Comparison of Lactate Dehydrogenase (LDH), Aspartate Aminotransferase (AST) and Alkaline Phosphatase (ALP) in Saliva of Normal, Gingivitis and Periodontitis Patients
Rafaela Cristiane Canavezi1, Viviane Maria Gonçalves de Figueiredo2, Alecsandro Moura de Silva3, Laura Souto Soares Lepesqueur4, José Renato Cavalcanti Queiroz5, Marcos Massi6, Renata Falchete do Prado7*, Lafayette Nogueira Junior8
1 Department of Dental Materials and Prosthodontics, Institute of Science and Technology of São José dos Campos, São Paulo State University (UNESP),
Sao Jose dos Campos, 12245000 Brazil.
2 Department of Dental Materials and Prosthodontics, Institute of Science and Technology of São José dos Campos, São Paulo State University (UNESP),
Sao Jose dos Campos12245000, Brazil.
3 Department of Dentistry, UNITAU - University of Taubaté, Taubaté, SP, Brazil.
4 Department of Dental Materials and Prosthodontics, Institute of Science and Technology of São José dos Campos, São Paulo State University (UNESP),
Sao Jose dos Campos 12245000, Brazil.
5 Department of Biotechnology, UnP – Laureate University, Natal, 59010020 Brazil.
6 Mackenzie Presbyterian University, School of Engineering-PPGEMN, São Paulo 01302907 Brazil.
7 Department of Dental Materials and Prosthodontics, Institute of Science and Technology of São José dos Campos, São Paulo State University (UNESP),
Sao Jose dos Campos, 12245000 Brazil.
8 Department of Dental Materials and Prosthodontics, Institute of Science and Technology of São José dos Campos, São Paulo State University (UNESP),
Sao Jose dos Campos, 12245000 Brazil.
*Corresponding Author
Renata Falchete do Prado,
Department of Dental Materials and Prosthodontics, Institute of Science and Technology of São José dos Campos, São Paulo State University (UNESP), Sao Jose dos Campos,
12245000 Brazil.
Tel: +551239479036
Fax: +551239479010
E-mail: renatafalchete@hotmail.com
Received: Ocotber 20, 2021; Accepted: November 13, 2021; Published: November 29, 2021
Citation: Rafaela Cristiane Canavezi, Viviane Maria Gonçalves de Figueiredo, Alecsandro Moura de Silva, Laura Souto Soares Lepesqueur, José Renato Cavalcanti Queiroz, Marcos Massi, Renata Falchete do Prado, Lafayette Nogueira Junior. Diamond-Like-Carbon Coating Over Prosthetic Screws: Analysis Of The Torque Maintenance After Retorque. Int J Dentistry Oral Sci. 2021;8(11):5157-5163. doi: dx.doi.org/10.19070/2377-8075-210001036
Copyright: Renata Falchete do Pradol©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: The retorqueing of fixing screws has become a routine in clinical practice, aiming to reduce the risk of screw
loosening; however, there are not in vitro studies that evaluate the effect of this clinical practice in nanofilm-coated screws.
The objective of this study was to verify the torque maintenance of prosthetic pillar screws coated with diamond-doped
diamond-like nanofilm (DD-DLC), submitted to retorque, after mechanical fatigue, in external (EH) and internal hexagonal
connections (IH).
Materials and Methods: Different implants and treatments of the prosthetic screws resulted in eight experimental groups
(n=5): untreated and not submitted to fatigue (EH-CON) (IH-CON); untreated and fatigued control (EH-F) (IH-F); with
DLC nanofilm and fatigued (EH-DLCF) (IH-DLCF) and with DD-DLC nanofilm and fatigued (EH-DD-DLCF) (IH-DDDCLF).
The coatings were plasma-deposited through the Plasma Enhanced Chemical Vapor Deposition method. The samples
were exposed to one million fatigue cycles; samples were submitted to reverse torque; samples were retorqued; then samples
were re-submitted to another one million mechanical cycles. After fatigue, the reverse torque of the screws was performed
to determine the torque maintenance. The screws were qualitatively analyzed through a scanning electron microscope. The
statistical analysis used ANOVA.
Results: There was no interaction between the studied factors. The treatment of screws and connection type did not present
significant differences. The coatings did not interfere in the adaptation of the screw to the implant.
Conclusion: The prosthetic screws with DLC and DD-DLC nanofilms, after retorque, did not present increased torque
maintenance.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Dental Implant; Screw Loosening; Reverse Torque; Retorque; Diamond-Like Carbon Coating.
Introduction
The complications of prostheses over implants present biological
and mechanical levels. Among the mechanical complications, the
loosening and fracture of the prosthetic screw, abutment fracture,
retention loss, crown cementation loss, and implant fracture may
be listed [1]. The screw loosening is the most common mechanical
cause associated with the failure of prostheses over implants
[2]. The adaptation between the abutment and the implant, the
parafunction, and/or oblique loads interfere in the screwed junction
resistance [3], and the corrosion also may interfere in this
issue [4].
In an attempt to minimize or control loosening, new implant, and
pillars designs, and screws surface treatments have been proposed
[5]. The prosthetic screw surface and material composition promote
changes in the coefficient of friction, to which the preload
value is inversely proportional [6].
The coating of the screw threads, as proposed in some studies, is
based on the principle of change in the coefficient of friction of
this surface (dry lubrication) [7], which improves its tribological
properties, generating more longitudinal stability in the pillar-implant
system with less screw loosening incidence [8]. Such coating
has been especially applied as carbon-like diamond (DLC) films,
grown from plasma [9].
An investigation using DCL-coated screws in hexagonal connections,
after fatigue simulation, demonstrated that samples with the
DLC coating were more resistant to an applied force than those
without the coating [7] and presented better torque maintenance
values than the ones with other coatings [10]. The DLC coating
of titanium screws in internal and external hexagonal connections,
after mechanical fatigue, had not shown damage to screws
threads [6].
Another class of carbon-based nanofilms is based on nanocrystalline
diamond [11]. A mixture of nanodiamond nanoparticles
with different forms of sp2-bonded carbon has been used for
improved tribological properties of industrial oils and greases.
These nanodiamond nanoparticles may be used as additives to
lubricants. They are one of the most promising nanocolloidal additives
[12].
Previous studies have shown that the retorquing, 10 min. after
first torque, caused an insignificant maladjustment effect of titanium
screws, suggesting that this procedure could be used routinely
[13]. The retorque evaluation of titanium and gold screws
in six months to one year of fatigue process proved that the titanium
screws stability was greater than the gold screws and after
one year, titanium screws were less stable due to torque loss
when maladjustments were found [14]. After mechanical cycling,
retorque did not present a significant difference between adapted
and non-adapted prostheses; hence, the retorque of gold and titanium
screws is indicated for multiple prostheses, since there was a
reduction in the loosening of such screws [15].
The purpose of this study was to evaluate the torque maintenance
of prosthetic pillar screws coated with diamond-dopped DLC nanofilm
after mechanical fatigue, submitted to retorque in external
(EH) and internal hexagonal connections (IH).
The considered null hypotheses were the following: H01 - The
torque maintenance of nanofilm-treated screws will not present
superior values than the ones of uncoated/non-fatigued screws;
H02 - internal hexagonal connections will not present torque
maintenance values higher than the ones found on external hexagonal
connections, and H03 – diamond-dopped DLC nanofilm
will not present difference in torque maintenance values when
compared to DLC nanofilm.
Materials And Methods
Material
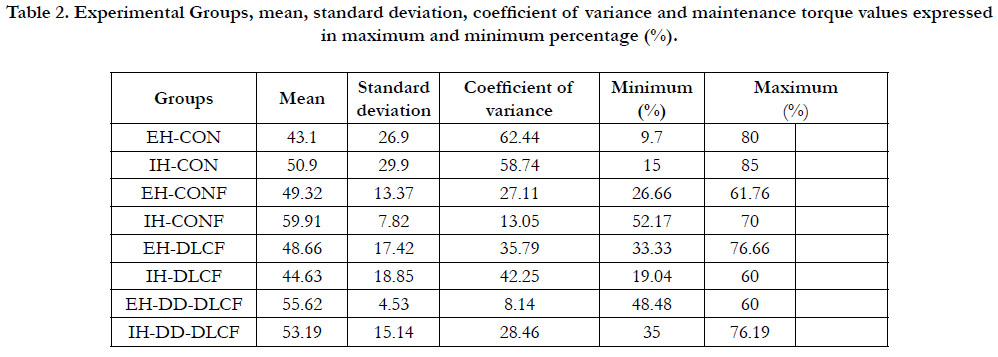
The materials used in this research are listed in Table 1.
Experimental and Sample Groups
This study was performed with the following experimental groups:
EH-CON: Prosthetic pillar screws, EH connection, non-fatigued, untreated.
EH-CONF: Prosthetic pillar screws, EH connection, fatigued,
untreated.
EH-DLCF: Prosthetic pillar screws, EH connection, fatigued,
pre-treated with DLC nanofilm.
EH-DD-DLCF: Prosthetic pillar screws, EH connection, fatigued,
pre-treated with diamond-doped DLC nanofilm (DDDLC).
IH-CON: Prosthetic pillar screws, IH connection, non-fatigued,
untreated.
IH-CONF: Prosthetic pillar screws, IH connection, fatigued, untreated.
IH-DLCF: Prosthetic pillar screws, IH connection, fatigued, pretreated
with DLC nanofilm.
IH-DD-DLCF: Prosthetic pillar screws, IH connection, fatigued,
pre-treated with DD-DLC nanofilm.
For the IH-CON and EH-CON groups, new, non-fatigued screws
were used. Each experimental group had five specimens. The
sampling calculation was performed based on the standard deviation
of a similar study [6], using a data analysis statistics software
(Minitab version 1.6, for Windows, Pennsylvania, USA), with 80%
of sampling power.
Preparation of specimens
The implants were installed in polyurethane resin blocks (22 x
15 mm - Polyurethane F16 with mineral load (RZ 30150-Axson,
France - elastic modulus of 3.6 GPa.). Implants were milled at an
inclination of 90º and installed with the assistance of a manual
ratchet, while blocks were fixed. The applied torque for the installation
of implants was 45 N. 3 mm of the implant threads were
left exposed (ISO 14801), whereas the pillar had a standard height
of 8 mm.
The screws were coated through the Plasma-Enhanced Chemical
Vapor Deposition technique (PECVD). For the DLC and diamond-
doped DCL nanofilms, the gas was the hexane (C6H14)
and the hexane with diamond nanoparticles (2 g/L), respectively.
In this deposition process, the screws were positioned at a sample
holder, which assured proper positioning. The deposition was
performed as previously described [6].
After deposition, screws were torqued with a digital torque meter
(TQ-680, Instrutherm Measuring Instruments São Paulo Brazil).
The torque of 20 Ncm was performed in IH and the torque of
30 Ncm was performed in EH, according to manufacturer recommendation.
Ten minutes after the application of the initial torque,
the procedure was repeated.
Experimental crown
Nickel-chrome alloy total crowns (Litecast B Will-Ceram/USA)
were prepared in a conical-trunk shape, with a diameter and occlusal
height of 8 mm, and presented a hole to access the screw.
The crowns were cemented with zinc oxide cement (Temp Bond
NE, KaVo-Kerr), with 500 g of pressure, for 10 min.
Fatigue testing
Mechanical fatigue was performed through a fatigue simulator
(ER-11000-Erios Plus, Equipment Technical and Scientific São
Paulo, Brazil). Cycles were applied with an average force of 133
N, at eccentric contact (3 mm), frequency of 4 Hz, 1 x106 cycles.
These cycles represent approximately 12 months of function and
were replicated at a temperature of 37°C ± 2°C.
After mechanical cycling, the abutment screw was subjected to
reverse torque (data reported elsewhere [6]).
Retorque and Fatigue testing
Screws were torqued again with the same digital torque meter using
20 Ncm (IH) and 30 Ncm (EH).
Mechanical fatigue was repeated. At the end of fatigue, the screws
were submitted to reverse torque to check the maintenance of
the torque.
Torque maintenance
The remaining torque quantity in each tightened union was calculated,
and these measurements were performed with the digital
torque meter. The reverse torque values were converted into
percentages related to the applied torque (retorque), through the
following equation (1):
Reverse torque (%) = (Reverse torque pos - loading / Applied
torque) x 100
Qualitative analysis
Screws from each group were selected for analysis through a
scanning electron microscope (SEM JEOL, model JSM-5310,
Munich, Germany), for the investigation of eventual alterations
in the structure of the screw (threads). One specimen of each
experimental group was sectioned with a precision cutter (IsoMet
1000, Buehler Ltd. IL, USA) on its longitudinal axis, allowing
observation of the marginal adaptation of the prosthetic screw.
The marginal adaptation was investigated by observing the gap
between the screw and the implant using photomicrographs.
Statistical Analysis
The reverse torque averages (%) of each experimental group were
submitted to statistical analysis using two-way ANOVA (factors:
connections and screws coatings), using Minitab software (version
16.1 for Windows, Pennsylvania, USA) (5% of significance
level).
Data normality was accessed through the Kolmogorov-Smirnov
Test (KS) for each experimental group. This confirms the possible
utilization of parametric statistical analysis, as well as per data
dispersion graphs.
Results
Torque maintenance
All groups presented Gaussian distribution according to the
normality test. There was no significant interaction between the
analyzed factors (screws coatings, p=0.638; implant connections,
p=0.615), nor amongst associated factors (p=0.765). And such findings were repeated between only fatigued groups (screws
coatings, p=0.356; implant connections, p=0.788; associated factors,
p= 0.444). The Group IH-CONF presented the highest
torque maintenance value, followed by EH-DD-DLCF and IHDLCF
(Table 2).
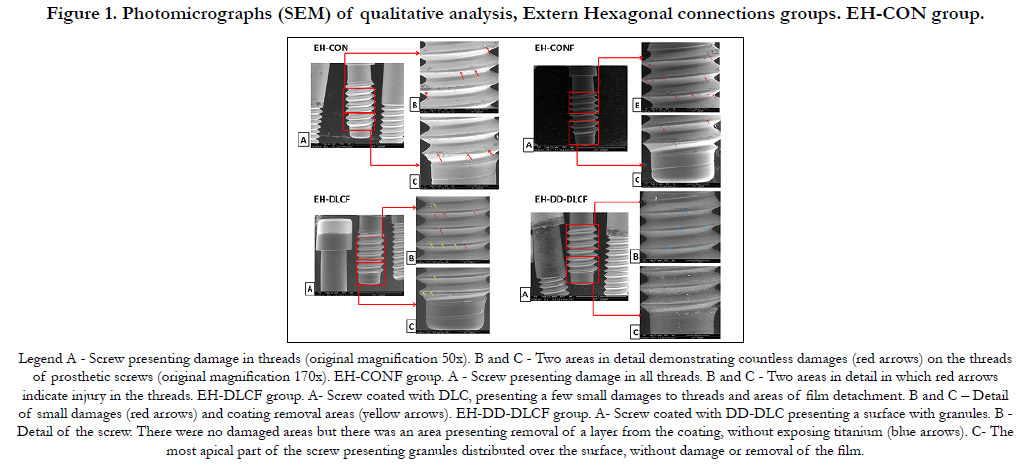
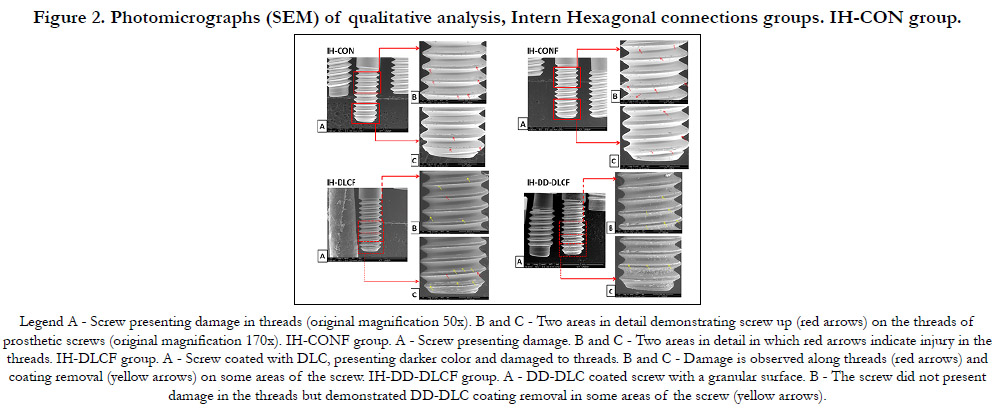
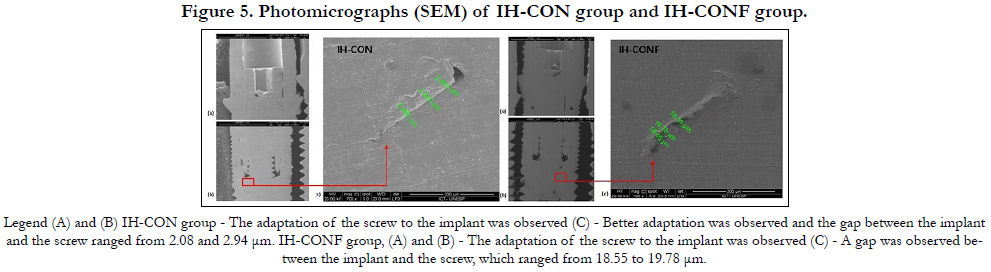
Qualitative analysis: Surface qualitative analysis
In the qualitative analysis of screws, in the EH/IH-DLCF group
(Fig. 1 and 2), there were lower screw thread damages when compared
to the groups without nanofilm.
The EH/IH-CON and EH/IH-CONF groups presented numerous
damages to screws threads (Fig. 1 and 2). The damages
found on EH/IH CON presented larger dimensions, whereas the
damages found in EH/IH-CONF presented higher quantity, but
smaller dimensions.
In some areas, the DLC nanofilm was removed in the EH-DLCF
group (Fig. 1) and IH-DLCF group (Fig. 2). The EH/IH-DDDLCF
groups presented scattered granulation along the screws’
surfaces and no alterations were observed (damage to threads) in
the screw’s structures (Fig. 1 and 2).
In the EH-DD-DLCF group (Fig. 1), the cervical portion of the
screw presented regions of possible coating layer removal, although
no titanium exposure occurred.
In the IH-DLCF group (Fig. 2), there was more incidence of
nanofilm delamination (exposing the titanium) when compared
to the EH-DLCF group (Fig. 1). In the IH-DD-DLCF group,
screws presented areas in which the DD-DLC film was removed
(Fig. 2). For both connections, the cervical portion of screws presented
a smaller quantity of scattered granulation than the apical
portion (Fig. 1 and 2).
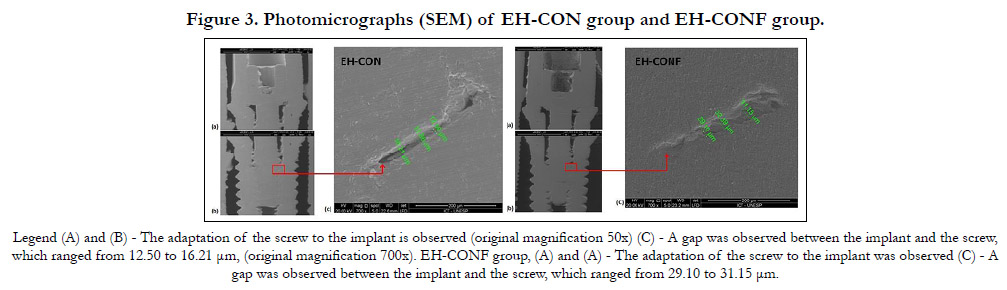
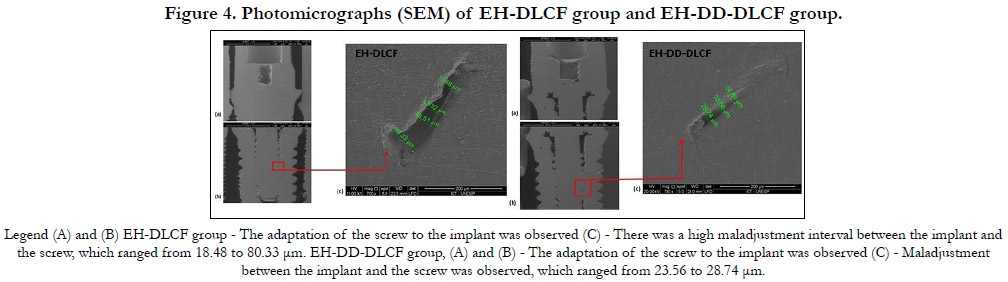
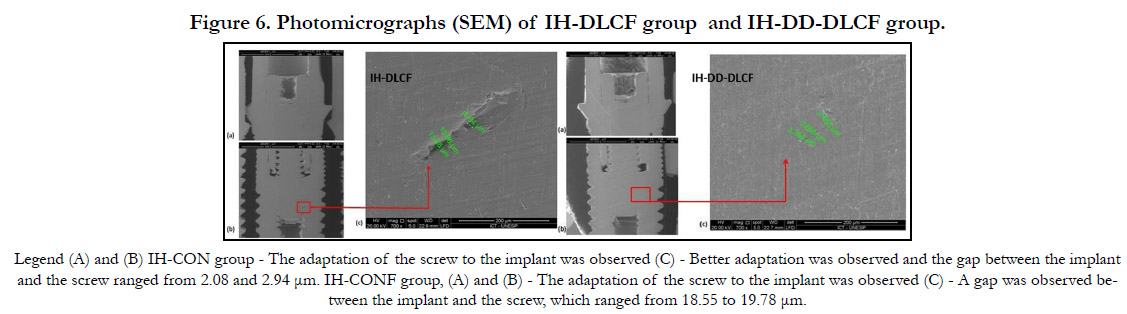
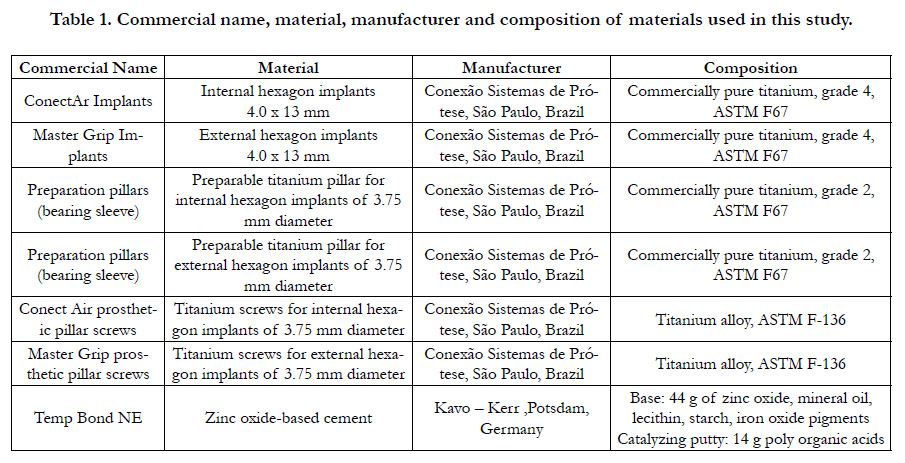
Qualitative analysis: Connection analysis
The DLC and DD-DCL coatings did not interfere in the adaptation
of the screw to the implant (Fig. 3-6). In the connections,
more alterations were observed in EH groups when compared to
IH groups, regardless of screw surface treatment (Fig. 3-6).
For cycled groups, the maladjustments were demonstrated more
frequently in groups with external hexagonal connections (Fig.
3-6). The IH-DD-DLCF group (Fig. 6) presented the lowest gaps
in maladjustment presence. Adding non-cycled groups to comparison,
EH/IH-CON group (Fig. 3) presented the smaller gaps
when compared to the fatigated groups.
Figure 1. Photomicrographs (SEM) of qualitative analysis, Extern Hexagonal connections groups. EH-CON group.
Figure 2. Photomicrographs (SEM) of qualitative analysis, Intern Hexagonal connections groups. IH-CON group.
Table 2. Experimental Groups, mean, standard deviation, coefficient of variance and maintenance torque values expressed in maximum and minimum percentage (%).
Discussion
According to the results of this study, the null hypotheses were
accepted; there were no significant differences among the groups.
The mean value of torque maintenance before the retorque and
mechanical recycling of our samples was described previously
[6]; it was approximately 68%. After complete the experiment,
the mean torque maintenance value was approximately 50%; this
decrease in the removal torque values after retorque and the occlusal
load occurred as expected, regardless of screw type[14] and
these results are following literature [15-17]. The embedment,
with gradual accommodation and adaptation between the contact
interfaces, results in a reduction of the friction coefficient [17].
Besides that, the removal torque values tended to decrease proportionally to the increase in the number of insertion/removal
cycles [16].
It was expected an improvement of torque maintenance in the
experimental coated groups. Dziedzic et al. reported that the carbon
coating on the screw threads reduced the friction in the interface
and improved the preload values [17] and consequently the
clamping force exerted by the abutment on the implant platform.
Due to the low friction coefficient of the DLC, the film should allow
greater preload with the same torque, improving the stability
of the joint [18]. Colpak & Gumus coated abutment screws with
DLC (Oerlikon Balzers) through the plasma vapor deposition
method and reported higher reverse torque values in DLC coated
abutment screws [19].
Additionally, diamond doped DLC films have unique properties
when compared to pure nanocrystalline diamond films or
metal-doped DLC films, which may provide advantages for electrochemical,
optical-window, field emission, or tribological applications
[11]. However, in this research, both coatings presented
similar torque maintenance when compared to uncoated groups.
Contradictory results may be explained by mechanical properties
determined by the method of deposition. Herein we used
PECVD. Each method has its advantages as well as disadvantages
such as high levels of internal stress, poor adhesive properties, or
high sensitivity to ambient conditions [20].
The literature demonstrates that external hexagonal connections
generate higher stress along with the implant, promoting greater
deformations than the internal hexagonal connection, thus IH
has a more favorable biomechanical situation for the prosthetic
performance [21], however, considering the limitations of the
present study, none difference was demonstrated between EH
and IH connections groups. Contradictorily, EH connections
groups demonstrated significant differences while the torque
maintenance values were more stable in the IH groups [6]; there
were no significant differences among IH groups in Lepesqueur’s
study [6]. The authors reported high torque maintenance value in
uncoated screws with external hexagonal connections when compared
to groups coated with diamond-like carbon and coated with
diamond-like carbon doped with diamond nanoparticles [6].
The fatigue simulation of retorqued screws resulted in the increase
of screw surface irregularities, and consequently increased
the coefficient of friction, but decreased the preload of the tightened
joint [22]. There was no screw fracture or loosening of prosthesis
in the presented study, so the stability of the tightened joint
was kept after retorque, which is following literature [23].
Most uncoated screw damages confirm that the DLC film favors
the wearing resistance and protect the coated surface and implant
threads. Coating removal was higher in the DLC nanofilm group
than the DD-DLC group, probably due to the greater roughness
of DLC, even though DLC presented a higher critical load for
delamination [6]. The elevated superficial roughness favors the
coefficient of friction increase, which favors the DLC film removal
during the torque of the screws and retorque procedures.
The granulation of DD-DLC coating over the screws is a characteristic
of this type of coating. The granules were more frequent
in the apical portion of the screw since the deposition process
occurred with the specimen upside-down on a sample-holder; so
this region was favored by the deposition process. The difference
in the number of damages and titanium exposure caused by the
coating removal of screws of different connections was attributed
to the fact that the external hexagonal connection generates high
stress along with the implant, promoting larger deformations than
the internal hexagonal connections [21]. Besides that, the smaller
micro-space found in the internal connection when compared to
the external connection resulted in intimal relation between the
implant and screw surfaces, favoring screwed joint clamping and
promoting coating removal.
Our marginal adaptation findings corroborate with the literature
[23]. The gaps between EH implant-pillar were larger than the
ones observed between IH’s, regardless of screw treatment. The
groups with non-fatigued screws presented smaller gap values,
consequently, their threads promoted better clamping between
the screw and the implant.
A limitation of the study was the lack of rotational misfit measurement.
Additional studies with the use of retorquing in accelerated
life tests, the use of ceramic pillars, and retorqued screws
fracture resistance evaluation should be carried out.
Conclusion
Based on these results, the surface of studied materials (coated/
uncoated) and the type of platform (IH/EH) do not interfere in
the torque maintenance when a retorque is applied.
Acknowledgements & Declarations
RCC thanks the scholarship from Coordination for the Improvement
of Higher Education (CAPES - Coordenação de
Aperfeiçoamento de Pessoal de Nível Superior – Brasil) – Finance
Code 001, in São José dos Campos, Brazil. Authors thanks
Conexão Sistemas de Prótese® (Campinas, SP, Brazil) that provided
the implants to the research.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Availability of data and material
Datasets are available from the corresponding author on reasonable
request. The raw data and all related documents supporting
the conclusions of this manuscript will be made available by the
authors, without undue reservation, to any qualified researcher.
Funding
This work was partly supported by the Coordination for the
Improvement of Higher Education (CAPES - Coordenação de
Aperfeiçoamento de Pessoal de Nível Superior – Brasil) – Finance
Code 001, in São José dos Campos, Brazil.
References
-
[1]. Srinivasan M, Meyer S, Mombelli A, Müller F. Dental implants in the
elderly population: a systematic review and meta-analysis. Clin Oral Implants
Res. 2017 Aug;28(8):920-930. Epub 2016 Jun 7. PubMed PMID:
27273468.
[2]. Araújo PM, Filho GS, Ferreira CF, Magalhães Benfatti CA, Cagna DR, Bianchini MA. Mechanical Complications Related to the Retention Screws of Prefabricated Metal Abutments With Different Angulations: A Retrospective Study With 916 Implants. Implant Dent. 2018 Apr;27(2):209-212. PubMed PMID: 29489548.
[3]. de Moraes SL, Verri FR, Santiago JF Jr, Almeida DA, de Mello CC, Pellizzer EP. A 3-D finite element study of the influence of crown-implant ratio on stress distribution. Braz Dent J. 2013 Nov-Dec;24(6):635-41. PubMed PMID: 24474362.
[4]. Mombelli A, Hashim D, Cionca N. What is the impact of titanium particles and biocorrosion on implant survival and complications? A critical review. Clin Oral Implants Res. 2018 Oct;29 Suppl 18:37-53. PubMed PMID: 30306693.
[5]. Callan DP. Dental implant design and oral and systemic health. Compend Contin Educ Dent. 2007 Sep;28(9):482-4, 486-90, 492. PMID: 17907371. [6]. Lepesqueur LS, de Figueiredo VM, Ferreira LL, Sobrinho AS, Massi M, Bottino MA, Nogueira Junior L. Coating dental implant abutment screws with diamondlike carbon doped with diamond nanoparticles: the effect on maintaining torque after mechanical cycling. Int J Oral Maxillofac Implants. 2015 Nov-Dec;30(6):1310-6. PubMed PMID: 26574857.
[7]. Kim SK, Lee JB, Koak JY, Heo SJ, Lee KR, Cho LR, Lee SS. An abutment screw loosening study of a Diamond Like Carbon-coated CP titanium implant. J Oral Rehabil. 2005 May;32(5):346-50. PubMed PMID: 15842243.
[8]. Wu L, Holloway BC, Beesabathina DP, Kalil C, Manos DM. Analysis of diamond-like carbon and Ti/MoS2 coatings on Ti–6Al–4V substrates for applicability to turbine engine applications. Surface and Coatings Technology. 2000 Aug 21;130(2-3):207-17.
[9]. Hauert R, Thorwarth K, Thorwarth G. An overview on diamond-like carbon coatings in medical applications. Surface and Coatings Technology. 2013 Oct 25;233:119-30.
[10]. Assunção WG, Delben JA, Tabata LF, Barão VA, Gomes EA, Garcia IR Jr. Preload evaluation of different screws in external hexagon joint. Implant Dent. 2012 Feb;21(1):46-50. PubMed PMID: 22228458.
[11]. Lian GD, Dickey EC, Ueno M, Sunkara MK. Ru-doped nanostructured carbon films. Diamond and Related Materials. 2002 Dec 1;11(12):1890-6. [12]. Ivanov MG, Ivanov DM. Nanodiamond nanoparticles as additives to lubricants. InUltrananocrystalline Diamond: Synthesis, Properties and Applications: Second Edition 2012 (pp. 457-492).
[13]. Spazzin AO, Henrique GE, Nóbilo MA, Consani RL, Correr-Sobrinho L, Mesquita MF. Effect of retorque on loosening torque of prosthetic screws under two levels of fit of implant-supported dentures. Braz Dent J. 2010 Jan;21(1):12-7. PubMed PMID: 20464315.
[14]. Farina AP, Spazzin AO, Pantoja JM, Consani RL, Mesquita MF. An in vitro comparison of joint stability of implant-supported fixed prosthetic suprastructures retained with different prosthetic screws and levels of fit under masticatory simulation conditions. Int J Oral Maxillofac Implants. 2012 Jul-Aug;27(4):833-8. PubMed PMID: 22848885.
[15]. Farina AP, Spazzin AO, Consani RL, Mesquita MF. Screw joint stability after the application of retorque in implant-supported dentures under simulated masticatory conditions. J Prosthet Dent. 2014 Jun;111(6):499-504. Epub 2014 Jan 11. PubMed PMID: 24423456.
[16]. Cardoso M, Torres MF, Lourenço EJ, de Moraes Telles D, Rodrigues RC, Ribeiro RF. Torque removal evaluation of prosthetic screws after tightening and loosening cycles: an in vitro study. Clin Oral Implants Res. 2012 Apr;23(4):475-80. Epub 2011 Apr 4. PubMed PMID: 21457352.
[17]. Dziedzic DS, Nhata J, Jamcoski VH, Dziedzic M. Assessment of preload in carbon coated prosthetic screws. RSBO Revista Sul-Brasileira de Odontologia. 2012;9(2):137-42.
[18]. Colpak ED, Gumus HO. Effect of Surface Modifications of Abutment Screws on Reverse Torque Values: An In Vitro Study. Int J Prosthodont. 2020 Jul/Aug;33(4):401-409. PubMed PMID: 32639700.
[19]. Penkov OV, Pukha VE, Starikova SL, Khadem M, Starikov VV, Maleev MV, Kim DE. Highly wear-resistant and biocompatible carbon nanocomposite coatings for dental implants. Biomaterials. 2016 Sep;102:130-6. Epub 2016 Jun 15.PubMed PMID: 27336185.
[20]. Torcato LB, Pellizzer EP, Verri FR, Falcón-Antenucci RM, Santiago Júnior JF, de Faria Almeida DA. Influence of parafunctional loading and prosthetic connection on stress distribution: a 3D finite element analysis. J Prosthet Dent. 2015 Nov;114(5):644-51.Epub 2015 Jul 14. PubMed PMID: 26187105.
[21]. Bulaqi HA, Mousavi Mashhadi M, Safari H, Samandari MM, Geramipanah F. Dynamic nature of abutment screw retightening: finite element study of the effect of retightening on the settling effect. J Prosthet Dent. 2015 May;113(5):412-9. Epub 2015 Mar 4. PubMed PMID: 25749092.
[22]. Montero J, Manzano G, Beltrán D, Lynch CD, Suárez-García MJ, Castillo- Oyagüe R. Clinical evaluation of the incidence of prosthetic complications in implant crowns constructed with UCLA castable abutments. A cohort follow-up study. J Dent. 2012 Dec;40(12):1081-9. Epub 2012 Sep 12. Pub- Med PMID: 22982530.
[23]. Diez JS, Brigagão VC, Cunha L, Neves AC, da Silva-Concilio LR. Influence of diamondlike carbon-coated screws on the implant-abutment interface. Int J Oral Maxillofac Implants. 2012 Sep-Oct;27(5):1055-60. PubMed PMID: 23057017.