Periodontal Disease: A Threat to Covid-19 Severity
BushraIjaz1*, Farzeen Tanwir1,2,3,4, Chander Kumar3, Saima Mazhar1, Syeda Natasha Zaidi1, SarahMoideen2,4, Areeba Dilshad5, Hira Ejaz6
1 Department of Dentistry,Bahria University Dental College, Pakistan.
2 Department of Dentistry, Fatima Jinnah Medical and Dental College, Pakistan.
3 Department of Dentistry, Dow University Health Sciences.
4 Department of Pharmacology, Fatima Jinnah Medical and Dental College, Pakistan.
5 Management Trainee officer, Department of Quality Assurance, Memon Medical Institute Hospital, Pakistan.
6 Malir Shed Hospital, Karachi, Pakistan.
*Corresponding Author
Bushra Ijaz,
Department of Dentistry, Bahria University Dental College, Pakistan.
E-mail: bushraijazz96@gmail.com
Received: September 14, 2021; Accepted: February 01, 2022; Published: April 01, 2022
Citation: Bushra Ijaz, Farzeen Tanwir, Chander Kumar, Saima Mazhar, Syeda Natasha Zaidi1, SarahMoideen, Areeba Dilshad, Hira Ejaz. Periodontal Disease: A Threat to Covid-19 Severity. Int J Dentistry Oral Sci. 2022;9(3):5269-5275. doi: dx.doi.org/10.19070/2377-8075-220001056
Copyright: Bushra Ijaz©2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
PD is an inflammatory illness affecting tissues that surrounds teeth. Co morbidities linked with PD are age, smoking, diabetes, hereditary, poor oral hygiene. These factors have been linked with severity of COVID-19, caused by virus namely corona virus “SARS-CoV-2.” As dysbiotic, inflammation and comorbidities disturb general well-being, it is probable that “periodontal status indicates the risk of complication of COVID-19”. Patients with COPD have a higher risk of provocation with COVID. Pregnancies can be complicated with co infection of SARS-CoV-2 with periodontal disease. Diabetic people also have PD probably because they are more prone to contract infections and higher chances to develop COVID-19 can also be increased with obesity and its consequences. Researchers have proved that aging is linked with PD and severe COVID-19 along with these factors. Smoking is the major risk factor in PD which leads to increase in enzyme ACE2; it’s an important element for development of covid-19. Chronic inflammation of airways had showed a relation between periodontal disease and asthma with enhanced ACE2 and TMPRSS 2 expression, increased SARS COV-2 infection susceptibility and Covid19 morbidity. Rheumatoid arthritis and liver disease also correspond to the development of covid-19 along with periodontitis. Patients who had history of liver disease have more chances to get SARS-COV-2 by means of the ACE-2 receptor. Degree of immunosuppression is thought to play a part in the vulnerability to SARS-CoV-2 infection. Hence, knowing the link between periodontal disease and COVID-19 severity, can aid in identifying the risk groups and create recommendation. The goal of the this review paper is to explain in detail the co-relation between periodontal disease and covid19.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Corona Virus; Periodontal Disease; Risk Factors; Covid19 Pandemic.
Introduction
“Periodontal disease” also referred to as “gum disease”. It is a set
of inflammatory illnesses distressing the tissues that surrounds
the teeth. In its initial stage, which is called gingivitis the gums
turn out to be red, swollen and might start bleeding. Its signs and
symptoms include: soreness or bleeding of gums while cleaning
teeth, bad breath, after brushing spitting out blood, swelling of
gums or formation of pockets between gums and teeth, in some
cases teeth may become mobile in later stages [1]. Periodontal
disease consists of gingivitis and periodontitis, the most common
disease of mankind. Its extreme form is distinguished by periodontal
ligament loss and destruction of adjacent alveolar bone.
Global prevalence of periodontal disease increased by 57.3%
from 1990 to 2010 [2]. Risk factors of periodontal disease include
diabetes, hereditary, and stress, poor oral hygiene, smoking, medication,
age [3].
Covid-19 disease is caused by a virus called novel “corona virus”,
SARS-CoV-2, it was found in Wuhan, China. Globally the
prevalence of patients infected with SARS-Cov-2 has exceeded
83,652 on 28 February 2020, and also number of mortality cases
of Covid-19 that is 2858 has been reported. On March 11,
2020, COVID-19 was professed a pandemic by the World Health
Organization (WHO). As of 27 March, 2020, a total of 103,942
confirmed cases with 1689 deaths in the United States reported globally, 27,324 expiries have been reported amongst 595,800
confirmed cases [5]. Uptillnow 85 403 patients in 57 territories/
countries are effected by Covid-19 and 2924 deaths in 9 countries
are reported. Comparatively death andillness and cases are
more reported in china than other countries. Evidence has reported
in Current epidemiological reports the transmission of
Covid-19 is form person to person in family and also in hospital
facility, the death ratiorate was highest 4.47% in Wuhan. A public
health emergency of international concern was constituted by
WHO when they declare SARS-COV-2outbreak [6]. Initial signs
and symptoms at incubation period, include: cough, fever, myalgia
and fatigue, however those who have lung disease, asthma
ranging moderate to severe, stern obesity, CKD (chronic kidney
disease), diabetes, and liver disease are as well at increased risk for
severe symptoms of COVID-19 [7]. The studies have shown that
those having chronic respiratory disease, diabetes, hypertension,
has higher risk of covid-19. In addition, age can be a risk factor
[8]. The goal of this article is to study Covid-19 and periodontal
disease at individual level and to assess the link between these two.
The importance of this review paper that periodontal disease, its
risk factor can be associated with Covid-19 severity. This paper
explain SEVERE COVID-19 ILLNESS AND PERIODONTAL
DISEASE SHARED RISK FACTORS that are Mouth-Covid
Connection, Chronic obstructive pulmonary disease (COPD),
Pregnancy, Inflammatory Markers, Diabetes,Obesity, Aging , Hypertension
and Cardiovascular, Oral dysbiosis- ETHIOPATHOGENIC,
Smoking, Asthma, Gender, Rheumatoid arthritis, Liver
Disease ended with HIV.
Hypothesis
“It is hypothesized that Periodontal disease can be associated with
increased risk of COVID-19 severity.”
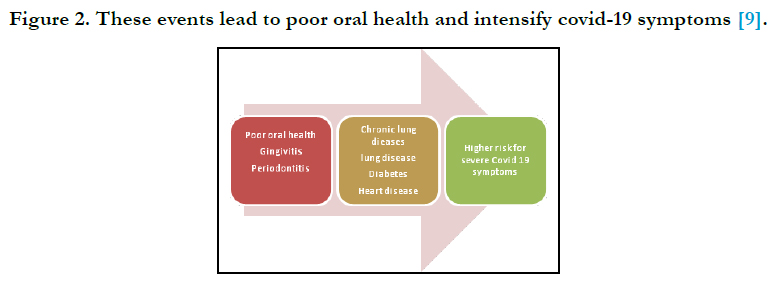
COVID-19 patients, who also have other co morbidities and risk
factor, also exacerbate the risk of periodontal disease. Until now,
evidence on oral health history counting periodontal status in patients
with intense COVID-19 infection has not been reported
[9].
Severe Covid-19 Illness And Periodontal Disease Shared Risk Factors
Mouth-Covid19 Connection
According to researcher, in Covid19 patient’s interleukin-6 is associated
with pulmonary consequences. Systemically and locally
cytokines are increase due to periodontitis, it also linked with respiratory
condition, lung function, pneumonia, and COPD. Therefore,
there is connection between covid-19, periodontitis and IL6
for this alliance the mechanism can be due to endothelial function,
gut dysbiosis, inflammation, and disturbance in IL-6 gene,
which also aggravate the inflammatory response, elevated levels
of pro inflammatory cytokines, such as IL-6, have been related
to periodontitis. In periodontal disease IL-6 is a known mediator.
In the dental literature, to reduce cytokine levels the ability
of nonsurgical periodontal therapy has been recognized. As a result,
periodontal disease can potentially protect COVID-infected
individuals by lowering IL-6 levels and inflammation. In adults
the frequency of periodontal disease is higher and the link between
respiratory problems, periodontal treatment IL-6 levels and
COVID-19 can be significant. In periodontal tissues, saliva, GCF
and serum in periodontitis patients, increase IL-6 levels have been
reported. The relationship between periodontitis and COVID-19
has various biological mechanisms. The pulmonary endothelium
and gut microbiome can be influence by periodontal disease because
of the dental bacterial load and systemic inflammation it
causes. Oral pathogens via aspiration of oral bacteria may also
enter the respiratory tract and boost the severity of the disease by
interrelate with the SARS-CoV-2 virus [10].
Chronic obstructive pulmonary disease (COPD)
Chronic obstructive pulmonary disease is persistent Lung disease
is caused by revelation to gases or elements that are toxic, in urbanized
states smoking being a major risk feature. COPD and PD
are associated as per different studies on the other hand; different factors can cofound this link such as smoking. Or age lately, it
was suggested that in older patients severe periodontitis has more
chances for COPD mortality or causality, the molecular mechanism
is unknown. It was stated that patients, when they present
COPD have a higher risk of provocation with COVID-19 and
those patients have a 4-fold greater risk to build up COVID-19
illness severely with preexisting COPD. It was proposed that patients
with chronic obstructive pulmonary disease ACE-2expression
are increased leads to increased risk. Hence, to recognize risk
groups to develop severe COVID-19, the link of PD with COPD
could be useful, as the risk of this affection importantly increased
by COPD [7].
Pregnancy
Pregnancy leads to many physiological changes, and to allow gestational
growth by suppressing the mother's immune system. It
was reported in studies that in pregnant women the susceptibility
of PD is because of exaggerated inflammatory response over the
last few years. In addition, it has been established that the gingival
response is triggered by high progesterone levels and leading to
dysbiosis. High periodontal pathogens development occurs in this
way, leading to medical manifestations in the protective and supporting
tissues of teeth. While, the connection among pregnancy
and PD is debatable, along with PD and pregnant women as they
may have complications during premature delivery or pregnancy,
some risk has been suggested. As long as worldwide the novel coronavirus
SARS-CoV-2 is increasing, some cases in pregnant women
of COVID19 have been confirmed. Although, women with
pregnancy are predispose to respiratory infectious disease due to
estrogen levels, high progesterone and immunosuppression, only
fewer than 10% prone to severe COVID-19 disease. But, prenatal
events such as, premature breakage of the membrane, preeclampsia,
low birth weight can be complicated by infection or it can
even cause death cases of COVID-19 with Vertical transmission
are not completely confirmed. Although the association between
periodontal disease and pregnancy is not clear, stating the fact.
Pregnancies in pregnant women can be complicated with coinfection
of SARS-CoV-2 with periodontal disease [7].
Inflammatory Markers
In Covid-19 infection anosmia and Aguesia are common finding
of patient however 20% of the patients develop serious illness
with 6% mortality rate which is mostly related with systemic diseases,
older age and immunosuppressant. Patients have elevated
levels of serum pro-inflammatory cytokines also chemokine including
IL1RA,IL1-b, IL2, IL6,IL7 IL8, IL9, IL10, MCP1 – 1a,
FGF2, GMCSF, GCSF, IFNc, TNFa and IP10, that lead to stimulate
infection severity. Dental specialists can get diseased easily
due to their straight revelation to blood and saliva [11].
During periodontitis, Low serum CD133+/KDR+ levels appear
to be associated with the likelihood of evolving forthcoming endothelial
dysfunction and CVD threat. Interestingly, these provocative
features of the host and disrupted immune-regulation
in PD have been extensively linked with development or severe
corona virus illness (COVID-19) [12].
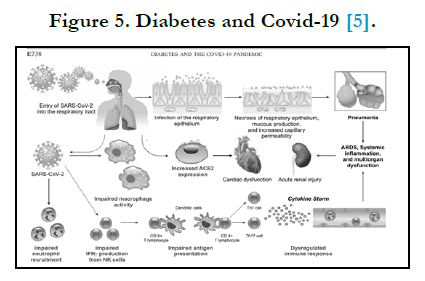
Diabetes
In older age, presence of hypertension, Diabetes Mellitus and
stern obesity (BMI 40 kg/m2) enhance illness and death in patients
of COVID-19 [5]. It can be difficult to treat diabetic patients with viral infection due to variations in plasma glucose levels because
of two reasons. Firstly, if the defensive system is compromised, it
is problematic to combat the infection and leading to prolonged
recovery period. Secondly, if levels of blood glucose are high the
virus may grow, similar to other respiratory disease; COVID-19 is
transmitted through air-droplets that are scattered when person
who is infected sneezes, cough and talks. Depending on the ecological
conditions the virus can continue to exist from a few hours
up to a few days [14]. Mechanisms that may enhance the liability
for COVID-19 patients with DM contain: 1) decreased viral clearance,
2) existence of CVD, 3) advanced affinity cellular binding
and efficient virus access 4) reduced function of T cell 5) enlarged
susceptibility to hyper infection and cytokine storm syndrome [5].
Individuals with diabetes are expected to have periodontal disease
PD, probably because they are more prone to contract infections.
It is considered a complication of diabetes. Those people
whose diabetes is not controlled are at risk. It was reported that
diabetes and periodontal disease are linked. PD makes it harder
for individuals who have diabetes to control their levels. Extreme
periodontal infection can expand glucose, adding to expanded
timeframes when the body capacities with a high glucose. This
puts individuals with diabetes at danger for periodontal difficulties
[15].
Obesity
With increasing prevalence yearly, almost 50 percent of the population
is obese or over weight. It is counted as an utmost risk factor
for developing periodontal disease after smoking. Alteration
of microbial composition of periodontal can occur with Obesity
and is linked with an increase in periodontal pathogens. A systemic
inflammation state is the main consequences of obesity in
individuals if PD is established and accompanied by the proinflammatory
cytokines and bacterial products dissemination [16].
The threat to progress severe COVID-19 disease can be increased
with obesity and its consequences. Factors drawn in this could
be functional capacity, reduced expiratory reserve capacity, and
respiratory system acquiescence. Moreover, reported in obesity
the augmented inflammatory factors could contribute to intensify
the development of severe COVID-19 and the response of the
patient [17]. Periodontal Disease, by dissemination of bacterial
products could add to the intensification of a complete inflammatory
response and as a cause of inflammatory cytokines in
individuals with COVID-19, consequently leading to the disease
aggravation. Furthermore, the people with PD and obesity have
abigger threat of developing extreme COVID-19 possibly [7].
Aging
Adults are more prone to periodontal disease because of additional
risk factors, presence of chronic diseases, delayed dental
treatment, poor oral hygiene and use of medication. Smoking can
also amend gingival micro biota and cause periodontal disease and
respiratory tract infection [18-20]. Above 65 years of age, people
are likelihood to severe COVID-19 illness [7]. Other factor which
is important is immunity and that is not as strong as young ones
[21]. Hence it is proved that aging factor is linked with PD and
severe COVID-19.
Hypertension and Cardiovascular
In PD, Chronic inflammatory response is induce by bacterial
species that lie in sub gingival bio film by encouraging the production
of cytokines “IL-1, IL-6, IL-8 and TNF-a” [22]. Which
increase and regulate levels of (CRP) C-reactive protein. High
density CRP is a marker present in cardiovascular diseases and
also in periodontitis where is increased by large production of
cytokines [23-25]. Hypertension represents one of the main co
morbidities to the COVID-19 patients. CVD is also an important
risk factor;epidemiological studies have established a link between
periodontitis, cardiovascular disease and hypertension [26].
Oral dysbiosis - ETHIOPATHOGENIC
When the bacteria of oral micro biota are imbalanced it is called
oral dysbiosis [4]. It is also associated with oral disease like periodontitis,
candidiasis etc. whereas, oral microbes including Porphyromonas
gingivalis, Salmonella, Prevotella intermedia and others
involved in periodontitis [26]. Impaired oral health is reported in
patients who are hospitalized with severe Covid-19 illness oron
some lifesaving mechanism or intubation. Moreover other factors
like, lack of oral hygiene, use of drugs that attack the SARSCoV-2
virus, and other co morbidities can produce dysbiosis and could
trigger oral diseases like periodontal disease [21]. In oral mucosa
levels of ACE2 are increased in covid-19 patients due to presence
of fusibacterium, Prevotella hence it proved the link between
Covid-19 severity and periodontitis [26].
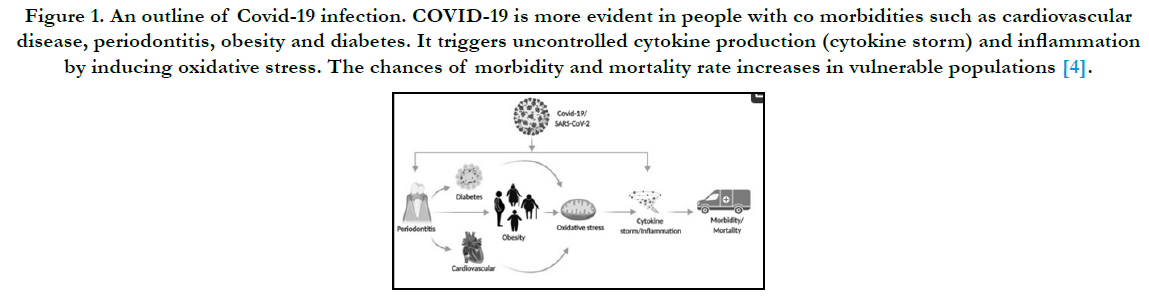
Figure 1. An outline of Covid-19 infection. COVID-19 is more evident in people with co morbidities such as cardiovascular disease, periodontitis, obesity and diabetes. It triggers uncontrolled cytokine production (cytokine storm) and inflammation by inducing oxidative stress. The chances of morbidity and mortality rate increases in vulnerable populations [4].
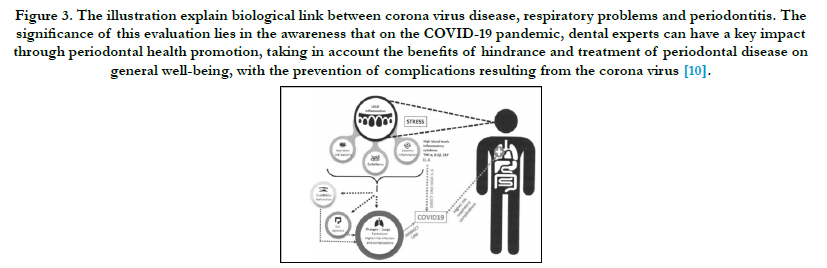
Figure 3. The illustration explain biological link between corona virus disease, respiratory problems and periodontitis. The significance of this evaluation lies in the awareness that on the COVID-19 pandemic, dental experts can have a key impact through periodontal health promotion, taking in account the benefits of hindrance and treatment of periodontal disease on general well-being, with the prevention of complications resulting from the corona virus [10].
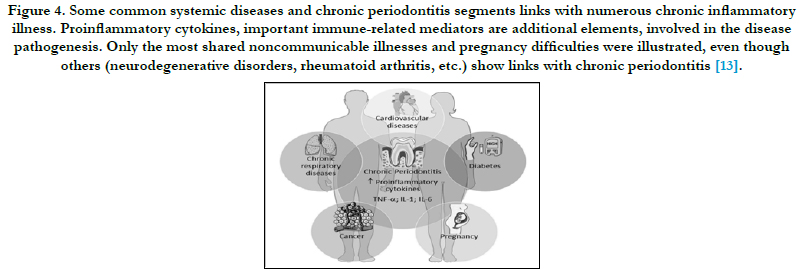
Figure 4. Some common systemic diseases and chronic periodontitis segments links with numerous chronic inflammatory illness. Proinflammatory cytokines, important immune-related mediators are additional elements, involved in the disease pathogenesis. Only the most shared noncommunicable illnesses and pregnancy difficulties were illustrated, even though others (neurodegenerative disorders, rheumatoid arthritis, etc.) show links with chronic periodontitis [13].
Smoking
In periodontal disease smoking is the major risk factor, because of which periodontal treatment is also affected, smoking impede host immune response, periodontal tissue activity and powerful microenvironment to combat against pathogen. Whereas expression of angiotensin converting enzyme ACE2 is increased by smoking and it is also a major factor for development of covid- 19, being more probable about 1.4 times to have severe symptoms of COVID-19 [27].
Asthma
Chronic inflammation of airways occur in asthma and research showed a relation between periodontal disease and asthma [27- 29]. In adults it might bea threat element for periodontal illness however it can be due to genetics, inflammatory factors or dysbiosis [7]. It was stated that asthma might be a peril for severe COVID 19 disease. In COVID 19 patients, asthma had low prevalence [30]. In thispatient with enhanced ACE2 and TMPRSS 2 (Tran’s membrane protease, serine 2) expression, increased SARS COV-2 infection vulnerability and Covid19 morbidity is indicated. Along these findings could suggest that periodontal disease with asthma could referas a strong risk for Covid-19 development [31].
Gender
It is stated in research studies that, women are less prone to the development of periodontal disease as compared to men [30, 32. 33]. Most likely immune function, environment and behavioral factor are involved to explain this difference [34]. Likewise in Covid19 illness it was suggested that in men there are more chances then women. Immunity reaction to SARS COV-2 may explicit this discrepancy therefore its alliance with immunologic factors and gender periodontal disease might show the risk of Covid-19 [35-37].
Rheumatoid arthritis
It is reported in studies that people with rheumatoid arthritis and periodontal disease have weaken systemic status, RA is a chronic inflammatory disease that has been allied with periodontal disease its prevalence is 0.3 to 1 % . Its mechanism is unknown. However Porphyromonas gingivalis produces an enzyme that causes citrullination [38]. Synovial fluid has been found to contain periodontal bacteria [39]. Patient with rheumatoid arthritis are more prone to communicable diseases and death rates are increased due to bronchopulmonary infection [40]. Relationship among rheumatoid arthritis, periodontal disease, bacterial and inflammatory systems could influence the result in people having COVID-19 [41].
Liver Disease
Relationship has been found among periodontal and liver disease .Nonalcoholic Fatty Liver Disease (NAFLD), liver cirrhosis (LC), hepatocellular carcinoma (HCC), have 20-30% prevalence all throughout world. Significantly transplantation of liver is related with PD, as to stay away from sepsis by period on topathogens the person with disease must be inspected by an oral expert before LT [42-45]. Subgingival microbial niches promote periodontal tissues inflammation and cytokines “IL-1ß, IL-6, IL-10, IL12, and TNF-a and INF-?”that participate in the development of liver disease. It is likewise associated with Covid-19; patients who had history of liver disease are more liable to SARS-COV 2 as by means of the ACE-2 receptor as virus binds to hepatocytes and cholangiocytes [46]. Therefore patients with periodontal disease and liver diseases aid to discover those individuals who are at risk for COVID-19.
HIV
Immune-compromised patients have more chances of systemic and oral indexes [47, 48]. According to researcher periodontal disease is linked with HIV because it is a chronic inflammation [49]. Some articles also stated that in prevalence of periodontal disease HIV is an important factor [50]. Whereas HIV is also associated with Covid-19 and the degree of immunosuppression is thought to show a part in the vulnerability to SARS-CoV-2 infection [51].
Complications
According to an international team of dental researchers, Covid-
19 patients whose reports are positive if they suffered from
periodontitis and are hospitalized are far more probable to die of
respiratory failure. Patients who are Hospitalized with COVID-19
have high interleukin (IL-6) levels, which is a harmful protein produced
by periodontitis, are at considerably larger risk of suffering
life-threatening respiratory problems and are probably in critical
condition and unable to breathe without the ventilator. In recent
study, it is shown that in COVID-19 patients’ who had gum disease
inflammation in their body were clearly higher as compared
to those who did not. The results of the study suggest that the
oral cavity inflammation possibly will unlock the door to the corona
virus being more aggressive [52].
Scientific Contribution: This paper contribute scientificallyas
until now, evidence on oral health history counting periodontal
status in patients with intense COVID-19 infection has not been
reported.
Conclusion
PD could be allied with severe COVID-19. Many researchers
have shown a potential connection between periodontal disease
and coronavirus. The bacteria involved in covid-19 is seems to
be similar to the ones from the oral cavity. Gingival Tissue that is
affected from periodontitis represent a board entry point for viral
or bacterial pathogens such as “SARS-COV-2’. Individuals with
severe medical conditions such as, respiratory disease, diabetes
can be a major risk factor for the development of covid-19 as well
as periodontitis since both of these share same risk factors which
itself is an indicator for the urge of immediate attention. Diagnosis
of SARS-COV 2 in an individual along with the presence of
periodontitis can worsen the condition and effects.
Future Recommendation
1. Further studies should be done to reveal the unknown mechanism
between Covid-19 and periodontal disease.
2. Individual having co morbidities like diabetes, respiratory disease,
HIV, hypertension and other above mentioned, should take
additional precautions.
3. Oral hygiene should be maintained especially in this pandemic
to lower the risk of covid-19, since a possible link between Covid-
19 and periodontitis is observed.
4. Studies should be conducted to assess the risk of Covid-19
transmission while going through aerosols procedures.
5. Public awareness sessions should be planned on how to maintain
your oral health since it could play a key role in battling the
virus it is stated that if good oral health is maintained , particularly “healthy gums” risk of developing the most serious complications
of corona virus are limited .
6. Further researches are necessary to identify the factors that are
still unknown and can lead to the complications of Covid-19.
7. Periodontal education should be provided along with other
forms of health education.
8. Further, clinical trials which can evaluate periodontal status in
individuals suffering from covid-19 are required to conclude the
correct mechanism as already mentioned that poor oral hygiene
can elevate the Covid-19 infection.
9. Relationship between COVID-19 illness and smoking is not
fully understandable;therefore, further research is important to
identify the danger of smokers and succession of Disease.
References
-
[1]. Periodontal disease - Wikipedia [Internet]. En.wikipedia.org. 2021 Available
from: https://en.wikipedia.org/wiki/Periodontal_disease
[2]. Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J ClinPeriodontol. 2017 May;44(5):456-462. Pub- Med PMID: 28419559.
[3]. Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci (Qassim). 2017 Apr- Jun;11(2):72-80. PubMed PMID: 28539867.
[4]. Coke CJ, Davison B, Fields N, Fletcher J, Rollings J, Roberson L, Challagundla KB, Sampath C, Cade J, Farmer-Dixon C, Gangula PR. SARSCoV- 2 Infection and Oral Health: Therapeutic Opportunities and Challenges. J Clin Med. 2021 Jan 5;10(1):156. PubMed PMID: 33466289.
[5]. Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J PhysiolEndocrinolMetab. 2020 May 1;318(5):E736-E741. PubMed PMID: 32228322.
[6]. Lai CC, Wang CY, Wang YH, Hsueh SC, Ko WC, Hsueh PR. Global epidemiology of coronavirus disease 2019 (COVID-19): disease incidence, daily cumulative index, mortality, and their association with country healthcare resources and economic status. Int J Antimicrob Agents. 2020 Apr;55(4):105946. PubMed PMID: 32199877.
[7]. Pitones-Rubio V, Chávez-Cortez EG, Hurtado-Camarena A, González- Rascón A, Serafín-Higuera N. Is periodontal disease a risk factor for severe COVID-19 illness? Med Hypotheses. 2020 Nov;144:109969. PubMed PMID: 32592918.
[8]. Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020 Mar 26;368:m1198. PubMed PMID: 32217618.
[9]. Botros N, Iyer P, Ojcius DM. Is there an association between oral health and severity of COVID-19 complications? Biomed J. 2020 Aug;43(4):325-327. PubMed PMID: 32713780.
[10]. Molayem S, Pontes CC. The Mouth-COVID Connection: H-6 Levels in Periodontal Disease—Potential Role in COVID-19-Related Respiratory Complications. Medicinastomatologica. 2020 Dec 29;57(4):68-80.
[11]. Kara C, Çelen K, Dede FÖ, Gökmenoglu C, Kara NB. Is periodontal disease a risk factor for developing severe Covid-19 infection? The potential role of Galectin-3. ExpBiol Med (Maywood). 2020 Oct;245(16):1425- 1427. PubMed PMID: 32838557.
[12]. Utomo H, Wijaksana IK, Prahasanti C. Porphyromonasgingivalis in Periodontitis: A Forgotten Enemy Behind COVID-19 Pandemic. Dental Hypotheses. 2021 Jan 1;12(1):28.
[13]. Cardoso EM, Reis C, Manzanares-Céspedes MC. Chronic periodontitis, inflammatory cytokines, and interrelationship with other chronic diseases. Postgrad Med. 2018 Jan;130(1):98-104. PubMed PMID: 29065749.
[14]. Diabetes A, diabetes W, diabetes C. COVID-19 and diabetes [Internet]. Idf.org. 2021 Available from: https://www.idf.org/aboutdiabetes/what-isdiabetes/ covid-19-and-diabetes/1-covid-19-and-diabetes.html
[15]. Periodontology A. Diabetes and Periodontal Disease | Perio.org [Internet]. Perio.org. 2021 [cited 1 July 2021]. Available from: https://www.perio.org/ consumer/gum-disease-and-diabetes.html
[16]. Suvan JE, Finer N, D'Aiuto F. Periodontal complications with obesity. Periodontol 2000. 2018 Oct;78(1):98-128. PubMed PMID: 30198136.
[17]. Dietz W, Santos-Burgoa C. Obesity and its Implications for COVID-19 Mortality. Obesity (Silver Spring). 2020 Jun;28(6):1005. PubMed PMID: 32237206.
[18]. Lamont RJ, Hajishengallis G. Polymicrobial synergy and dysbiosis in inflammatory disease. Trends Mol Med. 2015 Mar;21(3):172-83. PubMed PMID: 25498392.
[19]. Sampson V. Oral hygiene risk factor. Br Dent J. 2020 Apr;228(8):569. Pub- Med PMID: 32332938.
[20]. Ebersole JL, Graves CL, Gonzalez OA, Dawson D 3rd, Morford LA, Huja PE, et al. Aging, inflammation, immunity and periodontal disease. Periodontol 2000. 2016 Oct;72(1):54-75. PubMed PMID: 27501491.
[21]. Ebersole JL, Dawson DA 3rd, EmecenHuja P, Pandruvada S, Basu A, Nguyen L, et al. Age and Periodontal Health - Immunological View. Curr Oral Health Rep. 2018 Dec;5(4):229-241. PubMed PMID: 30555774.
[22]. Soory M. Chronic periodontitis as a risk marker for systemic diseases with reference to cardiometabolic disorders: common pathways in their progression. Immunology and Immunogenetics Insights. 2010 Jan;2:III-S5795.
[23]. Leong XF, Ng CY, Badiah B, Das S. Association between hypertension and periodontitis: possible mechanisms. ScientificWorldJournal. 2014 Jan 8;2014:768237. PubMed PMID: 24526921.
[24]. Paraskevas S, Huizinga JD, Loos BG. A systematic review and meta-analyses on C-reactive protein in relation to periodontitis. J ClinPeriodontol. 2008 Apr;35(4):277-90. PubMed PMID: 18294231.
[25]. Miyashita H, Honda T, Maekawa T, Takahashi N, Aoki Y, Nakajima T, et al. Relationship between serum antibody titres to Porphyromonasgingivalis and hs-CRP levels as inflammatory markers of periodontitis. Arch Oral Biol. 2012 Jun;57(6):820-9. PubMed PMID: 22172404.
[26]. Martu MA, Maftei GA, Sufaru IG, Jelihovschi I, Luchian I, Hurjui L,et al. COVID-19 and periodontal disease—Ethiopathogenic and clinical implications. Rom J Oral Rehabil. 2020 Oct;12(4).
[27]. Soledade-Marques KR, Gomes-Filho IS, da Cruz SS, Passos-Soares JS, Trindade SC, Cerqueira EMM, et al. Association between periodontitis and severe asthma in adults: A case-control study. Oral Dis. 2018 Apr;24(3):442- 448. PubMed PMID: 28833877.
[28]. Lee SW, Lim HJ, Lee E. Association Between Asthma and Periodontitis: Results From the Korean National Health and Nutrition Examination Survey. J Periodontol. 2017 Jun;88(6):575-581. PubMed PMID: 28398111.
[29]. Moraschini V, Calasans-Maia JA, Calasans-Maia MD. Association between asthma and periodontal disease: A systematic review and meta-analysis. J Periodontol. 2018 Apr;89(4):440-455. PubMed PMID: 28871892.
[30]. Haytac MC, Ozcelik O, Mariotti A. Periodontal disease in men. Periodontol 2000. 2013 Feb;61(1):252-65. PubMed PMID: 23240953.
[31]. Peters MC, Sajuthi S, Deford P, Christenson S, Rios CL, Montgomery MT, et al. COVID-19 Related Genes in Sputum Cells in Asthma: Relationship to Demographic Features and Corticosteroids. Am J RespirCrit Care Med [Internet]. 2020 Apr 29;rccm.202003-0821OC. Available from: https:// www.atsjournals.org/doi/10. 1164/rccm.202003-0821OC.
[32]. Meisel P, Eremenko M, Holtfreter B, Völzke H, Kocher T. The sex paradox in the interplay between periodontitis, obesity, and serum C-reactive protein: Data from a general population. J Periodontol. 2019 Dec;90(12):1365- 1373. PubMed PMID: 31343076.
[33]. Shiau HJ. Periodontal disease in women and men. Current Oral Health Reports. 2018 Dec;5(4):250-4.
[34]. Ioannidou E. The Sex and Gender Intersection in Chronic Periodontitis. Front Public Health. 2017 Aug 4;5:189. PubMed PMID: 28824898. [35]. Simoni M, Hofmann M. The COVID-19 pandemics: shall we expect andrological consequences? A call for contributions to ANDROLOGY. Andrology [Internet]. 2020 Apr 17;andr.12804.Availablefrom:https://onlinelibrary. wiley.com/doi/ abs/10.1111/andr.12804. [36]. Conti P, Younes A. Coronavirus COV-19/SARS-CoV-2 affects women less than men: clinical response to viral infection. J BiolRegulHomeost Agents. 2020 March-April,;34(2):339-343. PubMed PMID: 32253888.
[37]. Yi Y, Lagniton PNP, Ye S, Li E, Xu RH. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci. 2020 Mar 15;16(10):1753-1766. PubMed PMID: 32226295.
[38]. de Molon RS, Rossa C Jr, Thurlings RM, Cirelli JA, Koenders MI. Linkage of Periodontitis and Rheumatoid Arthritis: Current Evidence and Potential Biological Interactions. Int J Mol Sci. 2019 Sep 13;20(18):4541. PubMed PMID: 31540277.
[39]. Ogrendik M. Rheumatoid arthritis is linked to oral bacteria: etiological association. Mod Rheumatol. 2009;19(5):453-6. PubMed PMID: 19554393.
[40]. Moen K, Brun JG, Valen M, Skartveit L, Eribe EK, Olsen I, et al. Synovial inflammation in active rheumatoid arthritis and psoriatic arthritis facilitates trapping of a variety of oral bacterial DNAs. ClinExpRheumatol. 2006 Nov-Dec;24(6):656-63. PubMed PMID: 17207381.
[41]. Lamont RJ, Koo H, Hajishengallis G. The oral microbiota: dynamic communities and host interactions. Nat Rev Microbiol. 2018 Dec;16(12):745- 759. PubMed PMID: 30301974.
[42]. Han P, Sun D, Yang J. Interaction between periodontitis and liver diseases. Biomed Rep. 2016 Sep;5(3):267-276. PubMed PMID: 27588170.
[43]. Weintraub JA, Lopez Mitnik G, Dye BA. Oral Diseases Associated with Nonalcoholic Fatty Liver Disease in the United States. J Dent Res. 2019 Oct;98(11):1219-1226. PubMed PMID: 31369716.
[44]. Nagao Y, Tanigawa T. Red complex periodontal pathogens are risk factors for liver cirrhosis. Biomed Rep. 2019 Nov;11(5):199-206. PubMed PMID: 31632667.
[45]. Kim JY, Lee GN, Song HC, Park YM, Ahn YB, Han K, et al. Association between Fatty Liver Index and Periodontitis: the Korea National Health and Nutrition Examination Survey. Sci Rep. 2020 Mar 2;10(1):3805. PubMed PMID: 32123238.
[46]. Pirola CJ, Sookoian S. SARS-CoV-2 virus and liver expression of host receptors: Putative mechanisms of liver involvement in COVID-19. Liver Int. 2020 Aug;40(8):2038-2040. PubMed PMID: 32352224.
[47]. Szczawinska-Poplonyk A, Gerreth K, Breborowicz A, Borysewicz-Lewicka M. Oral manifestations of primary immune deficiencies in children. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 2009 Sep;108(3):e9-20. PubMed PMID: 19596208.
[48]. Peacock ME, Arce RM, Cutler CW. Periodontal and other oral manifestations of immunodeficiency diseases. Oral Dis. 2017 Oct;23(7):866-888. PubMed PMID: 27630012.
[49]. Noguera-Julian M, Guillén Y, Peterson J, Reznik D, Harris EV, Joseph SJ, et al. Oral microbiome in HIV-associated periodontitis. Medicine (Baltimore). 2017 Mar;96(12):e5821. PubMed PMID: 28328799.
[50]. Goldberg BE, Mongodin EF, Jones CE, Chung M, Fraser CM, Tate A, et al. The Oral Bacterial Communities of Children with Well-Controlled HIV Infection and without HIV Infection. PLoS One. 2015 Jul 6;10(7):e0131615. PubMed PMID: 26146997.
[51]. Ballester-Arnal R, Gil-Llario MD. The Virus that Changed Spain: Impact of COVID-19 on People with HIV. AIDS Behav. 2020 Aug;24(8):2253-2257. PubMed PMID: 32342259.
[52]. Gum disease linked to COVID-19 complications [Internet]. Medicalxpress. com. 2021 [cited 27 June 2021]. Available from: https://medicalxpress. com/news/2021-02-gum-disease-linked-covid-complications.html