Dental Stem Cells- Application In Dental Research And Therapeutic Implication
Deepika Rathna1, Monica Charlotte Solomon2*
1 Junior Research Scientist, Translational Health Science and Technology Institute, NCR Biotech Science Cluster 3rd Milestone, Faridabad - Gurgaon Rd, Expressway, Faridabad, Haryana 121001, India.
2 Professor, Department of Oral Pathology and Microbiology, Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal 576104, Karnataka, India.
*Corresponding Author
Dr. Monica Charlotte Solomon, MDS, PhD,
Professor, Department of Oral Pathology and Microbiology, Manipal College of Dental Sciences, Manipal, Manipal Academy of Higher Education, Manipal 576104, Karnataka, India.
Tel: 91-9845701925
E-mail: monica.charlotte@manipal.edu
Received: October 31, 2021; Accepted: November 28, 2021; Published: December 07, 2021
Citation: Deepika Rathna, Monica Charlotte Solomon. Dental Stem Cells - Application In Dental Research And Therapeutic Implication. Int J Dentistry Oral Sci. 2021;8(12):5201-5206. doi: dx.doi.org/10.19070/2377-8075-210001043
Copyright: Dr. Monica Charlotte Solomon, MDS, PhD�2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Stem cells are "special cells� that possess pluripotent abilities � they are able to self-renew themselves and maintain the same
properties as their progenitor cells. Stem cells have the ability to differentiate into multiple cell lineages. Stem cells are fascinating
cells as both embryonic and somatic stem cells when introduced into a specific part of the body can differentiate into the
required cell type. Thereby, help in replacing damaged tissue and restoring tissue function.
There are a multitude of cells that are a part of the embryogenesis of the orofacial region that retain pluripotent ability. The
dental stem cells are an easily accessible source for stem cells. These cells, when isolated and cultured can be stimulated to
proliferate and form viable tissues through chemical or virally induced methods.
However, the potential of dental stem cells in treating dental disorders and diseases is less explored. The objective of this
review is to recapitulates the various cells of the orofacial region with pluripotent potential and their application in treating
oral and dental disorders. This paper also renders an insight into Biobanking and tissue engineering pertaining to dental tissues.
A greater insight and a better understanding of the cellular features and functional properties of dental stem cells will help in
developing treatment strategies for dental diseases.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Dental Stem Cells; Pluripotency; Regeneration; Biobanking; Tissue Engineering.
Introduction
Stem cells are undifferentiated and pluripotent cells that can produce
new stem cells (self-renewal) and in a particular condition or
in response to specific signals they can exit from self -renewal and
engage in differentiation into specialized cells with specific function
[1]. The stem cells are either embryonic stem cells or adult
stem cells or perinatal stem cells or induced pluripotent stem cells
(iPS). Several populations of stem cells have been isolated from a
tooth and from the orofacial region. With advances in technology
the pluripotent ability of the stem cells is harnessed to transform
them into specialized cells. This has paved the way for stem cells
to be used in tooth repair, restoration and in tissue regeneration.
Regenerative dentistry is an up-and-coming specialty which involves
the replacement of damaged tissue with regenerated human
stem cells. Here we review the various sources of dental stem
cells and their application in dental research and their therapeutic
application.
Stem Cells Derived From Oral And Maxillofacial Region
Adult stem cells are also known as somatic stem cells or postnatal
stem cells, and they are found in most of the tissues and organs.
The adult stem cells which reside in several mesenchymal tissues,
are jointly referred to as mesenchymal stem cells or multipotent
mesenchymal stromal cells (MSCs). These cells can differentiate
into limited cell types or cells of mesenchymal origin. MSCs are
seen in dental tissues, including dental pulp, periodontal ligament,
dental papilla, and dental follicle. These stem cells can be isolated and grown under defined tissue culture condition. Once the cells
are cultured, they are used in tissue engineering [2].
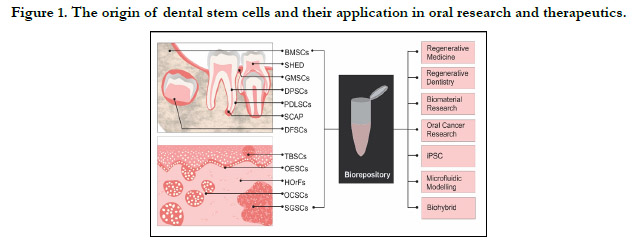
Most of the adult stem cells of the oral and maxillofacial region
are MSC�s. The different Mesenchymal stem cells occupy �stem
cell niches� in the oral and maxilla-facial region. These MSC�s include
dental pulp stem cells (DPSCs), stem cells from exfoliated
deciduous teeth (SHED), periodontal ligament stem cells (PDLSCs),
stem cells from the apical papilla (SCAP), Tooth germ progenitor
cells (TGPCs) Gingiva- derived Mesenchymal Stem cells
(GMSCs), dental follicle progenitor cells (DFPCs) and Bone Marrow
stem cells (BMSCs), salivary gland stem cells (SGSC�s) and
Oral Epithelial stem cells [3]. The origin of mesenchymal stem
cells of the oral and maxillofacial region was unknown for a long
time. It was considered that perivascular cells form mesenchymal
stem cells in most tissues. Recent studies have shown that glial
cells generate multipotent mesenchymal stem cells that produce
pulp cells and odontoblasts. This is consistent with the embryogenesis
of tooth formation wherein neural crest cells migrate to
form the dental ectomesenchyme [4].
Dental Pulp stem cells
The Dental pulp stem cells can be isolated from the permanent
third molar teeth. They exhibit high proliferation rate and a high
frequency of colony formation that produces densely calcified
nodules [5]. The dental pulp stem cells can form dentin- pulp
complexes [6].
Stem cells from exfoliated deciduous teeth
Stem cells are derived from the pulp of human exfoliated deciduous
teeth (SHED). These stem cells have a higher proliferation
rate, increased cell doubling time and a better osteo-inductive ability
compared to Dental Pulp stem cells. [7]. These cells can differentiate
into functional odontoblasts and are capable of generating
the formation of tubular dentin and angiogenic endothelial cells
[8].
Periodontal ligament stem cells
It is well established that the periodontal ligament contains a
population of progenitor cells. This population of stem cells are
able to differentiate into cementoblast-like cells, adipocytes and
connective tissue that is rich in collagen I in both in vitro and in
vivo settings [9].
Stem cells from the root apical papilla
Stem cells from the root apical papilla is an unique population
of cells that are located at the tip of the developing tooth roots.
Recently it has been determined that SCAPs possess the capacity
to differentiate into multiple cell types such as osteoblasts,
odontoblasts, neural cells, adipocytes, chondrocytes, and hepatocytes
[10].
Gingiva mesenchymal stem cells
Gingiva mesenchymal stem cells/progenitor cells are isolated
from the lamina propria of the gingiva. These cells are vested with
substantial regenerative and immunomodulatory properties [11].
Dental follicle stem cells
The dental follicle is known to contain progenitors for cementoblasts,
fibroblasts and osteoblasts. These stem cells can be isolated
from the third molar tooth. These cells have the ability to form
compact calcified nodules. These cells are typified by their rapid
rate of attachment in the culture and their expression of Nestin
and Notch -1 [12].
Tooth germ progenitor cell
TGPCS are found in the mesenchyme of wisdom teeth during
the late bell stage of odontogenesis [13]. TGPCs can differentiate
into dental tissues and non-dental mesenchymal tissues [14].
Oral epithelial stem cells
The basal layer of the oral epithelium contains a stem cell compartment
from which the oral mucosa is rejuvenated. These cells
expression of several stem cells markersThe basal layer serves as
a reservoir of cells with properties of self -renewal [15].
Periosteal derived stem cells
Alveolar bone stem cells (ASMSCs) reside within the osseous tissue.
Extracted ASMSCs displayed plastic adherence, colony formation,
and spindle-shaped fibroblast-like morphology. ABMSCs
had the potential to differentiate into adipocytes and chondrocytes
similar to those of other DSCs [16].
Salivary gland stem cells
In the human salivary gland, stem cells reside in the ductal region,
as indicated by the co-localization of stem cell markers [17]. The
intercalated ducts of the adult salivary glands has been recognized
to harbor a stem cell population capable of giving rise to both
acini and ducts [18].
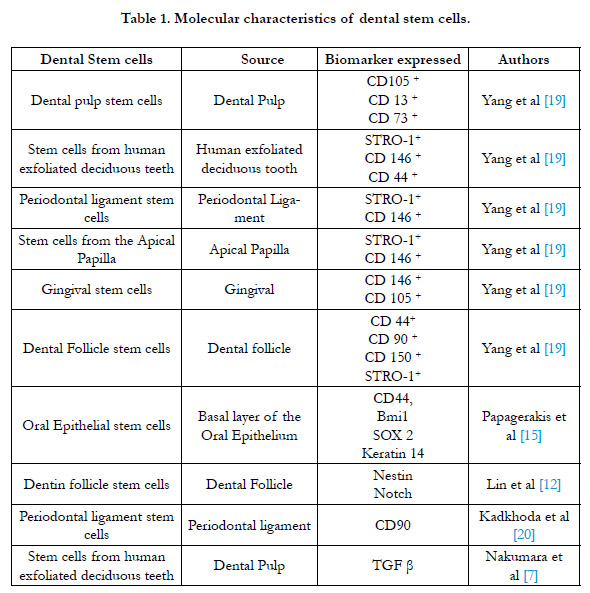
The molecular characteristics of the dental stem cells is given in
Table 1.
Induced Pluripotent Stem Cells
Takashi and Yamanakafound that somatic cells can be genetically
reprogrammed to achieve a pluripotent capacity by introducing
defined factors such as Oct3/4, SO2, Klf4 and c-Myc [21].
By introducing 3-4 transcription factors, the oral mesenchymal
cells such as dental pulp stem cells, stem cells from exfoliated deciduous
teeth, SCAP and stromal cells derived from the third molars
can be stimulated to generate iPS [22, 23]. Fibroblasts from
the gingiva is a good source for iPS. These cells are easily available
from patients and they have a high reprogramming capacity [24].
Adult human gingival fibroblasts can be reprogrammed without
using the transcription factor c-myc [25].
Induced pluripotent stem cells (iPS) in regenerative dentistry
There are studies that have been carried out where in iPS cells
have been used to produce cementum, alveolar bone and ameloblasts
[26, 27]. Ning et al stated that for formation of tooth to take place there is a need fora interaction of epithelium derived
from the ectoderm with the mesenchymal cells that are derived
from neural crest cells. Hence the cells that are induced to have a
pluripotent capacity should be able to differentiate into two lineages
with one being odontogenic in nature [28]. Through the
combination of iPS cells and enamel matrix derivatives, formation
of cementum, bone and periodontal ligaments has been
achieved [27]. This expertise can reform the field of medicine
because of IPS cells have the capacity to develop into all tissues/
organs. These IPS cells can play a vital role in the developing field
of ��tailored medicine�� which uses a patient�s own cells to provide
biologically compatible tissues [29].
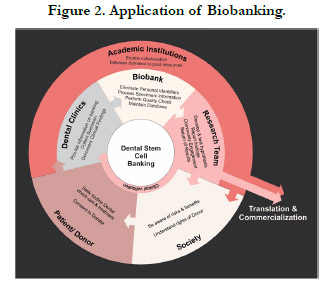
Dental stem cell banking
The advantages of dental stem cells include guaranteed matching
of donors, cells are saved before they are damaged, acquiring
them is a simple and a painless procedure, they are less expensive
and there are less ethical issues related to their clinical application.
The disadvantages of dental stem cells are that only a few cells are
available for isolation and that there is no proper research directed
towards understanding their long-term efficiency [30]. With the
realization that dental pulp stem cells are a major source of stem
cells and that they can be utilized for tissue engineering and in the
treatment of dental and medical diseases �tooth stem cell banks�
have emerged [31, 32].
The fundamental steps in dental biobanking involves sample collection
(whole tooth under sterile conditions), stem cell isolation,
stem cell storage and stem cell usage [33]. The various sources of
dental stems cells and the avenues where they can be utilized is
given in Fig 1. The benefits of biobanking of stem cells is given
in Fig 2.
Application Of Dental Stem Cells
Dental Material research
Evaluation of biological effects of dental materials is empirical
for its ultimate clinical usage. Several types of cells have been used
for this purpose ranging from primary cultured fibroblasts to immortalized
cell lines [34].
Regenerative Dentistry
Regenerative dentistry refers to designing biological alternatives
for root canal treatments, regeneration of dental hard tissues, revascularization
and regrowth of lost periodontal tissues [35].
Pulpstem cells
Owning to their highly proliferative and clonogenic nature, DPSCs
can differentiate into hard tissue forming cells. Damaged odontoblasts
can be replaced with newly regenerated odontoblastlike
cells that are derived from the DPSCs [36]. DPSCs have also
been implicated in regeneration of tooth pulp following endodontic
infection [37].
In another study a 3-dimensional cell construct comprising of
DPSC�s facilitated the regeneration of the dental pulp. When a
3-dimensional (3D) cell constructs composed of DPSC�s was
filled in a human root canal, pulp-like tissues with rich blood vessels
were formed within the human root canal 6 weeks after the
implantation [38].
Periodontal Ligament
Periodontal ligament stem cells that are isolated from miniature
pig have similar properties as that human periodontal ligament
stem cells. This implies that PDLSCs could assist in periodontal
tissue regeneration in vivo. This kind of cellular therapies can be
used to treat periodontal disease and to minimize tooth loss [39].
However, Li et al observed that PDLSCs derived from resorbed
primary teeth (humans) expressed RUNX2, which upregulated
RANKL and downregulated OPG. These imbalances between
RANKL and OPG finally led to osteoclast differentiation and
root absorption [40].
Salivary Gland
Salivary gland stem cells obtained from human submandibular
salivary gland were cultured to form salispheres. When these cultured
salispheres were transplanted into submandibular gland of
irradiated (to ablate the salivary glands) mice. The transplanted
stem cell salispheres were able to differentiate and produce saliva.
This shows that human SGs contain stem/progenitor cells capable
of self-renewal and differentiation to functional cells that can
produce saliva. This can be very beneficial in treating patients with
hyposalivation [41].
Dental stem cells and tissue Engineering
Tissue engineering comprises of three key elements: A scaffolding
/extracellular matrix, stem cells/Progenitor cells and signaling
molecules/ growth factor.
Scaffolds provide a structural integrity for cells until the newly
formed tissue becomes auto sustainable. Synthetic scaffolds such
a poly-(1-lactic acid) PLLA, Poly- (glycolic acid) PGA allow engineering
of complex dental structures with characteristics that
resemble the crowns of natural teeth [42].
When SHED cells were seeded in scaffolds surrounded with
dentin, they differentiated into odontoblasts. These odontoblasts
expressed DMP-1, sialophosphoprotein and matrix extracellular
phosphoglycoprotein [43].
Bone morphogenic proteins, Dentin sialoproteins, Dentin phosphoproteins
and Vascular endothelial factor that are present in the
scaffold assist in differentiation of dental stem cells. It has been
reported that SHED cells were able to differentiate into endothelial
cells that make functional blood vessels that carry blood [8].
Whole tooth engineering
This technique refers to regeneration of an entire tooth complex
of Enamel, dentin and cementum encasing the dental pulp
with stroma blood vessels. Whole tooth engineering technology
involves re-association between embryonic dental epithelial and
mesenchymal cells. Many methods have been proposed to carry
out this process. The hanging-drop technique provides a 3D architecture
to enable cell-cell adhesion [44].
Regenerative Medicine
The stem cells of the orofacial region do not express HOX genes,
and hence their cross -transplantation can result in the formation
of mature bone directly without the intermediate stage of cartilaginous
callus formation [45].
DPSCs were found to express a number of angiogenic factors
such as platelet derived growth factor (PDGF), vascular endothelial
growth factor (VEGF), and fibroblast growth factor (FGF)
[46]. Therefore, DPSCs are attractive stem cell source for the
treatment for chronic wounds, myocardial infarction, and stroke.
3D cell culture
Jimenez at al carried out an in vitro study wherein dental pulp
mesenchymal stem cells were cultured on 3D scaffolds of Polylactic
and polyglycolic scaffolds incorporated with hydroxyapatite
(HA) under osteogenic conditions. They found that that the HA
in the scaffold accelerated cell interaction and osteogenic differentiation
of the hDPSC�s. The cultured hDPSC�s showed a high
expression of osteogenic markers Runt-related transcription factor
2 (RUNX2), Oteopontin (OPN), Alkaline Phosphatas (ALP)
and Collagen I (COL_I). Hence this technology can be effectively
utilized in bone tissue engineering and regenerative medicine [47].
A fibrin -based bio-ink has been designed for human dental pulp
stem cells (hDPSC). The morphology of the hDPSC was wellmaintained
even after 25 days of cell culture. The expression of
DMP1 and DSPP (as evaluated through RT-PCR) by the hDPSC
increased with the concentration of fibrin in the bio-ink. This
indicates that Bio printing of hDPSC�s can induce localized odontogenic
differentiation [48].
Cell Sheet
Cell sheets technique is a process by which the cultured cells are
harvested as intact sheets with an extracellular matrix. In a clinical
study by Iwata et al, a three -layered periodontal ligament MSC�s
cell sheet was transplanted onto the clean root surface of teeth
with periodontal disease in ten patients. A six month follow -up of
these patients showed that there was reduced periodontal pocket
probing depth, there was gain in the clinical attachment and an
increase in the radiographic bone height in all the 10 patients [49].
Micofluidic modelling
The behaviour of stem cells in the orofacial region depends on
the cellular, molecular and physiological conditions of their microenvironment,
the stem cell niches. Micorfluidic technique provides
an environment for stem cells in culture media that mimics
the microenvironment of stem cells niches of the orofacial region.
This method provides a better microenvironment for crosstalk
among stem cells. The dental stem cell cultured this way will
be morphologically and functionally suitable for regeneration of
damaged or pathological tissues and organs of the orofacial region
[50].
Conclusion
To summarize, with a wide range of dental stem cell types that have been identified and with advances in technology, numerous
avenues are open for dental stem cells in dental research and
therapy. Although most of the biological potential of dental stem
cells has been deciphered through in vitro studies, the clinical trials
that are being carried out are also showing positive results. The
paramount target in dentistry is to be able replace lost teeth using
biological tissues; in essence a cell -based implant rather than a
metal one. The task that lies ahead is to be able to generate a biologically
functional root. Therefore, with advances in technology
and empowered with skills in cell culture and molecular biology
more research in the field of dental stem cells can be carried out.
These research outcomes can greatly contribute towards treating
dental and oral diseases with precision.
References
-
[1]. Weissman IL. Stem cells: units of development, units of regeneration,
and units in evolution. Cell. 2000 Jan 7;100(1):157-68. PubMed PMID:
10647940.
[2]. Estrela C, Alencar AH, Kitten GT, Vencio EF, Gava E. Mesenchymal stem cells in the dental tissues: perspectives for tissue regeneration. Braz Dent J. 2011;22(2):91-8. PubMed PMID: 21537580.
[3]. Egusa H, Sonoyama W, Nishimura M, Atsuta I, Akiyama K. Stem cells in dentistry--part I: stem cell sources. J Prosthodont Res. 2012 Jul;56(3):151- 65. PubMed PMID: 22796367.
[4]. Rodr�guez-Lozano FJ, Bueno C, Insausti CL, Meseguer L, Ram�rez MC, Blanquer M, Mar�n N, Mart�nez S, Moraleda JM. Mesenchymal stem cells derived from dental tissues. IntEndod J. 20
11 Sep;44(9):800-6. PubMed PMID: 21477154. [5]. Gronthos S, Brahim J, Li W, Fisher LW, Cherman N, Boyde A, DenBesten P, Robey PG, Shi S. Stem cell properties of human dental pulp stem cells. J Dent Res. 2002 Aug;81(8):531-5. PubMed PMID: 12147742.
[6]. Koyama N, Okubo Y, Nakao K, Bessho K. Evaluation of pluripotency in human dental pulp cells. J Oral Maxillofac Surg. 2009 Mar;67(3):501-6. PubMed PMID: 19231772.
[7]. Nakamura S, Yamada Y, Katagiri W, Sugito T, Ito K, Ueda M. Stem cell proliferation pathways comparison between human exfoliated deciduous teeth and dental pulp stem cells by gene expression profile from promising dental pulp. J Endod. 2009 Nov;35(11):1536-42. PubMed PMID: 19840643.
[8]. Sakai VT, Zhang Z, Dong Z, Neiva KG, Machado MA, Shi S, Santos CF, N�r JE. SHED differentiate into functional odontoblasts and endothelium. J Dent Res. 2010 Aug;89(8):791-6. PubMed PMID: 20395410.
[9]. Seo BM, Miura M, Gronthos S, Bartold PM, Batouli S, Brahim J, Young M, Robey PG, Wang CY, Shi S. Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet. 2004 Jul 10-16;364(9429):149- 55. PubMed PMID: 15246727.
[10]. Kang J, Fan W, Deng Q, He H, Huang F. Stem Cells from the Apical Papilla: A Promising Source for Stem Cell-Based Therapy. Biomed Res Int. 2019 Jan 29;2019:6104738. PubMed PMID: 30834270.
[11]. Fawzy El-Sayed KM, D�rfer CE. Gingival Mesenchymal Stem/Progenitor Cells: A Unique Tissue Engineering Gem. Stem Cells Int. 2016;2016:7154327. PubMed PMID: 27313628.
[12]. Lin NH, Gronthos S, Bartold PM. Stem cells and periodontal regeneration. Aust Dent J. 2008 Jun;53(2):108-21. PubMed PMID: 18494965.
[13]. Nanci A. Ten Cate�s Oral Histology-E-Book: Development, Structure, and Function. 9th ed. Elsevier Health Sciences; 2017.
[14]. Caracappa JD, Gallicchio VS.The future in dental medicine: Dental stem cells are a promising source for tooth and tissue engineering. J Stem Cell Res Ther. 2019;5(2):30-36.
[15]. Papagerakis S, Pannone G, Zheng L, About I, Taqi N, Nguyen NP, Matossian M, McAlpin B, Santoro A, McHugh J, Prince ME, Papagerakis P.
Oral epithelial stem cells - implications in normal development and cancer metastasis. Exp Cell Res. 2014 Jul 15;325(2):111-29. PubMedPMID: 24803391.
[16]. Lim KT, Hexiu J, Kim J, Seonwoo H, Choung PH, Chung JH. Synergistic effects of orbital shear stress on in vitro growth and osteogenic differentiation of human alveolar bone-derived mesenchymal stem cells. Biomed Res Int. 2014;2014:316803. PubMed PMID: 24575406.
[17]. Sato A, Okumura K, Matsumoto S, Hattori K, Hattori S, Shinohara M, Endo F. Isolation, tissue localization, and cellular characterization of progenitors derived from adult human salivary glands. Cloning Stem Cells. 2007 Summer;9(2):191-205. PubMed PMID: 17579552.
[18]. Ihrler S, Blasenbreu-Vogt S, Sendelhofert A, R�ssle M, Harrison JD, L�hrs U. Regeneration in chronic sialadenitis: an analysis of proliferation and apoptosis based on double immunohistochemical labelling. Virchows Arch. 2004 Apr;444(4):356-61. PubMed PMID: 14762713.
[19]. Yang B, Qiu Y, Zhou N, Ouyang H, Ding J, Cheng B, Sun J. Application of Stem Cells in Oral Disease Therapy: Progresses and Perspectives. Front Physiol. 2017 Apr 3;8:197. PubMed PMID: 28421002.
[20]. Kadkhoda Z, Rafiei SC, Azizi B, Khoshzaban A. Assessment of Surface Markers Derived from Human Periodontal Ligament Stem Cells: An In Vitro Study. J Dent (Tehran). 2016 Sep;13(5):325-332. PubMed PMID: 28127326.
[21]. Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006 Aug 25;126(4):663-76. PubMed PMID: 16904174.
[22]. Yan X, Qin H, Qu C, Tuan RS, Shi S, Huang GT. iPS cells reprogrammed from human mesenchymal-like stem/progenitor cells of dental tissue origin. Stem Cells Dev. 2010 Apr;19(4):469-80. PubMed PMID: 19795982.
[23]. Oda Y, Yoshimura Y, Ohnishi H, Tadokoro M, Katsube Y, Sasao M, Kubo Y, Hattori K, Saito S, Horimoto K, Yuba S, Ohgushi H. Induction of pluripotent stem cells from human third molar mesenchymal stromal cells. J Biol Chem. 2010 Sep 17;285(38):29270-8. PubMed PMID: 20595386.
[24]. Egusa H, Okita K, Kayashima H, Yu G, Fukuyasu S, Saeki M, et al. Gingival fibroblasts as a promising source of induced pluripotent stem cells. 2010 Sep 14;5(9):e12743. PubMed PMID: 20856871.
[25]. Wada N, Wang B, Lin NH, Laslett AL, Gronthos S, Bartold PM. Induced pluripotent stem cell lines derived from human gingival fibroblasts and periodontal ligament fibroblasts. J Periodontal Res. 2011 Aug;46(4):438-47. PubMed PMID: 21443752.
[26]. Yoshida K, Sato J, Takai R, Uehara O, Kurashige Y, Nishimura M, et al. Differentiation of mouse iPS cells into ameloblast-like cells in cultures using medium conditioned by epithelial cell rests of Malassez and gelatincoated dishes. Med MolMorphol. 2015 Sep;48(3):138-45. PubMed PMID: 25319805.
[27]. Duan X, Tu Q, Zhang J, Ye J, Sommer C, Mostoslavsky G, Kaplan D, Yang P, Chen J. Application of induced pluripotent stem (iPS) cells in periodontal tissue regeneration. J Cell Physiol. 2011 Jan;226(1):150-7. PubMed PMID: 20658533.
[28]. Ning F, Guo Y, Tang J, Zhou J, Zhang H, Lu W, Gao Y, Wang L, Pei D, Duan Y, Jin Y. Differentiation of mouse embryonic stem cells into dental epithelial-like cells induced by ameloblasts serum-free conditioned medium. BiochemBiophys Res Commun. 2010 Apr 2;394(2):342-7. PubMed PMID: 20206604.
[29]. Azqueta A, Collins AR. The essential comet assay: a comprehensive guide to measuring DNA damage and repair. Arch Toxicol. 2013 Jun;87(6):949-68. PubMed PMID: 23685795.
[30]. Roma M, Hegde S, Thomas MS. Biobanking in dentistry. Journal of Pharmaceutical Sciences and Research. 2016 Aug 1;8(8):767.
[31]. Rai S, Kaur M, Kaur S, Arora SP. Redefining the potential applications of dental stem cells: An asset for future. Indian J Hum Genet. 2012 Sep;18(3):276-84. PubMed PMID: 23716933.
[32]. Kabir R, Gupta M, Aggarwal A, Sharma D, Sarin A, Kola MZ. Imperative role of dental pulp stem cells in regenerative therapies: a systematic review. Niger J Surg. 2014 Jan;20(1):1-8. PubMed PMID: 24665194.
[33]. Berz D, McCormack EM, Winer ES, Colvin GA, Quesenberry PJ. Cryopreservation of hematopoietic stem cells. Am J Hematol. 2007 Jun;82(6):463-72. PubMed PMID: 17266054.
[34]. Nahid M, Bottenberg P. L'int�r�t des cultures cellulairesdans la recherche de mat�riauxdentairesbiocompatibles [Importance of cell cultures in biocompatible dental materials research]. Rev Belge Med Dent (1984). 2003;58(3):189-96. French. PubMed PMID: 14686145.
[35]. Torvi SJ, Munniswamy K. Regenerative dentistry: Current and future perspectives to rejuvenate and reclaim dental tissues. Journal of the International Clinical Dental Research Organization. 2014 Jul 1;6(2):112.
[36]. Huang GT. Pulp and dentin tissue engineering and regeneration: current progress. Regen Med. 2009 Sep;4(5):697-707. PubMed PMID: 19761395.
[37]. Yu J, Deng Z, Shi J, Zhai H, Nie X, Zhuang H, Li Y, Jin Y. Differentiation of dental pulp stem cells into regular-shaped dentin-pulp complex induced by tooth germ cell conditioned medium. Tissue Eng. 2006 Nov;12(11):3097- 105. PubMed PMID: 17518625.
[38]. Itoh Y, Sasaki JI, Hashimoto M, Katata C, Hayashi M, Imazato S. Pulp Regeneration by 3-dimensional Dental Pulp Stem Cell Constructs. J Dent Res. 2018 Sep;97(10):1137-1143. PubMed PMID: 29702010.
[39]. Yu J, Deng Z, Shi J, Zhai H, Nie X, Zhuang H, Li Y, Jin Y. Differentiation of dental pulp stem cells into regular-shaped dentin-pulp complex induced by tooth germ cell conditioned medium. Tissue Eng. 2006 Nov;12(11):3097- 105. PubMed PMID: 17518625.
[40]. Li B, Zhang Y, Wang Q, Dong Z, Shang L, Wu L, Wang X, Jin Y. Periodontal ligament stem cells modulate root resorption of human primary teeth via Runx2 regulating RANKL/OPG system. Stem Cells Dev. 2014 Oct 15;23(20):2524-34. PubMed PMID: 24827498.
[41]. Pringle S, Maimets M, van der Zwaag M, Stokman MA, van Gosliga D, Zwart E, Witjes MJ, de Haan G, van Os R, Coppes RP. Human Salivary Gland Stem Cells Functionally Restore Radiation Damaged Salivary Glands. Stem Cells. 2016 Mar;34(3):640-52. PubMed PMID: 26887347.
[42]. Young CS, Terada S, Vacanti JP, Honda M, Bartlett JD, Yelick PC. Tissue engineering of complex tooth structures on biodegradable polymer scaffolds. J Dent Res. 2002 Oct;81(10):695-700. PubMed PMID: 12351668.
[43]. Casagrande L, Demarco FF, Zhang Z, Araujo FB, Shi S, N�r JE. Dentin- derived BMP-2 and odontoblast differentiation. J Dent Res. 2010 Jun;89(6):603-8. PubMed PMID: 20351355.
[44]. Nakao K, Morita R, Saji Y, Ishida K, Tomita Y, Ogawa M, et al. The development of a bioengineered organ germ method. Nat Methods. 2007 Mar;4(3):227-30. PubMed PMID: 17322892.
[45]. Leucht P, Kim JB, Amasha R, James AW, Girod S, Helms JA. Embryonic origin and Hox status determine progenitor cell fate during adult bone regeneration. Development. 2008 Sep;135(17):2845-54. PubMed PMID: 18653558.
[46]. Tran-Hung L, Laurent P, Camps J, About I. Quantification of angiogenic growth factors released by human dental cells after injury. Arch Oral Biol. 2008 Jan;53(1):9-13. PubMed PMID: 17764655.
[47]. Jim�nez NT, Carlos Mun�var J, Gonz�lez JM, Infante C, Lara SJP. In vitro response of dental pulp stem cells in 3D scaffolds: A regenerative bone material. Heliyon. 2018 Sep 24;4(9):e00775. PubMed PMID: 30263971.
[48]. Han J, Kim DS, Jang H, Kim HR, Kang HW. Bioprinting of three-dimensional dentin-pulp complex with local differentiation of human dental pulp stem cells. J Tissue Eng. 2019 May 19;10:2041731419845849. PubMed PMID: 31205671.
[49]. Iwata T, Yamato M, Washio K, Yoshida T, Tsumanuma Y, Yamada A, Onizuka S, Izumi Y, Ando T, Okano T, Ishikawa I. Periodontal regeneration with autologous periodontal ligament-derived cell sheets - A safety and efficacy study in ten patients. Regen Ther. 2018 Aug 24;9:38-44. PubMed PMID: 30525074.
[50]. Pagella P, Neto E, Lamghari M, Mitsiadis TA. Investigation of orofacial stem cell niches and their innervation through microfluidic devices. Eur Cell Mater. 2015 Mar 20;29:213-23. PubMed PMID: 25794530.