Awareness of Antibiotic Prophylaxis Prescription for Patients with Prosthetic Joint Undergoing Dental Implant Placement
Alaa Alqutub1*, Khalid Aboalshamat2, Abrar Demyati1, Amjad Alotaibi3, Lujain Almehmadi4, Sarra Alotaiby5
1 Oral and Maxillofacial Surgery Department, Faculty of Dentistry, Um AlQura University, Makkah 24225, Saudi Arabia.
2 Preventative Dentistry Department, Faculty of Dentistry, Umm Al-Qura University, Makkah 24225, Saudi Arabia.
3 Ministry of Health, khaybar, Saudi Arabia.
4 King Faisal Hospital, Makkah, Saudi Arabia.
5 Ministry of Health, Bisha, Saudi Arabia.
*Corresponding Author
Alaa Alqutub,
Oral and Maxillofacial Surgery Department, Faculty of Dentistry, Um AlQura University, Makkah 24225, Saudi Arabia.
Tel: +966553353365
Fax: +966125270000
E-mail: Awqutub@uqu.edu.sa
Received: September 18, 2021; Accepted: November 13, 2021; Published: November 24, 2021
Citation: Alaa Alqutub, Khalid Aboalshamat, Abrar Demyati, Amjad Alotaibi, Lujain Almehmadi, Sarra Alotaiby. Awareness of Antibiotic Prophylaxis Prescription for Patients with Prosthetic Joint Undergoing Dental Implant Placement. Int J Dentistry Oral Sci. 2021;8(11):5152-5156. doi: dx.doi.org/10.19070/2377-8075-210001035
Copyright: Alaa Alqutub©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Purpose: This study aims to assess dentists' awareness and adherence to professional antibiotic prescribing guidelines, including
clinical practice guidelines from the American Dental Association (ADA) published in 2015, related to performing dental
implant surgeries for patients with prosthetic joints in Saudi Arabia.
Materials and Methods: An observational study utilizing an online validated questionnaire was conducted in Saudi Arabia.
The questionnaire was distributed to 156 general dentists and specialists in Saudi Arabia who are placing dental implants, in
the public and private sectors.
Results: Thirty out of the 156 participants have placed implants for patients with prosthetic joints. Half of the professional
dental personnel (56.40%) reported awareness of the 2015 ADA clinical practice guidelines and (52.60%) applied the guidelines
while treating patients with prosthetic joints.
Conclusion: In our study, dentists who place implants have an average awareness of the clinical practice guidelines for prescribing
antibiotic prophylaxis for prosthetic joints. However, less than 20% of dentists have experience placing implants for
patients with prosthetic Joints; most dentists who place implants are aware and apply the updated guidelines.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Introduction
Dental implants are preferable treatment options to replace missing
teeth [22]. They are bioinert alloplastic material constituted
mainly from pure titanium or titanium alloy that osseointegrate
with maxillary or mandibular alveolar bone [22]. Dental implant
placement is a surgical procedure requiring soft and hard tissue
manipulation [10]. Therefore, patients undergoing this procedure
should be assessed medically to rule out any medical conditions
that can compromise the patients ' health and the desired outcomes
[20].
Prescribing prophylactic antibiotics for healthy and medically
compromised patients who are undergoing dental implant placement
is still controversial [21]. Antibiotics were introduced into
modern medicine in 1928 by Alexander Fleming and they have
been prescribed to treat orofacial infections and as a prophylactic
against transit bacteremia from the oral microflora to other parts
of the body [12, 18]. One of the biggest problems in dental practice
is the high incidence of antimicrobial resistance due to the
empirical prescription of antibiotics without performing cultures
[11]. The development of new strains of bacteria is considered a
global health threat and dentists prescribed almost 10% of antibiotics
published in NHS general practice in 2016 [11]. In Saudi
Arabia, antimicrobial resistance among gram-positive and gramnegative
pathogens has increased [3, 23].
Prosthetic joint infection (PJI) is an uncommon dangerous complication
of the joint replacement procedure [24]. However,
wound contamination at the time of surgery is the most common
cause of early PJI, while bacteremia from distant sites of
infection or following medical and dental procedures may be responsible for late PJI which happens in more than 12 months
postoperatively [16, 19].
Both Staphylococcusaureus and Staphylococcus epidermidis are
determined as the organisms most often found infecting late PJI
[19]. On the other hand, the oral bacteria released following dental
procedures are mostly oral streptococci [16]. These bacteria
released in transient oral bacteremia are rarely found in infecting
prosthetic joints [16]. Nevertheless, several cases have reported
rare late PJI caused by distinct bacterial groups following routine
dental care [17]. These include Streptococcus gordonii which
was seen on the patient's joint aspirate aerobic surgical culture
of a case of late PJI of the knee following vigorous dental flossing
[15]. Recently, a case of a late PJI of the hip following dental
cleaning was caused by the Streptococcus salivarius group, a
member of the Viridans streptococci family [19]. Yet, it can be
concluded that the incidence of PJI caused by oral flora is extremely
rare [15].
Over one million total knee and hip joint replacements are performed
in the United States yearly [16]. As the years go by, the
number of joint replacement surgeries in Saudi Arabia has also
increased but remains lower than in western countries [1].
For the sake of life quality improvement for individuals living
with prosthetic joints and to restrict the widespread use of antibiotics,
the American Dental Association (ADA) and the American
Academy of Orthopedic Surgeons (AAOS) in 2012 have developed
the guidelines for patients with prosthetic joint replacement
and prophylactic antibiotics. In 2015, ADA supported the guidelines
and developed the clinical practice guidelines, stating that
"In general, for patients with prosthetic joint implants, prophylactic
antibiotics are not recommended before dental procedures
to prevent prosthetic joint infection"[21]. The clinical reasoning
for this recommendation is based on evidence that found no association
between dental procedures and PJI or any effectiveness
of prophylactic antibiotics [21]. In addition, the potential harm
of the antibiotic prescriptionincludes antibiotic resistance, anaphylaxis
and opportunistic infection [21]. However, a prophylactic
antibiotic is given in certain circumstances after consultation for
patients with a history of complications associated with their joint
replacement surgery or medically compromised conditions, who
are undergoing the dental procedure with gingival manipulation
[13, 21]. It is essential to determine an appropriate antibiotic regimen
and write the prescriptionrecommended by the orthopedic
surgeon [21].
Several studies have assessed the behavior of antibiotic prescription
with implant surgery procedures [5]. However, the pattern
among specialists is diverse and inconsistent and there is a wide
variety of antibiotics prescriptions regarding the time, dose, and
duration [5, 8]. The current study aims to assess dentists' awareness
and adherence to professional antibiotic prescribing guidelines,
including clinical practice guidelines from the ADA when
performing dental implant surgeries for patients with prosthetic
joints in Saudi Arabia.
Materials And Methods
A cross-sectional descriptive study was conducted using a selfadministered
questionnaire. The research committee approved
this study at the College of Dentistry (Umm Al Qura University,
Makkah, Saudi Arabia, IRB # 174-20). A pilot study was carried
out to validate the questionnaire and it was revised based
on the feedback received from the pilot study.Our sample size
was based on a 95% confidence interval and a 5% error margin.
Self-administered questionnaires were distributed through social
media to 156 general dentists and specialists who performed
dental implants surgeries working in governmental and private
sectors around Saudi Arabia. The questionnaire consists of 18
questions in two sections, including Yes/No questions, multiplechoice
and space for additional comments.The first part included
demographic data of the participants, including gender, nationality,
specialty, level of experience, sector, degree acquiring location,
previous experience of placing implants, and method of communicating
with the patient's physician. The second part consisted
of 11 questions about if the participants have had placed dental
implants for patients with prosthetic joints, knowledge regarding
the relation between PJI and dental implant placement, whether
an antibiotic is routinely prescribed, the antibiotics prophylaxis
protocol according to the clinical practice guidelines of the ADA
for patients with prosthetic joints.
The data were processed using SPSS then the results were tabulated
as numbers and percentages. Multiple linear regression with
backward elimination was used to compare the level of knowledge
with demographic variables.
Results
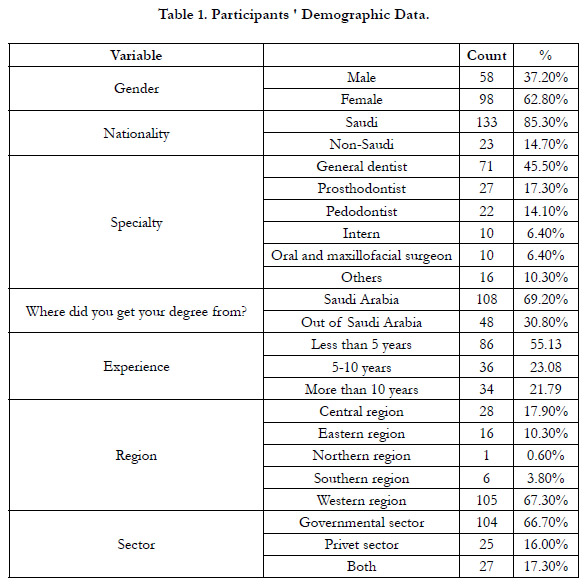
Data from 156 participants were analyzed for this study. Participants'
demographic data are shown in Table 1.
Only 30 (19.20%) participants have placed implants for patients
with prosthetic joints. Around half of the dental professions communicate
with the patient's physician directly via phone or email
(57.10%), while the others communicate with the patient's physician
indirectly via patients themselves (42.90%). Around half of
the dental professions (56.40%) reported awareness of theclinical
practice guidelines of the ADAregarding antibiotic prophylaxis
to patients with prosthetic joints. Also, 52.60% reported applying
them to patients with prosthetic joints, stating that prophylactic
antibiotics are not recommended to prevent prosthetic joint infection.
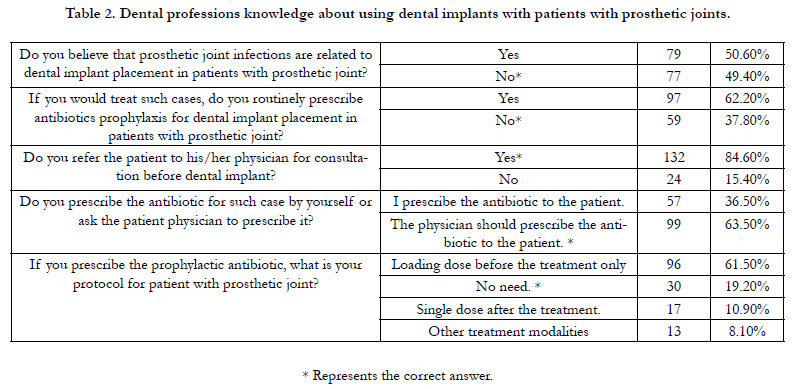
Dental professions were asked five questions regarding
using dental implants with patients with prosthetic joints. Their
answers are shown in Table 2.
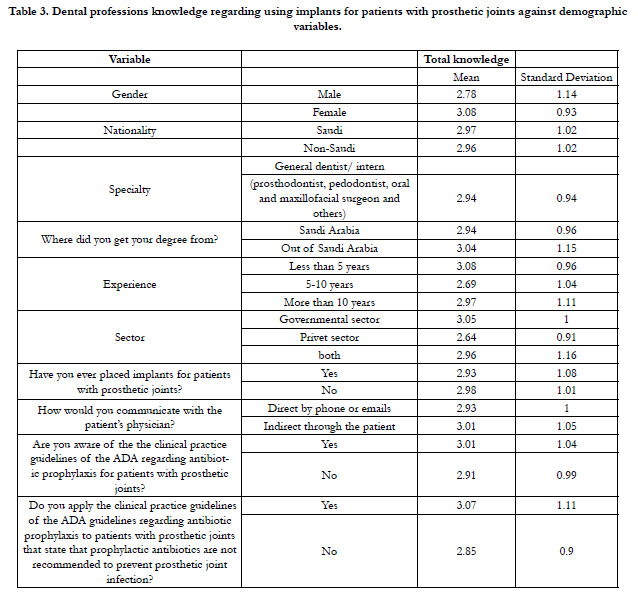
The mean of total correct answers is 2.96 with a standard deviation
of 1.01 points, out of a maximum score of 5. Multiple
linear regression with backward elimination was used to compare
the level of knowledge with demographic variables. None of
the demographic variables or previous experience were significantly
related to the total knowledge score; this includes gender,
nationality, specialty, level of experience, sector, degree acquiring
location, previous experience of placing implants, method of
communicating with patient's physician, reported awareness with
updated guidelines or even applying them. This was confirmed
again by performing bivariate analysis using T-test and ANOVA,
as shown in Table 3.
Table 2. Dental professions knowledge about using dental implants with patients with prosthetic joints.
Table 3. Dental professions knowledge regarding using implants for patients with prosthetic joints against demographic variables.
Discussion
Antibiotic overprescription has led to the emergence of resistant
bacteria worldwide (Fluent et al., 2016). The overuse and misuse of these medications caused a serious issue. In fact, according to
the Centers for Disease Control and Prevention each year in the
U.S., at least 2.8 million people are infected with antibiotic-resistant
bacteria or fungi, and more than 35,000 people die [14]. Also,
antibiotic-resistant infections increase poorer health outcomes,
the use of more toxic treatment, and higher health care costs [7].
Today, it wildly agrees that following the updated guidelines implanted
to improve decision-making and enhance awareness of
the dentists' own prescribing habits regarding antibiotic prophylaxis
is a valuable tool to reduce the rising threat [8]. Furthermore,
prophylaxis antibiotic was administered as a precautionary
measure for dental implant placement for medically compromised
patients such as patients with prosthetic joint replacement and the
fear of PJI [8].
Although the sample size was small, it was representative of a variety of dental professions who placed dental implants and
nearly half of them have reported that they are aware of the updated
guidelines but only (19.20%) have dealt with patients with
prosthetic joints. However, for the surveyed dentists, the demographic
variable or previous experience did not translate into better
knowledge in either the awareness with the clinical practice
guidelines of the ADA or following them.
Along with a survey that conducted in the Western region of Saudi
Arabia to assess the awareness of dental practitioners regarding
the prescription of antibiotics after routine dental extraction reported
that 77% of the dentists would prescribe antibiotics, even
though the majority of dentists are aware of the risk of bacterial
resistance. However, they still believe that taking antibiotics
will prevent odontogenic infections (Al-Sebaei & Jan, 2016). Our
study also concluded that 62.20% had said they would routinely
prescribe antibiotic prophylaxis before dental implant placement.
Another study conducted in Jeddah, Saudi Arabia, shows that
60% of dentists prescribe prophylactic antibiotics routinely before
dental implant placement [8].
In the present study, the protocol of antibiotic administration for
patients with prosthetic joint, 61.50% agree they would prescribe
a loading dose before the treatment. However, 10% suggest that
only a single dose after the treatment is sufficient. In addition,
another study showed that all dentists had prescribed antibiotics
preoperatively of dental implant placement and 41.4% prescribed
a postoperative dose [5]. Moreover, some practitioners prescribe
antibiotics for healthy patients if they undergo multiple implant
surgery with a flap [6]. Because the overprescribing, many authors
urged the need to develop strict guidelines to avoid the misuse of
antibiotics [13]. The present study shows that the majority of the
participants (84.6%) will seek medical consultation with the patients'
physician before the implant surgery regarding the need for
antibiotic prophylaxis. The most common method of communication
was direct via phone or email. This study had some limitations,
including that number of participants was small. However,
we anticipated that participation might not meet targets because
of a coronavirus outbreak during data collection.
Conclusion
The current study found that dentists who place implants are generally
aware of the importance of providing antibiotic prophylaxis
for patients with prosthetic joints. Although only around 20%
of dentists have experienced inserting implants for patients with
prosthetic joints, the majority are aware of and follow the updated
guidelines. Because the guidelines for using prophylactic antibiotics
have changed, different dental professions and patients should
be educated that using prophylactic antibiotics prior to dental implant
treatments is no longer recommended for dental implants
patients with prosthetic joints. This study supports the necessity
for dental professionals to be aware of the updated guidelines
to avoid antibiotic misuse and life-threatening consequences. Following
the updated guidelines will assist in reducing the costs and
morbidity that come with improper antibiotic overuse.
Declaration of Competing Interest
The authors declare that they have no known competing financial
interests or personal relationships that could have influenced the
work reported in this paper.
References
-
[1]. Abd-El-Aziz GS, Gomaa W, Hegaze A, Mustafa HN, Al-Hibshi A, et al.
Analytical study of clinicopathological data of Saudi patients with osteoarthritis
subjected to total knee arthroplasty. Int j morphol. 2019 Sep
1;37(3):1089-94.
[2]. American Dental Association–Appointed Members of the Expert Writing and Voting Panels Contributing to the Development of American Academy of Orthopedic Surgeons Appropriate Use Criteria. American Dental Association guidance for utilizing appropriate use criteria in the management of the care of patients with orthopedic implants undergoing dental procedures. J Am Dent Assoc. 2017 Feb;148(2):57-59. PubMed PMID: 28129802.
[3]. Al Johani SM, Akhter J, Balkhy H, El-Saed A, Younan M, Memish Z. Prevalence of antimicrobial resistance among gram-negative isolates in an adult intensive care unit at a tertiary care center in Saudi Arabia. Ann Saudi Med. 2010 Sep-Oct;30(5):364-9. PubMed PMID: 20697174.
[4]. Al-Sebaei MO, Jan AM. A survey to assess knowledge, practice, and attitude of dentists in the Western region of Saudi Arabia. Saudi Med J. 2016 Apr;37(4):440-5. PubMed PMID: 27052288.
[5]. Al-Kattan R, Al-Shibani N. Current trends in antibiotic prescription behavior among Saudi dentists performing implant surgery: A cross-sectional observational study. J Investig Clin Dent. 2019 May;10(2):e12383. PubMed PMID: 30556379.
[6]. Camacho-Alonso F, Munoz-Camara D, Sanchez-Siles M. Attitudes of dental implantologists in Spain to prescribing antibiotics, analgesics and antiinflammatories in healthy patients. Med Oral Patol Oral Cir Bucal. 2019 Nov 1;24(6):e752-e758. PubMed PMID: 31655835.
[7]. Demirjian A, Sanchez GV, Finkelstein JA, Ling SM, Srinivasan A, Pollack LA, Hicks LA, Iskander JK. CDC Grand Rounds: Getting Smart About Antibiotics. MMWR Morb Mortal Wkly Rep. 2015 Aug 21;64(32):871-3. PubMed PMID: 26292205.
[8]. El-Kholey KE, Wali O, Elkomy A, Almozayen A. Pattern of Antibiotic Prescription for Oral Implant Treatment Among Dentists in Saudi Arabia. Implant Dent. 2018 Jun;27(3):317-323. PubMed PMID: 29652754.
[9]. Fluent MT, Jacobsen PL, Hicks LA; OSAP, the Safest Dental Visit. Considerations for responsible antibiotic use in dentistry. J Am Dent Assoc. 2016 Aug;147(8):683-6. PubMed PMID: 27301851.
[10]. Handelsman M. Surgical guidelines for dental implant placement. Br Dent J. 2006 Aug 12;201(3):139-52. PubMed PMID: 16902543.
[11]. Bunce JT, Hellyer P. Antibiotic resistance and antibiotic prescribing by dentists in England 2007-2016. Br Dent J. 2018 Jul 13;225(1):81-84. PubMed PMID: 30002521.
[12]. HOFFMAN WS. Penicillin; its use and possible abuse. J Am Dent Assoc. 1947 Jan 15;34(2):89-99. PubMed PMID: 20278269.
[13]. Ireland RS, Palmer NO, Lindenmeyer A, Mills N. An investigation of antibiotic prophylaxis in implant practice in the UK. Br Dent J. 2012 Oct;213(8):E14. PubMed PMID: 23099724.
[14]. Kadri SS. Key Takeaways From the U.S. CDC's 2019 Antibiotic Resistance Threats Report for Frontline Providers. Crit Care Med. 2020 Jul;48(7):939- 945. PubMed PMID: 32282351.
[15]. Klein R, Dababneh AS, Palraj BR. Streptococcus gordonii prosthetic joint infection in the setting of vigorous dental flossing. BMJ Case Rep. 2015 Aug 11;2015:bcr2015210695. PubMed PMID: 26264944.
[16]. Little JW. Patients with prosthetic joints: are they at risk when receiving invasive dental procedures? Spec Care Dentist. 1997 Sep-Oct;17(5):153-60. PubMed PMID: 9791294.
[17]. McNally CM, Visvanathan R, Liberali S, Adams RJ. Antibiotic prophylaxis for dental treatment after prosthetic joint replacement: exploring the orthopaedic surgeon's opinion. Arthroplast Today. 2016 Mar 3;2(3):123-126. PubMed PMID: 28326413.
[18]. Oberoi SS, Dhingra C, Sharma G, Sardana D. Antibiotics in dental practice: how justified are we. Int Dent J. 2015 Feb;65(1):4-10. PubMed PMID: 25510967.
[19]. Olson LB, Turner DJ, Cox GM, Hostler CJ. Streptococcus salivarius Prosthetic Joint Infection following Dental Cleaning despite Antibiotic Prophylaxis. Case Rep Infect Dis. 2019 Apr 21;2019:8109280. PubMed PMID: 31143483.
[20]. Schimmel M, Srinivasan M, McKenna G, Müller F. Effect of advanced age and/or systemic medical conditions on dental implant survival: A systematic review and meta-analysis. Clin Oral Implants Res. 2018 Oct;29 Suppl 16:311-330. PubMed PMID: 30328186.
[21]. Sollecito TP, Abt E, Lockhart PB, Truelove E, Paumier TM, Tracy SL, Tampi M, et al. The use of prophylactic antibiotics prior to dental procedures in patients with prosthetic joints: Evidence-based clinical practice guideline for dental practitioners--a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015 Jan;146(1):11-16.e8. PubMed PMID: 25569493.
[22]. Tetè S, Mastrangelo F, Traini T, Vinci R, Sammartino G, Marenzi G, Gherlone E. A macro- and nanostructure evaluation of a novel dental implant. Implant Dent. 2008 Sep;17(3):309-20. PubMed PMID: 18784531.
[23]. Yezli S, Shibl AM, Livermore DM, Memish ZA. Antimicrobial resistance among Gram-positive pathogens in Saudi Arabia. J Chemother. 2012 Jun;24(3):125-36. PubMed PMID: 22759756.
[24]. Young H, Hirsh J, Hammerberg EM, Price CS. Dental disease and periprosthetic joint infection. J Bone Joint Surg Am. 2014 Jan 15;96(2):162-8. Pub- Med PMID: 24430417.