Prevalence Of Paediatric Oral Mucosal Lesions: A Retrospective Study in Saveetha Dental College, Chennai
Chenchulakshmi G1, Arvind M2*
1 Post Graduate Resident, Department of Oral Medicine and Radiology, SIMATS, Chennai, 600007, India.
2 Professor and Head of Department of Oral Medicine and Radiology, SIMATS,Chennai, 600007, India.
*Corresponding Author
Dr. Arvind M,
Professor and Head of Department of Oral Medicine and Radiology, SIMATS, Chennai, 600007, India.
E-mail: arvindmuthukrishnan@yahoo.com
Received: October 21, 2021; Accepted: January 27, 2022; Published: April 11, 2022
Citation: Chenchulakshmi G, Arvind M. Prevalence Of Paediatric Oral Mucosal Lesions: A Retrospective Study in Saveetha Dental College, Chennai. Int J Dentistry Oral Sci. 2022;9(4):5276-5281. doi: dx.doi.org/10.19070/2377-8075-220001057
Copyright: Arvind M©2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Mucosal lesions can either be congenital, developmental, infective, inflammatory, allergic, neoplastic and oral
changes due to underlying systemic disorders. Mucosal lesions in paediatric population can contribute to general ill health.
The oral mucosal lesions in children present as vesicles, ulcers, macules, changes in color, size alterations, and configuration
of the oral anatomy.Ulcerations, pain, and discomfort are frequent side effects, which result from irritation caused mainly by
fixed orthodontic appliances. Although painful and unpleasant, lesions heal quickly because of the fast metabolism of oral
mucosa in young and healthy patients. Epidemiological studies help in determining the incidence, prevalence and the severity
of diseases. They also help in assessing the distribution, the risk factors and associated aetiology. This information is useful
in the formulation of health care programmes at the primary level to spread awareness, help guide in early diagnosis and lead
to prompt treatment. Thorough clinical examination, evaluation and diagnosis is important to initiate the correct treatment.
Objective:-The purpose of this study was to determine the prevalence of oral mucosal lesions in paediatric patients visiting
the Department of Pediatric and Oral Medicine.
Methods: A retrospective study was conducted in patients visiting the Paediatric and oral medicine department with oral mucosal
lesions. Data was collected from an Electronic database. The results obtained were processed and descriptive statistical
analysis was made.
Results: Out of 7374 paediatric patients, 29 patients were reported with oral mucosal lesions. The total number of males were
fifteen and females were 15 reported to the department with oral mucosal lesions.
Conclusion: Aphthous stomatitis is the most frequently reported lesion. Early diagnosis and treatment of paediatric immune
mediated mucosal lesions can prevent future cutaneous involvement.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Oral Mucosal Lesions; Paediatric Population; Aphthous Stomatitis.
Introduction
Oral mucosal lesions can be identified by their etiology, clinical
characteristics, and prognosis. Oral health is the entire health of
the teeth, mucosal areas, periodontal tissues and tongue. The concept
of oral and dental health is mostly perceived to be limited
to carious teeth and periodontal diseases by both clinicians and
academics. Based on this view, diseases of oral mucosal areas
are generally ignored by dental practitioners.There are relatively
few reports in the literature regarding oral mucosal conditions
in children.[1] The most common oral disease, caries, is studied
the most, and cancer therapyrelated mucosal disorders are also
commonly described. Furthermore, the exact prevalence of oral
mucosal lesions in healthy children is controversial due to a lack
of standardized methods, different diagnostic criteria, and the description
of very few lesions in each survey. The lack of epidemiologic
data in this matter may lead to diseases of the soft tissues
of the oral cavity being overlooked. Despite World Health Organization
recommendations, the epidemiologic literature about
children and adolescents in this field is quite limited. Moreover,
the signs and symptoms of oral mucosal disorders in childhood
can change with aging and are often different from common adult
oral pathologies. These differences should be recognized by clinicians,
and are aided by epidemiologic studies that document the
frequency of oral lesions in children. Proper examination of the
oral mucosa is helpful in diagnosing developmental, neoplastic, infectious, or inflammatory alterations (1). The oral mucosal lesions
in children present as vesicles, ulcers, macules, changes in
color, size alterations, and configuration of the oral anatomy
[1]. Epidemiological studies help in determining the incidence,
prevalence and the severity of diseases [2]. Ulcerations, pain, and
discomfort are frequent side effects, which result from irritation
caused mainly by fixed orthodontic appliances. Although painful
and unpleasant, lesions heal quickly because of the fast metabolism
of oral mucosa in young and healthy patients [3]. They also
help in assessing the distribution, the risk factors and associated
aetiology [4]. This information is useful in the formulation of
health care programmes at the primary level to spread awareness,
help guide in early diagnosis and lead to prompt treatment [5].
Several studies have reported different frequencies of oral mucosal
lesions in various locations. The clinical examination is to
obtain a diagnosis of oral conditions and lesions is fundamental,
which is why it must be correct, thorough, and systematic manner
[6]. The exam of soft tissues in pediatric patients involves knowledge
of normal size, shape, color, and texture of the structures
that comprise it [7]. The correct exploration of the oral mucosa
can provide important tools in diagnosing developmental, neoplastic,
infectious, or inflammatory alterations [8]. The lesions in
oral mucosa in children can present as vesicles, ulcers, macules,
changes in color, size alterations, and configuration of the oral
anatomy [9]. Andres Pinto et al in 2014, in his article (Pediatric
Soft Tissue Oral Lesions) he divided the lesions into several categories
according to lesions types as follows. Anatomic Variations
in Gingiva, Frenum.
a) Developmental Lesions: Geographic tongue, Fissured tongue,
Retro cuspidpapillae ,Gingival overgrowth.
b) Mucosal Changes (COLOR): White Lesions, Linea Alba, Leukoedema,
Pseudo membranous candidiasis, White sponge nevus.
Red And/Or White Lesions: Petechiae, Purpura,Ecchymosis,
Erythematous Candidiasis. Angular Cheilitis, Erythema Migrans
(Benign Migratory Glossitis), Median Rhomboid Glossitis.
c) Brown-Black Lesions: Physiologic Pigmentation, Amalgam
Tattoo/Graphite, Melanocytic Nevus.
d) Soft Tissue Nodules: Inflammatory/reactive lesions- Mucocele,
Irritation fibroma, Peripheral ossifying fibroma, Pyogenic
granuloma, Peripheral giant cell granuloma.
e) Benign Tumors: Hemangioma, Lymphatic malformations, Fibroma,
Benign neoplasms Squamous papilloma.
f) Cysts: Eruption cyst
g) Ulcerations: Traumatic ulcers,Aphthous ulcers.
h) Infections: Herpes simplex virus, Coxsackievirus, Herpangina,
Hand, foot, mouth, Candida albicans, HIV infection
The most common lesions were angular cheilitis (14.7%), followed
by herpes labialis (10.7%), impetigo (9.3%), geographic
tongue, recurrent aphthous ulcer, and verruca vulgaris (2.7 %).
The purpose of this study was to determine the prevalence of
oral mucosal lesions in paediatric patients visiting the Department
of Pediatric and Oral Medicine. It will also serve as a baseline
for future studies with the goal of finding ways to improve oral
health in this region. Previously our team has a rich experience in
working on various research projects across multiple disciplines
[10-24]. Now the growing trend in this area motivated us to pursue
this project.
Materials And Methods
A retrospective study was conducted from a time period of June
2019 - March 2021 in patients visiting the Paediatric and Oral
medicine Department with oral mucosal lesions. Data was collected
from an Electronic database. Inclusion criteria were patients
from 3 years to 17 years old of both genders. The results
obtained were processed using Microsoft office Excel worksheet
and descriptive statistical analysis was done.This retrospective
study was done to determine the prevalence of oral mucosal lesions
in paediatric patients visiting the Department of Paediatric
and Oral Medicine. The results are presented in tables showing
the number of lesions found in males and females in the paediatric
population.
Results
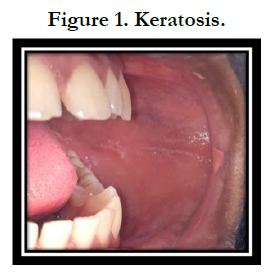
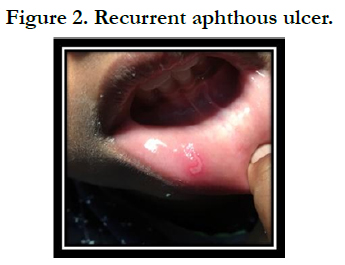
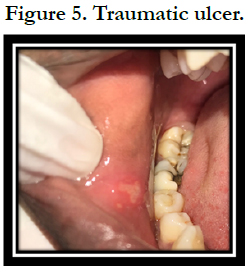
Seven thousand three hundred and seventy-four paediatric patients
were reported in the time period of 2 years (2019-2021), out
of them 28 patients reported with oral mucosal lesions. Figure 1
represents Keratosis seen in left buccal mucosa, Figure 2 represents
Recurrent Aphthous ulcer on lower labial mucosa, Figure 3
represents Lichen planus seen on left retromolar region in relation
to lower posteriors, Figure 4 represents Angular cheilitis in right
commissures of lips, Figure 5 represents Traumatic ulcer on right
buccal mucosa.
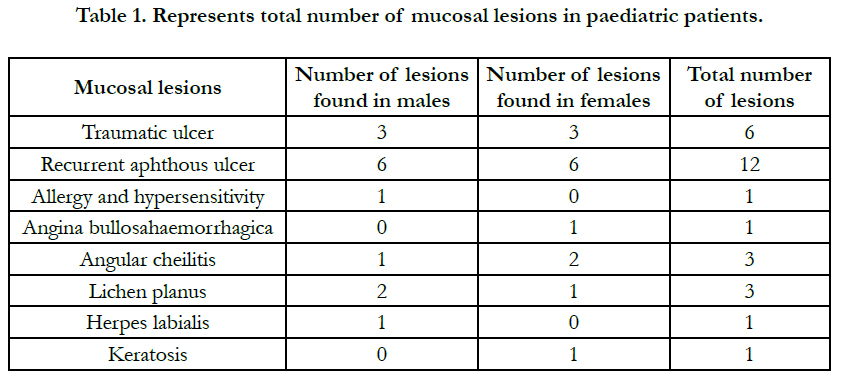
Table 1 represents the total number of lesions seen in the paediatric
population included in the study. Traumatic ulcer seen in 6 patients(
3 males and 3 females), Recurrent aphthous ulcer seen in 12
patients (6 males and 6 females), Allergy and hypersensitivity seen
in 1 patient (1 in male), Angina bullosa haemorrhagica in 1 patient
(1 female), Angular cheilitis in 3 patients (1 male and 2 females),
Lichen planus in 3 patients (2 males and 1 female), Herpes labialis
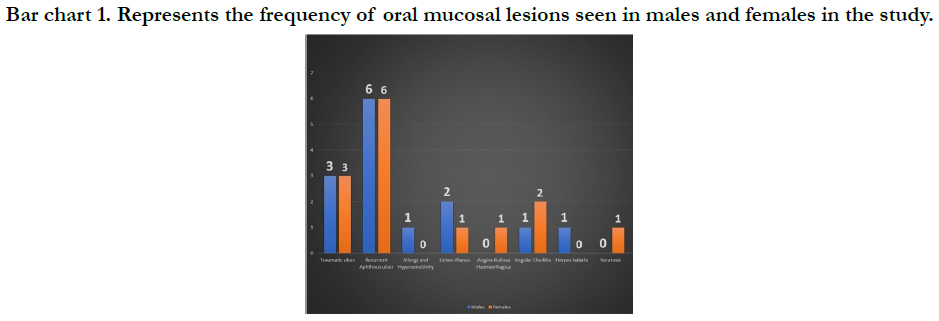
in 1 patient (1 male) and Keratosis in 1 patient (1 female). Bar
chart 1 representing the frequency of oral mucosal lesions seen in
males and females in the paediatric population in the study.
Bar chart 1. Represents the frequency of oral mucosal lesions seen in males and females in the study.
Discussion
Oral mucosal lesions found in children are distinct from those found in adults [25]. This may be a result of physical development
and growth that takes place in children [26]. They differ from
different populations not only because of their small sizes [27],
but also because certain lesions have a predilection for children.
Oral mucosal lesions can be identified by their aetiology, clinical
characteristics, and prognosis. Oral health is the entire health
of the teeth, mucosal areas, periodontal tissues and tongue. The
concept of oral and dental health is mostly perceived to be limited
to carious teeth and periodontal diseases by both clinicians
and academics. Based on this view, diseases of oral mucosal areas
are generally ignored by dental practitioners. There are relatively
few reports in the literature regarding oral mucosal conditions in
children.[1] Proper examination of the oral mucosa is helpful in
diagnosing developmental, neoplastic, infectious, or inflammatory alterations [28]. The oral mucosal lesions in children present
as vesicles, ulcers, macules, changes in color, size alterations, and
configuration of the oral anatomy [29]. Epidemiological studies
help in determining the incidence, prevalence and the severity
of diseases [30]. This survey was a retrospective study designed
to evaluate the prevalence of oral mucosal lesions in children attended
the Department of Medicine and Pediatric Dentistry in
Saveetha dental college. Retrospective studies are important in
estimating the prevalence of a disease in the population and in
identifying high-risk populations in paediatric population mainly.
The study was approved by the Ethical Committee at the Saveetha
College.
The prevalence of oral mucosal lesions in this study was 37.2%.
Out of 7374 paediatric patients, 28 patients were reported with
oral mucosal lesions (14 females and 15 males). Traumatic ulcer
seen in 6 patients, Recurrent aphthous stomatitis seen in 12 patients,
Allergy and hypersensitivity seen in 1 patient, Angina bullosa
nervosa seen in 1 patient, Angular cheilitis seen in 3 patients,
Lichen planus in 3 patients, Herpes labialis in 1 patient, Keratosis
seen in 1 patient. The percentage of the lesions found in this
study was in accordance with that observed in Argentina by Crivelliet
al. (1988) -39.04%) and Spain by (García-Polaet al. (2002)
-38.94%). The most prevalent lesions were minor aphthous ulcer
(21.5%), irritation fibroma (15.7%), traumatic ulcer (15.7%),
traumatic erosion (10.5%), impetigo (10.5 %), pigmented lesions
(5.2%), herpes labialis (5.2%), intraoral herpes (5.2 %), mucocele
(5.2%) and ranula (5.2 %). No malignant lesions were found in
the present study, which confirms the rarity of these lesions in
the oral cavity [31]. Recurrent aphthous stomatitis (RAS) is one
of the most common oral diseases. Despite intensive research, the
definite aetiology could not be found, but there is genetic predisposition,
with strong associations with interleukin genotypes, and
sometimes a family history [20]. Approximately 50% of women
and 40% of men experienced the aphthous stomatitis 2 or more
times throughout their lives [7]. The RAS begins during childhood
and adolescence, and is seen clinically in 3 forms; minor,
major and herpetiform aphthae. Minor RAS is the most common
type [20]. In our study the incidence of recurrent aphthous stomatitis
is 2.3%. The other studies with children in the literature,
this ratio was found to be 1.57% in Brazil [10] and 4.08% in Spain
[6]. And the rate was found to be 10.87% in the study conducted
by Crivelli et al. [17] in Argentina. When we evaluated the correlation
between socioeconomic status and the RAS in Argentinean
study, the rate is 19% in schools in the region with higher socioeconomic
status, and this rate is 12% in the school in the region
with low socioeconomic status [17]. In the study conducted by
Bessa et al. [10], there was no significant correlation between socioeconomic
status and the RAS. Lichen planus (LP) is a chronic
inflammatory, autoimmune disease, affecting a wide variety of
sites, including skin and mucous membranes. In contrast to dermal
LP, oral lichen planus (OLP) demonstrates clinical variability.
The prevalence of OLP ranges between 0.5% and 3% and may
occur in 70% to 77% of patients with cutaneous LP. However,
some studies report that OLP, without cutaneous involvement
occurs more commonly. It is currently considered a disease of
unknown aetiology and with multifactorial pathogenesis. Most
studies suggest that LP is a CD8+ T cell-mediated autoimmune
disease. It is believed that the CD8+ T lymphocytes induce keratinocyte
apoptosis and cause epithelial basal cell layer damage.
[2] Possible causes of OLP such as an allergy to dental restorative
materials (amalgam, gold), local trauma (Koebner phenomenon)
and hepatitis B or C virus infection have been reported.
Moreover, genetic factors, lifestyle and emotional stress may be
contributing factors in its pathogenesis. Many drugs are capable
of producing a lichenoid drug eruption.OLP is most frequently
manifested during the fifth and sixth decades of life. OLP commonly
affects buccal mucosa, although tongue, gingiva and palatal
mucosa may also be affected.[2] In both adults and children
cutaneous LP is characterised by extremely pruritic eruption of
flat-topped, polygonal and violaceous papules with overlying fine
reticular striations known as Wickham Striae.[6] OLP presents in
mainly three different clinical forms. In order of advancing severity
and symptomatology, they are reticular, plaque and erosive
types.[7] Reticular OLP typically presents as asymptomatic, greyish
white, lacy, interlacing striae. The plaque form is characterised
by slightly elevated, irregular white patches while the erosive form
is erythematous and frequently painful [3, 7]. Histopathology of
OLP reveals hyperkeratosis, acanthosis, liquefaction degeneration
of basal cells and existence of a band of lymphocytic infiltrate in
close proximity to surface epithelium.It is rare in children, in our
study only one case of oral lichen planus is reported [4]. Cheilitis
is clinically characterised by the lesions which are a few millimetres
in length and extend from the corners of the mouth to the cheeks.
Erosions, ulcerations and fissures occur over the time [7]. The aetiology
is thought to include low vertical size, mechanical trauma,
Candida albicans, Staphylococcus and Streptococcus infections,
iron deficiency anaemia and riboflavin deficiency [15]. Angular
Cheilitis is a chronic inflammation of the skin and labial mucosa
at the corners of the mouth. The aetiology may be due to nutritional
deficiencies (riboflavin, folate), anaemia (iron deficiency)
allergy, infections, physical irritation, low socioeconomic status,
and bruxism. The prevalence in children is low when compared
to adult population or in adolescents. Clinical presentation of angular
cheilitis is usually characterised by the presence of painful
cracking, fissuring, and erythema on bilateral commissures. Incidence
of cheilitis in our study population is less compared to
other studies [8]. Herpes labialis is a common disease caused by infection with herpes simplex virus, most often type 1. Primary
infection with herpes simplex is asymptomatic in the majority of
children (8899%), but when symptomatic, it commonly presents
as acute gingivostomatitis [19]. Herpes labialis is the reactivation
of the primary infection, often following a prodromal period, and
lesions present early on as clusters of vesicles on the lip which
soon burst and scab over. The lesions usually last for 710 days
before resolving. Like geographical tongue, the condition is intermittent,
and its precipitating factors are said to include trauma,
immunosuppression, exposure to sunlight, stress or other illness.
There are many causes of traumatic ulcerations in the mouth.
These can be classified as physical, chemical, thermal, and radial
[7]. Sharp-edged teeth or restorations, rough fillings or habits
such as cheek biting, hardly tooth brushing, burns due to the high
temperature causes traumas [15]. Especially in children, as a result
of biting the lip due to the numbness following the mandibular
anaesthesia, larger traumatic ulcerations may usually occur on the
lower lip [7]. A lot of chemicals and drugs can cause chemical irritation
of the tissues inside the mouth. Many of these substances
are caustic. Aspirin, sodium perborate, hydrogen peroxide and
alcohol are some of these substances. Clinical features and history
are important in the diagnosis of all traumatic lesions. The
treatment strategy is based on the removal of the etiologic traumatic
factor. In our study, traumatic lesions were the second most
common oral mucosal lesion with the rate of 3.17%. In a study
of Benavides et al.[11] which was conducted in Brazil, incidence
of traumatic lesions is 6%, and in the study conducted by Garcia-
Pola et al.[6], this rate is in second place with the rate of 22.15%.
Several studies in different geographic locations have reported
frequency in oral mucosal lesions. In a study conducted in Argentina
by Muniz et al.In 1981 [32], for a total sample of 75 healthy
paediatric male patients, ages 6 to 13, 46 patients presented oral
mucosal lesions, with a prevalence of 61.3 %. Even though it is
rare, the dental practitioner should remain alert for any suspicious
lesion. Non-traumatic white patches, white patches with red areas,
chronic non-healing ulcers, and indurated lesions are some
of the features which would make a lesion suspicious and should
be investigated further [33]. Opportunistic screening of high-risk
individuals will go a long way in detecting oral cancer and precancer
at a relatively early stage. For the dentists to fully contribute
to improvement of early detection, they must perform thorough
examinations [34]. Repeatedly training oneself to scrutinise the
entire oral mucosa in a systematic fashion reduces the chance of
missing any lesion [1].
The lesions were identified without assistance of laboratory or
histological tests [35]. While trained examiners can be expected to
identify many entities (such as aphthous ulcers, nicotinic stomatitis
and recurrent herpes labialis) without additional diagnostic
aids, others (such as nevus) may have other differential diagnoses
and can be diagnosed clinically with less certainty. Furthermore,
some lesions (tumours, nonspecific lesions and lesions of
unknown aetiology) require biopsy for confirmation. The prevalence
of mucosal lesions in this study are present as acute problems
where people may be more inclined to seek treatment for
mucoceles, ranulas (even buccal mucosa fibromas that suffer biting
trauma at every meal) and other acute conditions, so these
are less likely to be seen in prevalence studies. The diagnosis of
these oral mucosal lesions is a challenge for the dentist because
of its varied clinical expression. This study demonstrates that patients
in the paediatric population are more prone to developing
oral mucosal lesions. Future studies should focus on multivariate
models to explore the risk factors for lesions that are of clinical
significance. Although there were a number of studies on each
condition, few were directly comparable in terms of the methodology
applied. There was substantial variation between reports
in a number of elements important to an epidemiological study,
such as the diagnostic criteria and method of detection employed,
although, in many instances, there was inadequate detail to allow
full appraisal of the methodology. There is a need for more good
quality epidemiological studies in this area.Our institution is passionate
about high quality evidence based research and has excelled
in various fields [36-46].
Conclusion
Aphthous stomatitis is the most frequently reported lesion. Good
nutrition and appropriate oral hygiene maintenance could prevent
a lot of inflammatory and infective associated paediatric oral lesions.
Early diagnosis and treatment of paediatric immune mediated
mucosal lesions can prevent future cutaneous involvement.
Clinicians should be aware that prevalence for mucosal lesions in
adults are different from those for children and for some conditions,
prevalence increases with age as well as gender predilection.
Studies of adult populations, however may be valid, they
may have limited applicability to children. Mostly caution should
be definitely used in applying reported prevalence unless the ages
and other demographic characteristics of the subjects are similar
to those of the patients.
References
-
[1]. Al-Mobeeriek A, AlDosari AM. Prevalence of oral lesions among Saudi dental
patients. Ann Saudi Med. 2009 Sep-Oct;29(5):365-8. PubMed PMID:
19700894.
[2]. dos Santos Júnior J. Occlusion: Principles and Treatment. Quintessence Publishing (IL); 2007.
[3]. Firestone AR, Scheurer PA, Bürgin WB. Patients' anticipation of pain and pain-related side effects, and their perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1999 Aug;21(4):387-96. PubMed PMID: 10502901.
[4]. Majorana A, Bardellini E, Flocchini P, Amadori F, Conti G, Campus G. Oral mucosal lesions in children from 0 to 12 years old: ten years' experience. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 2010 Jul;110(1):e13-8. PubMed PMID: 20452255.
[5]. Köse O, Güven G, Özmen I, Akgün ÖM, Altun C. The oral mucosal lesions in pre-school and school age Turkish children. J EurAcadDermatolVenereol. 2013 Jan;27(1):e136-7. PubMed PMID: 22188486.
[6]. Kramer IR, Pindborg JJ, Bezroukov V, Infirri JS. Guide to epidemiology and diagnosis of oral mucosal diseases and conditions. World Health Organization. Community Dent Oral Epidemiol. 1980 Feb;8(1):1-26. Pub- Med PMID: 6929240.
[7]. Barmes DE, Infirri JS. WHO activities in oral epidemiology. Community Dent Oral Epidemiol. 1977 Jan;5(1):22-9. PubMed PMID: 264415.
[8]. Hussein SA, University of Sulaimani, Noori AJ. Prevalence of oral mucosal changes among 6- 13 year old children in Sulaimani city, Iraq. Sulaimani Dent J. 2014;1:5-9.
[9]. Bessa CF, Santos PJ, Aguiar MC, do Carmo MA. Prevalence of oral mucosal alterations in children from 0 to 12 years old. J Oral Pathol Med. 2004 Jan;33(1):17-22. PubMed PMID: 14675136.
[10]. Govindaraju L, Gurunathan D. Effectiveness of Chewable Tooth Brush in Children-A Prospective Clinical Study. J ClinDiagn Res. 2017 Mar;11(3):ZC31-ZC34. PubMed PMID: 28511505.
[11]. Christabel A, Anantanarayanan P, Subash P, Soh CL, Ramanathan M, Muthusekhar MR, et al. Comparison of pterygomaxillarydysjunction with tuberosity separation in isolated Le Fort I osteotomies: a prospective, multicentre, triple-blind, randomized controlled trial. Int J Oral Maxillofac Surg. 2016 Feb;45(2):180-5. PubMed PMID: 26338075.
[12]. Soh CL, Narayanan V. Quality of life assessment in patients with dentofacial deformity undergoing orthognathic surgery--a systematic review. Int J Oral Maxillofac Surg. 2013 Aug;42(8):974-80. PubMed PMID: 23702370. [13]. Mehta M, Deeksha, Tewari D, Gupta G, Awasthi R, Singh H, et al. Oligonucleotide therapy: An emerging focus area for drug delivery in chronic inflammatory respiratory diseases. ChemBiol Interact. 2019 Aug 1;308:206- 215. PubMed PMID: 31136735.
[14]. Ezhilarasan D, Apoorva VS, Ashok Vardhan N. Syzygiumcumini extract induced reactive oxygen species-mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med. 2019 Feb;48(2):115-121. PubMed PMID: 30451321.
[15]. Campeau PM, Kasperaviciute D, Lu JT, Burrage LC, Kim C, Hori M, et al. The genetic basis of DOORS syndrome: an exome-sequencing study. Lancet Neurol. 2014 Jan;13(1):44-58. PubMed PMID: 24291220.
[16]. Kumar S, Sneha S. Knowledge and awareness regarding antibiotic prophylaxis for infective endocarditis among undergraduate dental students. Asian J Pharm Clin Res. 2016 Oct 1:154-9.
[17]. Christabel SL, Gurunathan D. Prevalence of type of frenal attachment and morphology of frenum in children, Chennai, Tamil Nadu. World J Dent. 2015 Oct;6(4):203-7.
[18]. Kumar S, Rahman R. Knowledge, awareness, and practices regarding biomedical waste management among undergraduate dental students. Asian J Pharm Clin Res. 2017 Aug 1;10:341-5.
[19]. Sridharan G, Ramani P, Patankar S. Serum metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Cancer Res Ther. 2017 Jul- Sep;13(3):556-561. PubMed PMID: 28862226.
[20]. Ramesh A, Varghese SS, Doraiswamy JN, Malaiappan S. Herbs as an antioxidant arsenal for periodontal diseases. J IntercultEthnopharmacol. 2016 Jan 27;5(1):92-6. PubMed PMID: 27069730.
[21]. Thamaraiselvan M, Elavarasu S, Thangakumaran S, Gadagi JS, Arthie T. Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian SocPeriodontol. 2015 Jan-Feb;19(1):66-71. PubMed PMID: 25810596.
[22]. Thangaraj SV, Shyamsundar V, Krishnamurthy A, Ramani P, Ganesan K, Muthuswami M, et al. Molecular Portrait of Oral Tongue Squamous Cell Carcinoma Shown by Integrative Meta-Analysis of Expression Profiles with Validations. PLoS One. 2016 Jun 9;11(6):e0156582. PubMed PMID: 27280700.
[23]. Ponnulakshmi R, Shyamaladevi B, Vijayalakshmi P, Selvaraj J. In silico and in vivo analysis to identify the antidiabetic activity of beta sitosterol in adipose tissue of high fat diet and sucrose induced type-2 diabetic experimental rats. ToxicolMech Methods. 2019 May;29(4):276-290. PubMed PMID: 30461321.
[24]. Ramakrishnan M, Bhurki M. Fluoride, fluoridated toothpaste efficacy and its safety in children-review. Int J Pharm Res. 2018 Oct 1;10(04):109-4.
[25]. Shulman JD. Prevalence of oral mucosal lesions in children and youths in the USA. Int J Paediatr Dent. 2005 Mar;15(2):89-97. PubMed PMID: 15790365.
[26]. Baricevic M, Mravak-Stipetic M, Majstorovic M, Baranovic M, Baricevic D, Loncar B. Oral mucosal lesions during orthodontic treatment. Int J Paediatr Dent. 2011 Mar;21(2):96-102. PubMed PMID: 21121986.
[27]. Favia G, Limongelli L, Tempesta A, Maiorano E, Capodiferro S. Oral lesions as first clinical manifestations of Crohn's disease in paediatric patients: a report on 8 cases. Eur J Paediatr Dent. 2020 Mar;21(1):66-69. PubMed PMID: 32183532.
[28]. Hong CHL, Dean DR, Hull K, Hu SJ, Sim YF, Nadeau C, et al. World Workshop on Oral Medicine VII: Relative frequency of oral mucosal lesions in children, a scoping review. Oral Dis. 2019 Jun;25Suppl 1:193-203. PubMed PMID: 31034120.
[29]. Oral Mucosal Space/Surface Lesions. Diagnostic Imaging: Oral and Maxillofacial. 2017:9269.
[30]. Reichart PA. Oral mucosal lesions in a representative cross-sectional study of aging Germans. Community Dent Oral Epidemiol. 2000 Oct;28(5):390-8. PubMed PMID: 11014516.
[31]. Ali M, Sundaram D. Biopsied oral soft tissue lesions in Kuwait: a sixyear retrospective analysis. Med PrincPract. 2012;21(6):569-75. PubMed PMID: 22699793.
[32]. de Muñiz BR, Crivelli MR, Paroni HC. Clinical study of oral soft tissue lesions in boys in a children's home. Rev AsocOdontol Argent. 1981 Sep- Oct;69(7):405-8. PubMed PMID: 6950468.
[33]. Medina AC, Sogbe R, Gómez-Rey AM, Mata M. Factitial oral lesions in an autistic paediatric patient. Int J Paediatr Dent. 2003 Mar;13(2):130-7. PubMed PMID: 12605633.
[34]. Kovac-Kovacic M, Skaleric U. The prevalence of oral mucosal lesions in a population in Ljubljana, Slovenia. J Oral Pathol Med. 2000 Aug;29(7):331- 5. PubMed PMID: 10947249.
[35]. Jin X, Zeng X, Wu L. Oral Mucosal Lesions of Systemic Diseases. Case Based Oral Mucosal Diseases. 2018:169-97.
[36]. VijayashreePriyadharsini J. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol. 2019 Dec;90(12):1441-1448. PubMed PMID: 31257588.
[37]. J PC, Marimuthu T, C K, Devadoss P, Kumar SM. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin Implant Dent Relat Res. 2018 Aug;20(4):531-534. PubMed PMID: 29624863.
[38]. Ramesh A, Varghese S, Jayakumar ND, Malaiappan S. Comparative estimation of sulfiredoxin levels between chronic periodontitis and healthy patients - A case-control study. J Periodontol. 2018 Oct;89(10):1241-1248. PubMed PMID: 30044495.
[39]. Ramadurai N, Gurunathan D, Samuel AV, Subramanian E, Rodrigues SJL. Effectiveness of 2% Articaine as an anesthetic agent in children: randomized controlled trial. Clin Oral Investig. 2019 Sep;23(9):3543-3550. PubMed PMID: 30552590.
[40]. Sridharan G, Ramani P, Patankar S, Vijayaraghavan R. Evaluation of salivary metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Oral Pathol Med. 2019 Apr;48(4):299-306. PubMed PMID: 30714209.
[41]. Ezhilarasan D, Apoorva VS, Ashok Vardhan N. Syzygiumcumini extract induced reactive oxygen species-mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med. 2019 Feb;48(2):115-121. PubMed PMID: 30451321.
[42]. Mathew MG, Samuel SR, Soni AJ, Roopa KB. Evaluation of adhesion of Streptococcus mutans, plaque accumulation on zirconia and stainless steel crowns, and surrounding gingival inflammation in primary molars: randomized controlled trial. Clin Oral Investig. 2020 Sep;24(9):3275-3280. PubMed PMID: 31955271.
[43]. Samuel SR. Can 5-year-olds sensibly self-report the impact of developmental enamel defects on their quality of life? Int J Paediatr Dent. 2021 Mar;31(2):285-286. PubMed PMID: 32416620.
[44]. R H, Ramani P, Ramanathan A, R JM, S G, Ramasubramanian A, et al. CYP2 C9 polymorphism among patients with oral squamous cell carcinoma and its role in altering the metabolism of benzo[a]pyrene. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020 Sep;130(3):306-312. PubMed PMID: 32773350.
[45]. Chandrasekar R, Chandrasekhar S, Sundari KKS, Ravi P. Development and validation of a formula for objective assessment of cervical vertebral bone age. ProgOrthod. 2020 Oct 12;21(1):38. PubMed PMID: 33043408.
[46]. VijayashreePriyadharsini J, SmilineGirija AS, Paramasivam A. In silico analysis of virulence genes in an emerging dental pathogen A. baumannii and related species. Arch Oral Biol. 2018 Oct;94:93-98. PubMed PMID: 30015217.