To Comparatively Evaluate Oxygen Saturation Level Among Dental Health Professionals Using 3 Different Types of Masks -N95, KN95 And Surgical Three-Layered Mask
Dr. Ajay Singh Rao1*, Dr. Suwidhi Ranka2, Dr. Unnati Shah2, Dr. Meghna Kothari2
1 Reader, Department of Conservative Dentistry & Endodontics, K M Shah Dental College & Hospital, Sumandeep Vidyapeeth deemed to be University, Vadodara, Gujarat, India.
2 Post Graduate, Department of Conservative Dentistry & Endodontics, K M Shah Dental College & Hospital, Sumandeep Vidyapeeth deemed to be university, Vadodara, Gujarat, India.
*Corresponding Author
Dr. Ajay Singh Rao,
Reader, Department of Conservative Dentistry & Endodontics, K M Shah Dental College & Hospital, Sumandeep Vidyapeeth deemed to be University, Vadodara, Gujarat, India.
Tel: +918385017307
E-mail: drajayinendo@gmail.com
Received: September 18, 2021; Accepted: November 13, 2021; Published: November 24, 2021
Citation: Dr. Ajay Singh Rao, Dr. Suwidhi Ranka, Dr. Unnati Shah, Dr. Meghna Kothari. To Comparatively Evaluate Oxygen Saturation Level Among Dental Health Professionals Using 3 Different Types of Masks -N95, KN95 And Surgical Three-Layered Mask. Int J Dentistry Oral Sci. 2021;8(11):5141-5145. doi: dx.doi.org/10.19070/2377-8075-210001033
Copyright: Dr. Ajay Singh Rao©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To Comparatively Evaluate Oxygen Saturation Level Among Dental Health Professionals Using 3 Different Types of Masks -N95, KN95 And Surgical Three-Layered Mask.
Settings and Design: Double blinded Randomized Clinical Trial
Methods & Materials: Total 90 Dental health professionals were randomly assigned into three groups; Group A-N 95 mask
(3M), Group B-KN 95 mask (3M) and Group C- Surgical three-layered mask (3 ply Surgical mask). The oxygen saturation
level was measured for all the Groups before wearing the mask and after 1 hour wearing the mask using a pulse oximeter
(MedTech).
Results: The statistical analysis showed that there was no significant difference in Pre-op (before wearing mask) &Post-op
(1 hour after wearing mask) in the oxygen saturation level among all three experimental Groups. Although, as an individual
group, Group B (KN95) showed statistically significant change in the oxygen saturation within the same group (Intra group)
pre-op and post-op.
Conclusion: This study confirms the fact that wearing any of these mask (N95, K95 or Surgical) continuously for 1 hour
doesn’t affect the oxygen saturation level. So it can be concluded that for any dental procedure taking up to 1 hour, it is safe
to wear any of the above mentioned mask.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Dental Professionals; KN9 Mask; N95 Mask; Oxygen Saturation; Pulse Oximeter; Surgical Three-Layered Mask.
Introduction
Each system and structure in the body requires oxygen for living.
Without oxygen, cells begin to malfunction, eventually die
ultimately leading to organ failure [1]. Standard oxygen saturation
values are between 95 and 100 percent. Oxygen saturation levels
below 90 percent are considered abnormally low and can be a
clinical emergency [2]. The device used to measure the Oxygen
saturation level is called as ‘Pulse Oximeter’. This device can be
attached to a finger, a wrist, a foot, or any other area where the
device can detect blood supply [3-5].
Health care personnel (HCP) who are routinely exposed to viral
respiratory infections in the workplace may transmit infection
to others [6, 7]. Severe acute respiratory syndrome coronavirus 2
(SARS-CoV-2) is primarily spread via respired airborne droplets
[8, 9].
Dental healthcare professionals cannot always follow the interpersonal
distance of more than a meter and are frequently exposed
to saliva, blood, and other body fluids during surgical procedures.
Moreover, many dental surgical procedures generate aerosol, and
the risk of airborne infection is to be considered higher and hence
spent long time wearing personal protecting equipment especially
a mask [10-12].
The WHO and the United States Centers for Disease Control
and Prevention (CDC) recommend wearing a mask as an essential measure to protect the health personnel from accidental exposure
through nose and mouth. Hence a variety of masks are available
in the market.
An N95 mask is designed to accomplish a tight facial fit and very
effective filtration of airborne particles. Note that the edges of
the mask are designed to form a seal around the nose and mouth
[13].
KN 95 is almost similar to N 95 mask. Both masks are appraised
to capture 95% of minute particles (0.3-micron particles, to be
exact). Both ratings need masks to be tested for filtration effectiveness
at capturing salt particles (NaCl).
Surgical three-layered masks are often referred to as face masks,
although not all face masks are regulated as surgical masks. A surgical
mask is meant to help block large-particle droplets, splatter,
splashes or sprays, that may hold microorganisms (viruses and
bacteria), keeping it away from nose and mouth. Surgical masks
may also help to reduce exposure of saliva and respiratory secretions
to others [14].
Dental health professionals like Surgeons and Endodontists, etc
are often using mask on regular basis and they work for longer period.
Prolong wearing of any kind of mask may cause breathless
or suffocation and may affect the oxygen saturation level.
No literature was available that evaluated and compared effect
of these above-mentioned masks on oxygen saturation levels of
dental healthcare professionals.
Hence, this study aims to Comparatively Evaluate Oxygen Saturation
Level among Dental Health Professionals Using 3 Different
Types of Masks -N95, KN95 And Surgical Three-Layered Mask.
Null hypothesis stated there was no difference in evaluation of
oxygen saturation level among Dental health professionals using 3
different types of masks-N95, KN 95 and Surgical Three-Layered
mask (P value <0.05).
Materials And Methods
CTRI Registration was done as per central trial registry for this
randomized clinical trial (CTRI/2021/03/032201). After obtaining
ethical clearance (SVIEC/ON/DentSRP/20133).
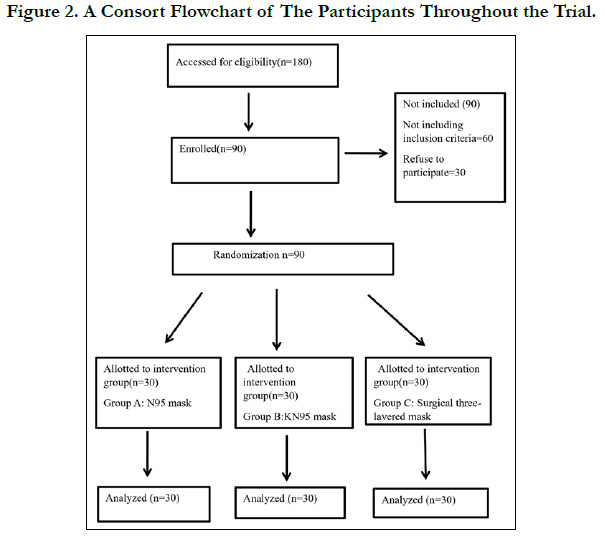
The total sample size required for the study was 90 (30 per group)
achieves 80% power using this formula:
(Zalpha +Zbeta) ^2*Sqrt(n*delta^2/2kS^2)
A total of 90 permanently/provisionally registered dental health
professionals aged 20 to 50 years, having experience of wearing
mask on regular basis were included in the study after obtaining
signed informed consent from all dental health professionals.
Dental health professionals with habit of smoking, pre -oxygen
saturation level less than 91, previous medical history and ongoing
medications, covid -19 recovered and pregnant females were
excluded.
Selected professionals were allocated randomly in 3 groups:
Group A: N 95 mask, Group B: KN 95 and Group C: Surgical
three-layered mask.
Hence study design was randomized double blinded clinical study.
The seat numbers were written on the desk and participants were
asked to sit randomly by maintaining 6ft distance. At a time only
30 Dental health professionals were participating in the study; all
of them were randomly selected for any of the 3 groups (10 per
group).
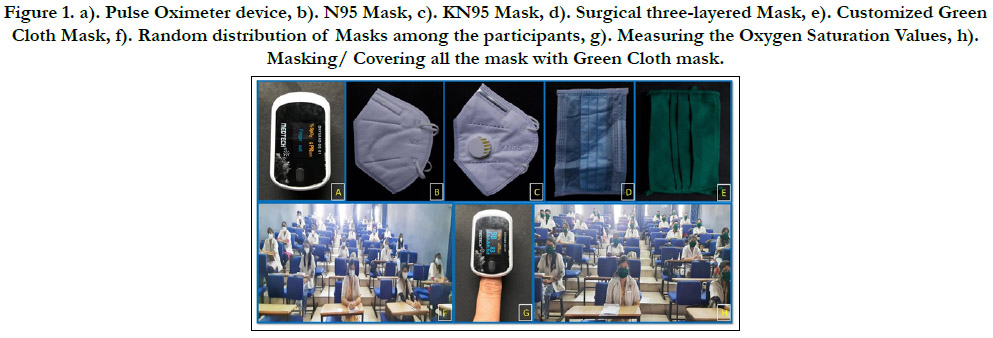
The pulse oximeter (MedTech) with a reusable clip type finger
probe on index finger was used to measure the blood Oxygen
saturation during the study (Fig 1A).
The primary investigator measured the Oxygen saturation level
of all the participants according to the seat numbers. 2 readings
of Oxygen saturation level were recorded and average value was
taken for each participant (Fig 1G).
The co-investigator randomly distributed the masks to each group
respectively. 10- N95 mask (Fig1B); 10- KN95 Mask (Fig1C); 10-
Surgical mask (Fig1D). Allotment of the masks as well as measurements
of oxygen saturation levels of all the participants were
done by the Co-investigator.
The primary investigator was totally unaware (blinded) of mask
distribution procedure to avoid bias. After distributing the mask,
an educational video was played (Fig 1F) for 1 hour (every day
from 10 am -11am for each batch of 30 people.).
After 1 hour when the video ended, the co-investigator gave an
additional green cloth mask (Fig 1E) which were customized and
were large enough to cover the entire surface of the pre-worn
experimental mask on the face (irrespective of the type of mask
they were already wearing) just to keep the primary investigator
blinded (Fig1H) when he comes back to measure the oxygen saturation
after 1 hour.
Now once again, the primary investigator measured the oxygen
saturation level of all the participants according to their seat numbers.
Again, 2 readings of Oxygen saturation level were recorded
and average value was taken for each participant.
Those participants who experienced breathlessness or suffocation
were immediately ask to remove the mask and were excluded
from the study.
Statistical Analysis
The data were entered into spreadsheets, and Statistical analysis
was analysed using one-way ANOVA test for quantitative data
with multiple Tukey tests and categorical data using non parametric
tests. The data was analysed with IBM SPSS 20 for windows
statistical software (P=0.05)
Results
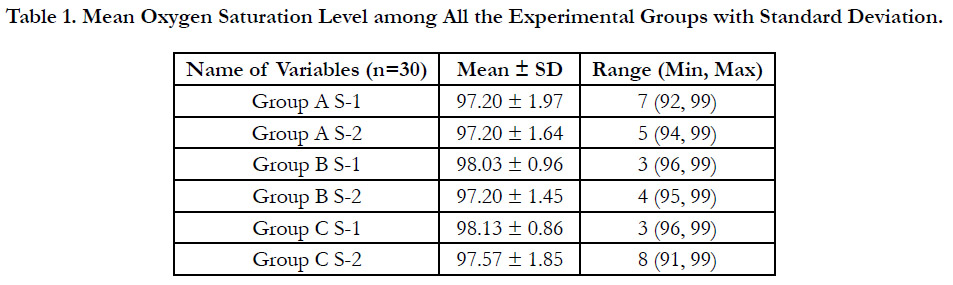
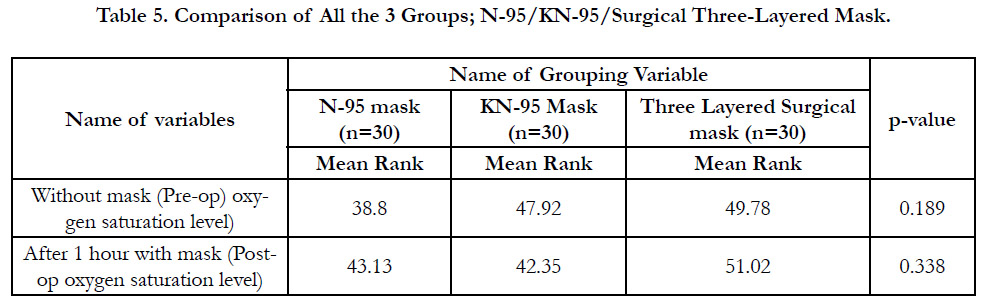
The result states that there is no statistically significant difference
in oxygen saturation level among Dental health professionals using
3 different types of masks-N95, KN 95 and Surgical Three-
Layered mask (P value <0.05).(Table-5)
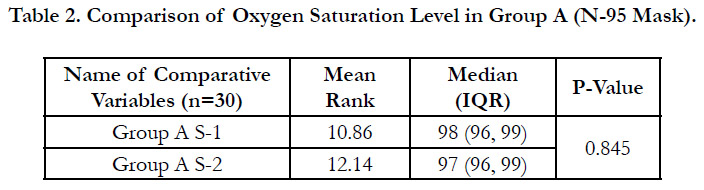
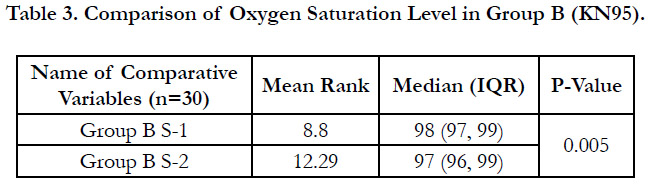
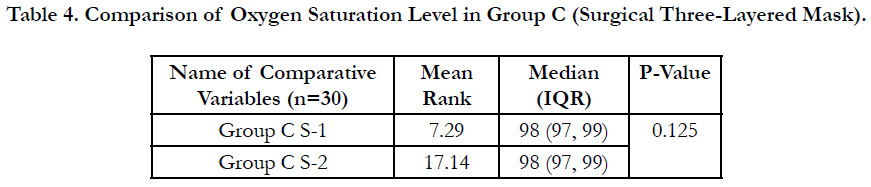
But if we look at the individual groups it shows statistically significant
difference in Group B (KN95) mask at pre and post 1 hour
interval (P<0.005) (Table-1-4).
Figure 1. a). Pulse Oximeter device, b). N95 Mask, c). KN95 Mask, d). Surgical three-layered Mask, e). Customized Green Cloth Mask, f). Random distribution of Masks among the participants, g). Measuring the Oxygen Saturation Values, h). Masking/ Covering all the mask with Green Cloth mask.
Discussion
Oxygen is essential to life. If the supply of oxygen is interrupted,
this energy generating process is curtailed or ceases, with resulting
cell injury and, ultimately, cell death and organ failure. Blood
oxygenation is most frequently measured non-invasively by pulse
oximetry. This allows convenient and safe continuous monitoring
of oxygen saturation in peripheral (capillary) blood (SpO2) [15].
Oxygen saturation can drop for many reasons, including suffocation,
choking, infections: such as pneumonia, Covid 19, drowning
diseases, such as emphysema, lung cancer, and lung infection
gasping poisonous chemicals, heart or a history of heart attack
allergic reactions, general anaesthesia, sleep apnea [14].
Healthcare professionals are always exposed to a high risk of
infection. The WHO and the United States Centers for Disease
Control and Prevention (CDC) recommend a series of essential
protective procedures, such as protective equipment for health
workers during the care of patients with suspected or confirmed
COVID-19, one of the most effective being masks [15, 16].
Dental healthcare professionals cannot always respect the interpersonal
distance of more than a meter and are exposed to
saliva, blood, and other body fluids during surgical procedures.
Moreover, many dental surgeries can generate aerosol, and the
risk of airborne infection is to be considered higher and hence
spent long time wearing personal protecting equipment especially
mask [16-18]. As mentioned earlier, scarcity of literature was seen
that examines the physiological effects of various mask in dental
healthcare professionals.
Depending on their structure and filtering capacity 2 types of
masks: surgical masks and respiratory masks. Surgical three-layered
masks are considered a medical device with a certified nomenclature
of the EN 14683 standard. They are utmost effective
for offering a microbial barrier and resistance to splashes, contributing
a filtration percentage of around 80% [19-21]. It provides
protection in only 1 direction to avoid the transmission of
infectious agents carried by the user. They prevent the passage of
microorganisms present from the inside out; therefore, the use of these masks is recommended for COVID-19 patients [20-23].
However, these surgical three-layered masks do not certify a good
airtight seal, and thereby permit particles to enter around the ends.
The present study resulted that oxygen saturation level in dental
health professional wearing three layered surgical masks before
was mean range of 7.29 and after one hour was 17.14 that did not
elicit a statistically significant difference (P value-0.125) (Table-4).
The usage of N95 masks has been measured a US standard administered
by the NIOSH. These masks are designed to protect
users from air particles, including aerosols [24], with a particle
filtration size of 0.3 microns of 95% and have a lesser amount of
leakage in the face seal due to the close-fitting to the user’s face
[20, 23, 25, 26].
The present study shows that oxygen saturation level in dental
health professional wearing N-95 mask before was mean range of
10.86 and after one hour was 12.14 that did not elicit a statistically
significant difference (P value-0.84).(Table-2)
KN95 masks are accessible in the market and comply with GB
2626-2006 guidelines. These masks have a filtration capacity of
94-95% of particles with 4 overlying coatings, which are attached
together to evade the exit of particles from the carrier and the
aspiration of aerosols that may incorporate the virus.
A study found out that the filter layer of N95 is 8-fold thicker
than that of KN95, which explains its 10% higher filtration efficiency (97.03 %) versus KN95 (87.76 %) [27-30]. Till now, no
studies have been done on physiological effects of KN95 respirators.
The results of present study showed that oxygen saturation
level in dental health professional wearing KN-95 mask before
was mean range of 8.80 and after one hour was 12.29 that did
elicit a statistically significant difference (P value-0.005) (Table-3).
Considering the limitation of the study, comparison of different
type the mask showed that there was not statistically significant
difference in Pre/Post oxygen saturation levels thus the null hypothesis
was accepted in the study.
Conclusion
This study confirms that wearing the mask (N95, K95 or Surgical)
continuously for 1 hour doesn’t affect the oxygen saturation
level. So it can be concluded that for any dental procedure taking
up to 1 hour, it is safe to wear any of the above mentioned mask.
Although in Group B, there was a significant difference found in
pre & post 1 hour oxygen saturation, but that was within the safe
range (average 95%).
Acknowledgements
This study has been registered at ClinicalTrials.gov with ID: CTRI/2021/03/032201.
Limitation
1.Since we evaluated Oxygen saturation level at 1 hour interval,
more studies are required to evaluate at different time intervals.
2.The sample size taken in the present study is relatively small
(90). Hence, studies with larger sample size should be done.
3.Only 3 types of masks were evaluated in the study, other types
of masks such as respirator’s, FFP2 and double masking needs to
be evaluated.
References
-
[1]. Kalogeris T, Baines CP, Krenz M, Korthuis RJ. Cell biology of ischemia/
reperfusion injury. Int Rev Cell Mol Biol. 2012;298:229-317. PubMed
PMID: 22878108.
[2]. Schutz SL. Oxygen saturation monitoring by pulse oximetry. AACN procedure manual for crit care. 2001;4:77–82.
[3]. Neff TA. Routine oximetry. A fifth vital sign? Chest. 1988 Aug;94(2):227. PubMed PMID: 3396392.
[4]. Seifi S, Khatony A, Moradi G, Abdi A, Najafi F. Accuracy of pulse oximetry in detection of oxygen saturation in patients admitted to the intensive care unit of heart surgery: comparison of finger, toe, forehead and earlobe probes. BMC Nurs. 2018 Apr 17;17:15. PubMed PMID: 29692684.
[5]. Plüddemann A, Thompson M, Heneghan C, Price C. Pulse oximetry in primary care: primary care diagnostic technology update. Br J Gen Pract. 2011 May;61(586):358-9. PubMed PMID: 21619771.
[6]. Schutz SL. Oxygen saturation monitoring by pulse oximetry. AACN procedure manual for crit care. 2001;4:77–82.
[7]. Goins WP, Talbot HK, Talbot TR. Health care-acquired viral respiratory diseases. Infect Dis Clin North Am. 2011 Mar;25(1):227-44. PubMed PMID: 21316002.
[8]. Hui DSC, Zumla A. Severe Acute Respiratory Syndrome: Historical, Epidemiologic, and Clinical Features. Infect Dis Clin North Am. 2019 Dec;33(4):869-889. PubMed PMID: 31668196.
[9]. Schoeman D, Fielding BC. Coronavirus envelope protein: current knowledge. Virol J. 2019 May 27;16(1):69. PubMed PMID: 31133031.
[10]. Xerez J, Neto H, Lopes F, et al. Profile of dental students about biosafety. Rev FacOdontol Porto Alegre. 2012;53(1):11-15.
[11]. Uramis MR, Pena Y, Perez A. From biosafety to infection control in ˜ dentistry. Rev CubanaEstomatol. 2014;51(2):224-236.
[12]. Benitez J. On the use or not of masks, as uncertain as the new coronavirus. Rev Exp Med. 2019;5(3):120-121.
[13]. Janssen L, Ettinger H, Graham S, Shaffer R, Zhuang Z. The use of respirators to reduce inhalation of airborne biological agents. J Occup Environ Hyg. 2013;10(8):D97-D103. PubMed PMID: 23767796.
[14]. Jacobs JL, Ohde S, Takahashi O, Tokuda Y, Omata F, Fukui T. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial. Am J Infect Control. 2009 Jun;37(5):417-419. PubMed PMID: 19216002.
[15]. Higgins C. Oxygen saturation–better measured than calculated. [16]. Xerez J, Neto H, Lopes F, et al. Profile of dental students about biosafety. Rev FacOdontol Porto Alegre. 2012;53(1):11-15.
[17]. Uramis MR, Pena Y, Perez A. From biosafety to infection control in ˜ dentistry. Rev CubanaEstomatol. 2014;51(2):224-236.
[18]. Benitez J. On the use or not of masks, as uncertain as the new coronavirus. Rev Exp Med. 2019;5(3):120-121.
[19]. Sigua-Rodriguez EA, Bernal J, Lanata A, et al. COVID-19 and dentistry: a review of recommendations and perspectives for Latin America. Int J Odontostomatol. 2020;14(3):299-309.
[20]. Hirschmann MT, Hart A, Henckel J, Sadoghi P, Seil R, Mouton C. COVID- 19 coronavirus: recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg Sports TraumatolArthrosc. 2020 Jun;28(6):1690-1698. PubMed PMID: 32342138.
[21]. Lepelletier D, Grandbastien B, Romano-Bertrand S, Aho S, Chidiac C, Géhanno JF, Chauvin F; French Society for Hospital Hygiene and the High Council for Public Health. What face mask for what use in the context of COVID-19 pandemic? The French guidelines. J Hosp Infect. 2020 Apr 26;105(3):414–8. PubMed PMID: 32348833.
[22]. Azap A, Erdinç FS. Medical mask or N95 respirator: When and how to use? Turk J Med Sci. 2020 Apr 21;50(SI-1):633-637. PubMed PMID: 32336079.
[23]. Long Y, Hu T, Liu L, Chen R, Guo Q, Yang L, Cheng Y, Huang J, Du L. Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis. J Evid Based Med. 2020 May;13(2):93- 101. PubMed PMID: 32167245.
[24]. Radonovich LJ Jr, Simberkoff MS, Bessesen MT, Brown AC, Cummings DAT, et al; ResPECT investigators. N95 Respirators vs Medical Masks for Preventing Influenza Among Health Care Personnel: A Randomized Clinical Trial. JAMA. 2019 Sep 3;322(9):824-833. PubMed PMID: 31479137.
[25]. Boškoski I, Gallo C, Wallace MB, Costamagna G. COVID-19 pandemic and personal protective equipment shortage: protective efficacy comparing masks and scientific methods for respirator reuse. GastrointestEndosc. 2020 Sep;92(3):519-523. PubMed PMID: 32353457.
[26]. Ma QX, Shan H, Zhang HL, Li GM, Yang RM, Chen JM. Potential utilities of mask-wearing and instant hand hygiene for fighting SARS-CoV-2. J Med Virol. 2020 Sep;92(9):1567-1571. PubMed PMID: 32232986.
[27]. Yim W, Cheng D, Patel SH, Kou R, Meng YS, Jokerst JV. KN95 and N95 Respirators Retain Filtration Efficiency despite a Loss of Dipole Charge during Decontamination. ACS Appl Mater Interfaces. 2020 Dec 9;12(49):54473-54480. PubMed PMID: 33253527.
[28]. Roberge RJ, Coca A, Williams WJ, Powell JB, Palmiero AJ. Physiological impact of the N95 filtering facepiece respirator on healthcare workers. Respir Care. 2010 May;55(5):569-77. PubMed PMID: 20420727.
[29]. Loeb M, Dafoe N, Mahony J, John M, Sarabia A, Glavin V, Webby R, Smieja M, Earn DJ, Chong S, Webb A, Walter SD. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA. 2009 Nov 4;302(17):1865-71. PubMed PMID: 19797474.
[30]. Offeddu V, Yung CF, Low MSF, Tam CC. Effectiveness of Masks and Respirators Against Respiratory Infections in Healthcare Workers: A Systematic Review and Meta-Analysis. Clin Infect Dis. 2017 Nov 13;65(11):1934- 1942. PubMed PMID: 29140516; PMCID: PMC7108111.