Socket Preservation - A Case Report
Bhargavi Sheth1, Poonam Rai1*, Devanand Shetty2, Kushal Shah1
1 Post Graduate Student, Department of Periodontics and Oral Implantology, D Y Patil School of Dentistry, Navi Mumbai, India.
1 Professor, Department of Periodontics and Oral Implantology, D Y Patil School of Dentistry, Navi Mumbai, India.
2 Professor & Head of Department, Department of Periodontics and Oral Implantology, D Y Patil School of Dentistry, Navi Mumbai, India.
*Corresponding Author
Dr. Poonam Rai,
Professor, Department of Periodontics and Oral Implantology, D Y Patil School of Dentistry, Navi Mumbai, India.
Tel: +91 98920 19346
E-mail: drpoonamm.singh@gmail.com
Received: December 13, 2021; Accepted: February 12, 2022; Published: February 18, 2022
Citation: Bhargavi Sheth, Poonam Rai, Devanand Shetty, Kushal Shah. Socket Preservation - A Case Report. Int J Dentistry Oral Sci. 2022;9(2):5246-5248. doi: dx.doi.org/10.19070/2377-8075-220001052
Copyright: Poonam Rai©2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Post the extraction of a tooth, there is alveolar bone resorption in that area, which leads to further complications in terms of prosthetic and surgical situations when the tooth needs to be replaced. To serve this problem of dimensional reduction of alveolar bone around the missing tooth, socket preservation offers an ideal solution. This case report discusses the extraction of a root-canal treated right mandibular molar which was extracted atraumatically by hemisectioning the tooth and preserving the inter-radicular bone followed by grafting the socket with demineralized freeze dried bone allograft and PerioCol membrane. After a healing period of 3-months a CBCT scan was done to evaluate the regeneration of the grafted site and bone fill. This brings us to a conclusion that grafting the socket post-extraction, helps reduce the dimensional changes for better prosthetic rehabilitation.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Socket Preservation; Demineralized Freeze Dried Bone Allograft; Periocol Membrane.
Introduction
Each time a tooth is lost due to caries or any other cause; there are
morphological and dimensional changes in the alveolar bone surrounding
that region. These changes are observed both in the vertical
and horizontal directions [1]. Bone remodelling takes place
in the initial 3-6 months after the tooth is extracted [2]. This is a
critical phase wherein maximum dimensional changes are expected.
Therefore, preservation of the alveolar socket post extracting
the tooth plays an important role in preventing the dimensional
changes. This further impacts the placement of implant in that
region without compromising the implant dimensions hence resulting
in long-term success of the implant. If the socket is compressed
after tooth extraction, there may be severe bone defects
near the socket, which will hamper the further prosthetic rehabilitation
of that area.
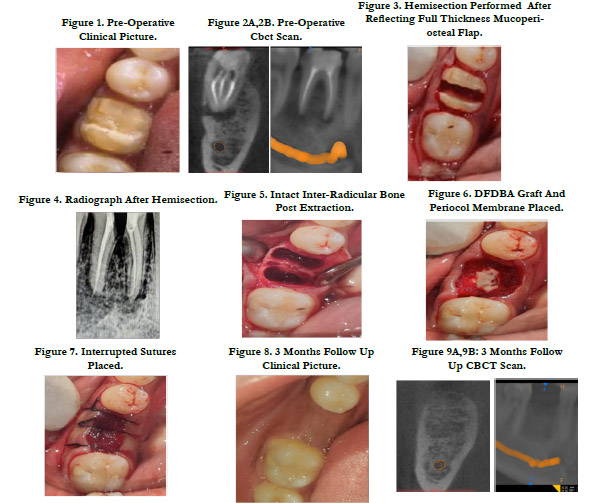
Case Report
A 23-year-old male patient reported to the department with a
complaint of a fractured tooth in the lower right back region of
the jaw. The patient was systemically healthy. He gave a history
of root canal treatment in relation to the same tooth. On clinical
examination it was found that there was insufficient crown
height (FIG 1). The patient was advised a CBCT scan from another
department to evaluate the cause of pain, which revealed
a fracture line along with some periapical pathology in relation
to tooth number 46 (FIG 2a,2b). The treatment plan comprising
of an atraumatic tooth extraction by hemisectioning the tooth,
followed by socket preservation with demineralized freeze dried
bone allograft and PerioCol membrane, was discussed with the
patient. An informed consent was obtained from the patient followed
by scaling and root planing 2 weeks prior to the procedure.
On the day of the procedure local anesthesia (2% lignocaine with
1:80,000 adrenaline) was administered to the patient. A full thickness
mucoperiosteal flap was reflected beyond the mucogingival
junction and the tooth was hemisectioned with the help of an
airotor and a straight diamond bur (FIG 3). A radiograph was taken
to evaluate whether or not the vertical groove of hemisection
has reached the furcation of the tooth (FIG 4). Once the desired
depth of hemisection was attained, Periotomes were used for
extracting the tooth atraumatically while simultaneously preserving
the inter-radicular bone. Curettage of the extraction socket
was done using a spoon excavator and the socket was rinsed with sterile saline(FIG 5). PerioCol membrane was adapted around
the socket after which demineralized freeze dried bone allograft
(500-1000 micron particle size) was used to graft the socket upto
an extent such that the membrane would not collapse into the
socket (FIG 6). The flap was then coronally advanced and sutured
using interrupted sutures to attain maximum closure (FIG
7). The entire procedure was performed under antibiotic coverage
(Amoxicillin 500mg) post-operative medication comprising
of Cap. Amox 500 TDS for 5 days , Metronidazole 400 mg TDS
for 5 days and Ibuprofen 400 mg BID for 3 days were prescribed.
Suture removal was done after 2 weeks. After 1 month the patient
was recalled and evaluated for healing which was satisfactory. Patient
was recalled after 3 months for clinical and CBCT scan to
evaluate the bone fill. On CBCT evaluation it was seen that there
was minimum amount of radiolucency at the grafted site (FIG
9a, 9b). Clinical examination of the surgical site showed complete
soft tissue healing (FIG 8).
Discussion
Studies have quoted the use of guided bone regeneration techniques
in socket preservations gives better results, especially
when a membrane is used [3]. In this case a socket preservation
was done along with raising a full thickness mucoperiosteal flap,
there are certain known disadvantaged of raising a flap during
socket preservation as there is difficulty in attaining primary closure
along with increased tension in the flap and reduction of
vestibular depth. To overcome these drawbacks newer techniques
are used which are more conservative as a flap reflection is not
required [4, 5]. The grafting material should be biocompatible,
osteoconductive and osteoinductive [6]. Xenografts and alloplasts
with or without a membrane have shown adequate results for
socket preservation. Few studies have also used a combination
of allografts; however, there are negligible differences in changes
to alveolar ridge dimensions when comparing DFDBA to combination
allografts [7]. DFDBA has been extensively used in periodontal
treatment and has proven to be safe, and it induces the
formation of new bone. DFDBA is both osteoconductive and
osteoinductive in nature. Use of DFDBA has been used in several
animal studies and has proven that it could stimulate the formation
of new bone by osteoinduction. DFDBA also acts as a scaffold
for osteoconduction [8]. Among all the available membranes,
collagen membrane was preferred as it has a high biocompatibility
and haemostatic activity that facilitates clot formation and stabilizes
the wound. Collagen has a high chemotactic function for
fibroblasts. This promotes cell migration, and primary wound
coverage [9]. In this case the ridge dimensions were preserved because of the use of DFDBA and PerioCol membrane for a
better outcome.
Conclusion
Socket preservation done with the help of guided bone regeneration
technique can minimize bone resorption and aid in further
placement of implants.
References
-
[1]. Schropp L, Kostopoulos L, Wenzel A. Bone healing following immediate
versus delayed placement of titanium implants into extraction sockets: a
prospective clinical study. Int J Oral Maxillofac Implants. 2003 Mar-
Apr;18(2):189-99.Pubmed PMID: 12705296.
[2]. Kanwar S, Shetty A, Shetty D, Wadkar P. Socket preservation and reconstruction:
A case report with follow up of 9 months. Int. J. Appl. Dent.
Sci.2021.
[3]. Vignoletti F, Matesanz P, Rodrigo D, Figuero E, Martin C, Sanz M. Surgical
protocols for ridge preservation after tooth extraction. A systematic review.
Clin Oral Implants Res. 2012 Feb;23 Suppl 5:22-38.Pubmed PMID:
22211304.
[4]. Sclar AG. Preserving alveolar ridge anatomy following tooth removal in
conjunction with immediate implant placement. The Bio-Col technique.
Atlas Oral Maxillofac Surg Clin North Am. 1999 Sep;7(2):39-59.Pubmed
PMID: 11905323.
[5]. Landsberg CJ, Bichacho N. A modified surgical/prosthetic approach for optimal
single implant supported crown. Part I--The socket seal surgery. Pract
Periodontics Aesthet Dent. 1994 Mar;6(2):11-7.Pubmed PMID: 7670061.
[6]. Yip I, Ma L, Mattheos N, Dard M, Lang NP. Defect healing with various
bone substitutes. Clin. Oral Implants Res. 2015 May;26(5):606-14.
[7]. Horowitz R, Holtzclaw D, Rosen PS. A review on alveolar ridge preservation
following tooth extraction. J. Evid. Based Dent. Pract. 2012 Sep
1;12(3):149-60.
[8]. Kukreja BJ, Dodwad V, Kukreja P, Ahuja S, Mehra P. A comparative evaluation
of platelet-rich plasma in combination with demineralized freeze-dried
bone allograft and DFDBA alone in the treatment of periodontal intrabony
defects: A clinicoradiographic study. J Indian Soc Periodontol. 2014
Sep;18(5):618-23.Pubmed PMID: 25425824.
[9]. Zubillaga G, Von Hagen S, Simon BI, Deasy MJ. Changes in alveolar bone
height and width following post-extraction ridge augmentation using a fixed
bioabsorbable membrane and demineralized freeze-dried bone osteoinductive
graft. J Periodontol. 2003 Jul;74(7):965-75.Pubmed PMID: 12931758.