Health Organization. Community Dent Oral Epidemiol. 1980 Feb;8(1):1-26. Pub- Med PMID: 6929240.
[7]. Barmes DE, Infirri JS. WHO activities in oral epidemiology. Community Dent Oral Epidemiol. 1977 Jan;5(1):22-9. PubMed PMID: 264415.
[8]. Hussein SA, University of Sulaimani, Noori AJ. Prevalence of oral mucosal changes among 6- 13 year old children in Sulaimani city, Iraq. Sulaimani Dent J. 2014;1:5-9.
[9]. Bessa CF, Santos PJ, Aguiar MC, do Carmo MA. Prevalence of oral mucosal alterations in children from 0 to 12 years old. J Oral Pathol Med. 2004 Jan;33(1):17-22. PubMed PMID: 14675136.
[10]. Govindaraju L, Gurunathan D. Effectiveness of Chewable Tooth Brush in Children-A Prospective Clinical Study. J ClinDiagn Res. 2017 Mar;11(3):ZC31-ZC34. PubMed PMID: 28511505.
[11]. Christabel A, Anantanarayanan P, Subash P, Soh CL, Ramanathan M, Muthusekhar MR, et al. Comparison of pterygomaxillarydysjunction with tuberosity separation in isolated Le Fort I osteotomies: a prospective, multicentre, triple-blind, randomized controlled trial. Int J Oral Maxillofac Surg. 2016 Feb;45(2):180-5. PubMed PMID: 26338075.
[12]. Soh CL, Narayanan V. Quality of life assessment in patients with dentofacial deformity undergoing orthognathic surgery--a systematic review. Int J Oral Maxillofac Surg. 2013 Aug;42(8):974-80. PubMed PMID: 23702370. [13]. Mehta M, Deeksha, Tewari D, Gupta G, Awasthi R, Singh H, et al. Oligonucleotide therapy: An emerging focus area for drug delivery in chronic inflammatory respiratory diseases. ChemBiol Interact. 2019 Aug 1;308:206- 215. PubMed PMID: 31136735.
[14]. Ezhilarasan D, Apoorva VS, Ashok Vardhan N. Syzygiumcumini extract induced reactive oxygen species-mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med. 2019 Feb;48(2):115-121. PubMed PMID: 30451321.
[15]. Campeau PM, Kasperaviciute D, Lu JT, Burrage LC, Kim C, Hori M, et al. The genetic basis of DOORS syndrome: an exome-sequencing study. Lancet Neurol. 2014 Jan;13(1):44-58. PubMed PMID: 24291220.
[16]. Kumar S, Sneha S. Knowledge and awareness regarding antibiotic prophylaxis for infective endocarditis among undergraduate dental students. Asian J Pharm Clin Res. 2016 Oct 1:154-9.
[17]. Christabel SL, Gurunathan D. Prevalence of type of frenal attachment and morphology of frenum in children, Chennai, Tamil Nadu. World J Dent. 2015 Oct;6(4):203-7.
[18]. Kumar S, Rahman R. Knowledge, awareness, and practices regarding biomedical waste management among undergraduate dental students. Asian J Pharm Clin Res. 2017 Aug 1;10:341-5.
[19]. Sridharan G, Ramani P, Patankar S. Serum metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Cancer Res Ther. 2017 Jul- Sep;13(3):556-561. PubMed PMID: 28862226.
[20]. Ramesh A, Varghese SS, Doraiswamy JN, Malaiappan S. Herbs as an antioxidant arsenal for periodontal diseases. J IntercultEthnopharmacol. 2016 Jan 27;5(1):92-6. PubMed PMID: 27069730.
[21]. Thamaraiselvan M, Elavarasu S, Thangakumaran S, Gadagi JS, Arthie T. Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian SocPeriodontol. 2015 Jan-Feb;19(1):66-71. PubMed PMID: 25810596.
[22]. Thangaraj SV, Shyamsundar V, Krishnamurthy A, Ramani P, Ganesan K, Muthuswami M, et al. Molecular Portrait of Oral Tongue Squamous Cell Carcinoma Shown by Integrative Meta-Analysis of Expression Profiles with Validations. PLoS One. 2016 Jun 9;11(6):e0156582. PubMed PMID: 27280700.
[23]. Ponnulakshmi R, Shyamaladevi B, Vijayalakshmi P, Selvaraj J. In silico and in vivo analysis to identify the antidiabetic activity of beta sitosterol in adipose tissue of high fat diet and sucrose induced type-2 diabetic experimental rats. ToxicolMech Methods. 2019 May;29(4):276-290. PubMed PMID: 30461321.
[24]. Ramakrishnan M, Bhurki M. Fluoride, fluoridated toothpaste efficacy and its safety in children-review. Int J Pharm Res. 2018 Oct 1;10(04):109-4.
[25]. Shulman JD. Prevalence of oral mucosal lesions in children and youths in the USA. Int J Paediatr Dent. 2005 Mar;15(2):89-97. PubMed PMID: 15790365.
[26]. Baricevic M, Mravak-Stipetic M, Majstorovic M, Baranovic M, Baricevic D, Loncar B. Oral mucosal lesions during orthodontic treatment. Int J Paediatr Dent. 2011 Mar;21(2):96-102. PubMed PMID: 21121986.
[27]. Favia G, Limongelli L, Tempesta A, Maiorano E, Capodiferro S. Oral lesions as first clinical manifestations of Crohn's disease in paediatric patients: a report on 8 cases. Eur J Paediatr Dent. 2020 Mar;21(1):66-69. PubMed PMID: 32183532.
[28]. Hong CHL, Dean DR, Hull K, Hu SJ, Sim YF, Nadeau C, et al. World Workshop on Oral Medicine VII: Relative frequency of oral mucosal lesions in children, a scoping review. Oral Dis. 2019 Jun;25Suppl 1:193-203. PubMed PMID: 31034120.
[29]. Oral Mucosal Space/Surface Lesions. Diagnostic Imaging: Oral and Maxillofacial. 2017:926–9.
[30]. Reichart PA. Oral mucosal lesions in a representative cross-sectional study of aging Germans. Community Dent Oral Epidemiol. 2000 Oct;28(5):390-8. PubMed PMID: 11014516.
[31]. Ali M, Sundaram D. Biopsied oral soft tissue lesions in Kuwait: a sixyear retrospective analysis. Med PrincPract. 2012;21(6):569-75. PubMed PMID: 22699793.
[32]. de Muñiz BR, Crivelli MR, Paroni HC. Clinical study of oral soft tissue lesions in boys in a children's home. Rev AsocOdontol Argent. 1981 Sep- Oct;69(7):405-8. PubMed PMID: 6950468.
[33]. Medina AC, Sogbe R, Gómez-Rey AM, Mata M. Factitial oral lesions in an autistic paediatric patient. Int J Paediatr Dent. 2003 Mar;13(2):130-7. PubMed PMID: 12605633.
[34]. Kovac-Kovacic M, Skaleric U. The prevalence of oral mucosal lesions in a population in Ljubljana, Slovenia. J Oral Pathol Med. 2000 Aug;29(7):331- 5. PubMed PMID: 10947249.
[35]. Jin X, Zeng X, Wu L. Oral Mucosal Lesions of Systemic Diseases. Case Based Oral Mucosal Diseases. 2018:169-97.
[36]. VijayashreePriyadharsini J. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol. 2019 Dec;90(12):1441-1448. PubMed PMID: 31257588.
[37]. J PC, Marimuthu T, C K, Devadoss P, Kumar SM. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin Implant Dent Relat Res. 2018 Aug;20(4):531-534. PubMed PMID: 29624863.
[38]. Ramesh A, Varghese S, Jayakumar ND, Malaiappan S. Comparative estimation of sulfiredoxin levels between chronic periodontitis and healthy patients - A case-control study. J Periodontol. 2018 Oct;89(10):1241-1248. PubMed PMID: 30044495.
[39]. Ramadurai N, Gurunathan D, Samuel AV, Subramanian E, Rodrigues SJL. Effectiveness of 2% Articaine as an anesthetic agent in children: randomized controlled trial. Clin Oral Investig. 2019 Sep;23(9):3543-3550. PubMed PMID: 30552590.
[40]. Sridharan G, Ramani P, Patankar S, Vijayaraghavan R. Evaluation of salivary metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Oral Pathol Med. 2019 Apr;48(4):299-306. PubMed PMID: 30714209.
[41]. Ezhilarasan D, Apoorva VS, Ashok Vardhan N. Syzygiumcumini extract induced reactive oxygen species-mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med. 2019 Feb;48(2):115-121. PubMed PMID: 30451321.
[42]. Mathew MG, Samuel SR, Soni AJ, Roopa KB. Evaluation of adhesion of Streptococcus mutans, plaque accumulation on zirconia and stainless steel crowns, and surrounding gingival inflammation in primary molars: randomized controlled trial. Clin Oral Investig. 2020 Sep;24(9):3275-3280. PubMed PMID: 31955271.
[43]. Samuel SR. Can 5-year-olds sensibly self-report the impact of developmental enamel defects on their quality of life? Int J Paediatr Dent. 2021 Mar;31(2):285-286. PubMed PMID: 32416620.
[44]. R H, Ramani P, Ramanathan A, R JM, S G, Ramasubramanian A, et al. CYP2 C9 polymorphism among patients with oral squamous cell carcinoma and its role in altering the metabolism of benzo[a]pyrene. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020 Sep;130(3):306-312. PubMed PMID: 32773350.
[45]. Chandrasekar R, Chandrasekhar S, Sundari KKS, Ravi P. Development and validation of a formula for objective assessment of cervical vertebral bone age. ProgOrthod. 2020 Oct 12;21(1):38. PubMed PMID: 33043408.
[46]. VijayashreePriyadharsini J, SmilineGirija AS, Paramasivam A. In silico analysis of virulence genes in an emerging dental pathogen A. baumannii and related species. Arch Oral Biol. 2018 Oct;94:93-98. PubMed PMID: 30015217.