Palatal Plate Therapy In Children with Down Syndrome: A Systematic Review Of Literature
Farah Chouchene*, Fatma Masmoudi2, Ahlem Baaziz3, Fethi Maatouk4, Hichem Ghedira5
1 Pediatric and Preventive Dentistry Department, Faculty of Dental Medicine of Monastir, ABCD F Laboratory of Biological, Clinical and Dento-Facial
Approach, University of Monastir, Monastir, Tunisia, Rue HediChekir. Hiboun 5111 Mahdia.
2 Pediatric and Preventive Dentistry Department, Faculty of Dental Medicine of Monastir, Tunisia, Monastir 5119 Tunisia.
3 Professor in Pediatric Dentistry, Pediatric and Preventive Dentistry Department, Faculty of Dental Medicine of Monastir, Monastir, Tunisia, Monastir 5119 Tunisia.
4 Pediatric and Preventive Dentistry Department, Faculty of Dental Medicine of Monastir, Monastir, Tunisia, Monastir 5119 Tunisia.
5 Pediatric and Preventive Dentistry Department, Faculty of Dental Medicine of Monastir, Monastir, Tunisia, Monastir 5119 Tunisia.
*Corresponding Author
Farah Chouchene,
Pediatric and Preventive Dentistry Department, Faculty of Dental Medicine of Monastir, ABCD F Laboratory of Biological, Clinical and Dento-Facial Approach, University of
Monastir, Monastir, Tunisia, Rue HediChekir. Hiboun 5111 Mahdia.
Tel: 0021622821412
E-mail: Farah.pedo@gmail.com
Received: May 18, 2021; Accepted: November 13, 2021; Published: November 22, 2021
Citation: Farah Chouchene, Fatma Masmoudi, Ahlem Baaziz, Fethi Maatouk, Hichem Ghedira. Palatal Plate Therapy In Children with Down Syndrome: A Systematic Review Of Literature. Int J Dentistry Oral Sci. 2021;8(11):5076-5083. doi: dx.doi.org/10.19070/2377-8075-210001022
Copyright: Farah Chouchene©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: The oro-facial abnormalities in children with Down syndrome (DS) can be managed through oro-facial therapy
using a palatal plate. The present review aimed to investigate the frequency, duration, and type of palatal plates with their different
stimulation elements in palatal plates therapy used in early infancy in children with DS.
Methods: Electronic databases including Medline (via PubMed), The Cochrane Library (CENTRAL) and Scopus were
searched. Only studies published in English during the last twenty years describing the effects of palatal plate therapy (PPT)
on oral motor function were included. The ROBINS-I tool was used to assess the quality of the methodology of the included
studies.
Results: Six studies were retained, included a total of 300 children with DS with a mean age ranged between 2 months and 13
years. All children in the PPT reported a significant improvement of the memetic muscles, tongue retraction and significant
longer lip closure. The children in the palatal plate therapy group were treated with modified palatal plates according to Castillo
Morales. Different palatal plates were used, and the PPT frequencies were ranged between 2 and 3 times daily for 5 to 60
minutes with a duration ranged from 12 to 48 months.
Conclusion: All the included studies in the present review, reported that palatal plates designed in accordance with the shape
of Castillo-Morales basic plates when used before 3 months of age and for several minutes a day combination with orofacial
physiotherapy, improved the orofacial disorders in children with DS.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Down Syndrome; Trisomy 21; Palatal Plate Therapy; Orofacial Regulation Therapy.
Introduction
Children with Down syndrome (DS) exhibit peculiar orofacial
features. These orofacial characteristics have a considerable negative
impact on the quality of life, causing problems related to the
performance of daily activities [1-3].
To improve oral motor function of children with DS, a therapeutic
concept, orofacial regulation therapy (OFRT), was developed
and introduced by Castillo-Morales [4, 5].
This therapy aimed to eliminate tongue dysfunctions and improve
the function of the orbicularis oris and mimetic muscles, leading
to improvements in sucking, articulation, swallowing and nasal
breathing [6, 7].
OFRT includes the functional diagnosis of oral sensorimotor
dysfunctions, a special manual facial stimulation program, and
treatment of oral functions with removable activating palatal
plates and other orthodontic appliances [7].
The palatal plate therapy (PPT) was designed to stimulate tongue
movements, to increase mobility of the upper lip improving the
facial musculature tonus and consists of two simultaneous steps:
the first one is the insertion of a palatal plate device and the second
one is a simultaneous orofacial therapy provided by a physiotherapist
or speech-language pathologist [7, 8].
The aim of the present review was to investigate the frequency,
duration, and type of palatal plates with their different stimulation
elements in palatal plates therapy used in early infancy in children
with DS.
Methods
Protocol
The present review was reported according to the principles of
the Preferred Reporting Items for Systematic Reviews and Metaanalysis
(PRISMA) statement [9] and the Cochrane Handbook.
[10].
Review question
The review question was established based on the Participants,
Interventions, Control, and Outcomes (PICO) principles: “In
children with Down’s syndrome, isthe PPT effective, and what
are the frequency, duration and type of stimulation palatal plates
used?” The detailed PICO principles were as follows: 1. Participants:
Children with Down syndromewho received palatal plate.
2. Interventions: Palatal plate therapy. 3. Control: Children with
Down syndromenot having received palatal plate. 4. Outcome:
oral motor function improvement.
Eligibility criteria
Studies were considered eligible if they met the following criteria:
Longitudinal/observational studies or controlled clinical trials
comparing palatal plates treatment in children with down syndrome
(under the age of 18 years) with a control group for at
least 12-month follow-up period describing the type of palatal
plate used.
Evaluating the treatment effect of palatal plates by at least two assessment
methods: a clinical examination or a parental questionnaire
and video recording.
Case series, case reports, studies focusing on adults were excluded.
Search strategy
An electronic literature search was conducted independently by
two authors (FC and FM) using MEDLINE (via PubMed), The
Cochrane Library (CENTRAL) and Scopus databases.
The following search terms and combinations of Medical Subject
Heading terms (MeSh) were used and adapted for each database:
(Down Syndrome OR Trisomy 21) AND (Stimulation plate OR
Palatal plateOR Orthodontic Appliances, Removable OR Dental
appliance) AND (Orofacial OR Orofacial regulation therapy)
AND (Child).
Only articles published in English from the year January 1, 2000,
to March 31, 2020, were included.
The last research was conducted in April 2020.
The two authors (FC and FM) supplemented the electronic search
by a manual research.
The research was also supplemented by tracking citations of the
relevant studies via Google Scholar. A research of the gray literature
was also carried out by the authors to identify any additional
unpublished articles.
Studies selection
Two authors (FC and FM) independently screened the titles and
abstracts of all the records selected from the different databases.
Then, to select the articles that meet the inclusion criteria the two
authors independently screened all the selected full texts and all
the references the included studies. Agreement and discrepancies
between the two authors were resolved by discussion.
Data collection
Two authors (FC and FM) independently collected data from the
collected studies using a data sheet extraction.
The following variables were included: publication details (author
and year), study design, number and age of children, sample size
of test and control group, frequency, duration, and palatal plate
design assessment methods, follow-up period and main outcomes.
All the studies were subject to qualitative analyses.
In the present systematic review, the palatal plate therapy success
was defined on the accomplishment in oral motor function improvement:
longer closed mouth, improved tongue position and
improved muscle function.
Quality assessment
Each included article was assessed independently by the authors
(FC and FM) using the ROBINS-I tool for assessing risk of bias
in non-randomized studies of interventions for seven domains
[11].
Domains one and two covered confounding and selection of
participants into the study, address issues before the start of the
interventions. Domain threecovered the classification of the interventions.
The other four domains covered: biases due to deviations
from intended interventions, missing data, measurement of
outcomesand selection of the reported result.
Each domain was divided into three categories as low risk of bias,
unclear and high risk of bias.
If one or all domains were evaluated to be of low risk;the study
was classified as low risk of bias, if one or more domains were
evaluated to be unknown risk; the study was classified as moderate
risk.
If one or more domains were evaluated to be a high risk; the study was classified as high risk of bias.
Results
Study selection
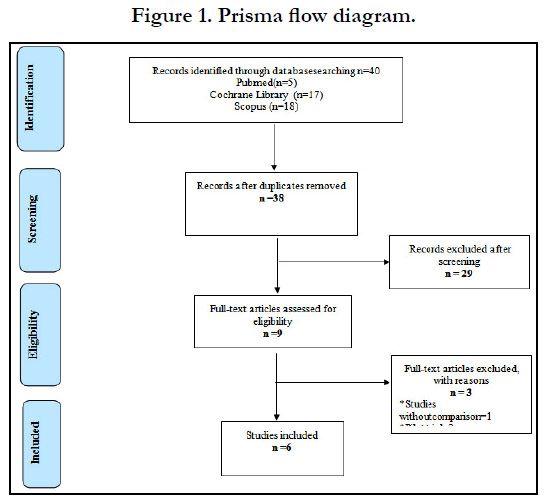
About 40 potentially related titles were derived from the electronic
research (Figure 1).
After removing the duplicates and reviewing the abstract, the full
text of nine studies were retained and compared by the authors
with the inclusion criteria. Of these nine studies, three studies did
not meet the inclusion criteria were excluded and at the final stage
of selection,only six articles were retained for qualitative analyses.
Study characteristics
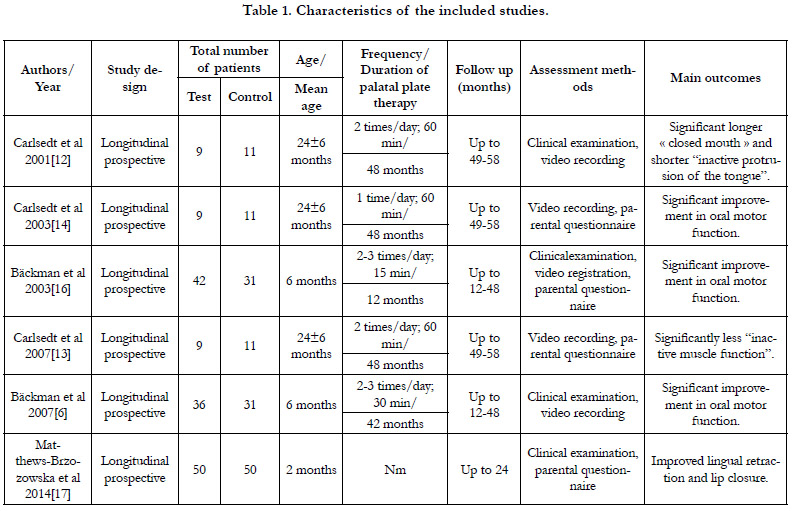
In the present review, six longitudinal prospective studies were
retained (Table 1).
The studies were published between 2001 and 2014. A total
of 300 children with DS with a mean age ranged between two
months and 13 years were included. The test group in all the included
studies was treated with palatal plates therapy when the
control group were children treated only by speech therapy and
physiotherapy. The follow-up period ranged between 12 and 58
months.
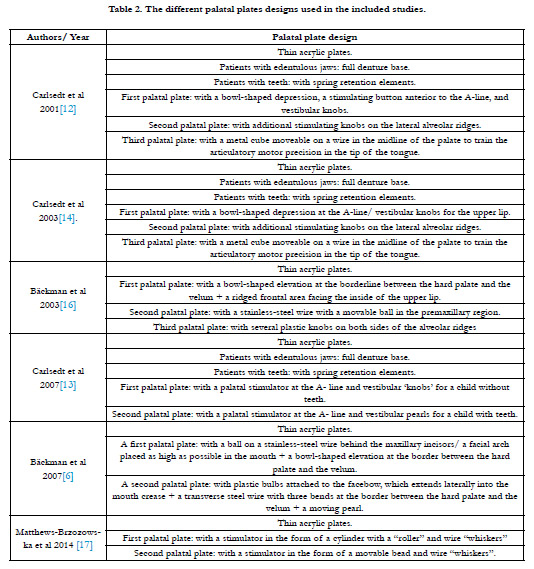
The different palatal plates designs used in the included studies
are summarized in Table 2.
The palatal plate therapy frequencies ranged between two and
three times daily for 5 to 60 minutes with a duration ranged from
12 to 48 months.
The outcomes assessed in all thestudies included oral parameters,
oral motor function, facial expression, tongue position, lip activity
and speech.
The treatment outcomes were evaluated by clinical examination
and video recording in two studies [6, 12] by video recording and
parental questionnaire in two studies, [13, 14] by Clinical examination
and parental questionnaire in one study [15] and by clinical
examination, video registration and parental questionnaire in one
study [16].
Main outcomes
All the included studies reported that the palatal plate therapy
improved orofacial disorders in children with DS.
In the study by Carlsedt et al.conducted in 2001, [12] the PPT was
initiated between the age of 3 and 33 months, and all children
had used the plate for at least 4 years for approximately 1h twice
or three times a day. The palatal plates used in this study were
designed with knobs and/or bowls stimulation areas to enhance
the orofacial function [12].
The first and principally used plate in Carlsedt et al. study [12] was
designedin accordance with Castillo-Morales.
After 4 years of PPT, extraoral examination and video registrationshowed
that children in the palatal plate group had significantly
more rounding lips during speech (P < 0.05). [12]
The mean normal muscle tension recorded was 81.0% ± 11.0%
in the palatal plate group, whereas it was 68.2% ± 22.5% in the
control group [12]
In this study, a statically significant difference was alsoreported
between the groups in the duration of mouth opening and tongue
protrusion (P<0.01)[12].
In the study of Carlsedt et al. conducted in 2003, [14]asignificant
difference between the groups; in visible tongue (P<00.1), visible
tongue during non-speech time (P<00.5) and lip-rounding during
spontaneous speech (P<00.1) were reported.
The palatal plate group showed, during non-speech time, significant
longer period of “closed mouth” (P<00.5)[14].
In this study, PPT was started in children aged between 3 and
33 months with a four-years follow-up (49-58 months) [14]. The
plates were designed with pearls, knobs,and bowls and were used
at least 1 hour twice a day [14].
In this study the most frequently used plates were designed with
a bowl-shaped depression at the line A associated with vestibular
buttons to stimulate the upper lip [14].
After 4 and 5 months, a second palatal plate with additional stimulation
buttons on the lateral alveolar ridges to stimulate the lateral
edges of the tongue was used.For older children for a period of
five months a third plate with a movable metal cube on a wire at
the level of the palate to stimulate the tip of the tongue was used
[14].
In Carlsedt et al. study conducted in 2007, [13] the palatal plate
therapy was initiated in children aged between 3 and 33 months
with a follow-up of at least four years.
The palatal plates used were designed in accordance with the
shape of Castillo-Morales basic plates, as full denture base for
children with edentulous jaws and with spring retentions when
children had teeth [13].
The plates used for approximately one hour twice a day aimed
to increase the tongue activity and to stimulate the upper lip[13].
The results of this study, showed that after one year of using the
palatal plate, a significant increase of mouth closure (P<00.1), and
tongue protrusion (P<00.1) were found [13].
In the study of Ba¨ckman et al. [6, 16] results showed that PPT
improved the oral motor performance and prerequisites for articulation.
In Ba¨ckman et al. study, [16] the palatal plates were used two to
three times daily for 15 minutesin addition but not during speech
therapy exercises.
Three different palatal plates were used. Although the plates were
used for only an average of 15 minutes per day, the repeated
short-time stimulation seems to have been beneficial [16].
The first palatal plate used between 6 and 10 months of age, was
designed to stimulatenormalized position of the tongue and lips
[16].
The second palatal plate used between the age of 10 and 14
months, in addition to the stimulation areas in the first plate, had
a stainless-steel wire with a movable ball to stimulate lip closure,
retraction and lateral movements of the tongue [16].
The third palatal plate used by Ba¨ckman et al.[16] between 14 and
18 months of agewas designed to stimulate tongue retraction and
lip closure.
During PPT, no negative effects of the plates were noticed by
the authors, but some of the palatal plates had to be adjusted to
enhance retention either by rebasing or by using adhesive and in
minority of cases by making a new plate [6, 12-14, 16, 18].
A special problem in the design of the second plate was noticed
by Ba¨ckman et al [16]. Indeed, the arch wire facilitated the removal
of the plate by the child.
In the second study of Ba¨ckman et al.[6] children with DS were
treated with palatal plate from the age of 6 months, the palatal
plates were used two to three times daily for 30 minutes not during
speech therapy exercises. Only two different types of palatal
plates were used by Ba¨ckman et al [6].
The first palatal plate, intended for use until the age of 30 months,
was designed to stimulate the tongue and to improve lip closure
[6].
The second palatal plate intended for use between 30 and 48
months, was designed to stimulate lip closure, and mobility of the
lateral and dorsal parts of the tongue [6].
In the study of Matthews-Brzozowska et al. [15] children were
assessed by clinical examination and parental questionnaire and
reported an improvement of the memetic muscles, tongue retraction
and lip closure.
Two types of palatal plates were used one with a stimulator in
the form of a cylinder with a “roller” and wire “whiskers” and
one with a stimulator in the form of a movable bead and wire
“whiskers”[15].
The results showed that the plate with a “roller” produced best
results in lip closure, memetic muscles, and tongue retraction [15].
Quality assessment
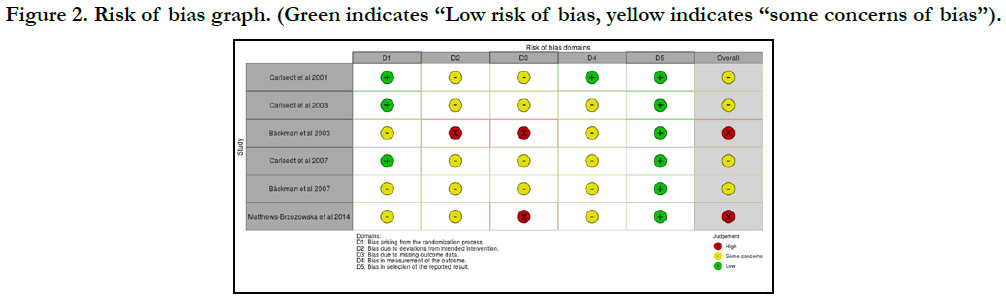
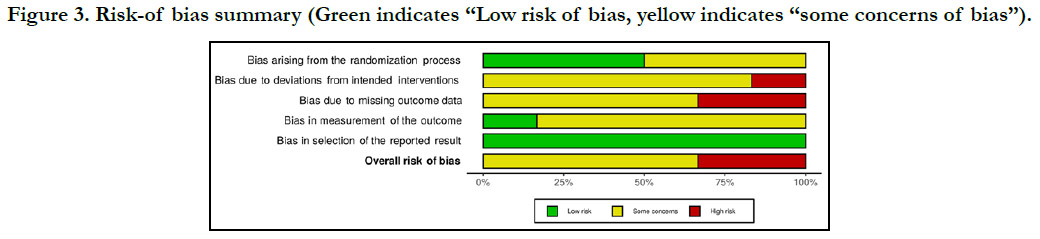
The risk of bias assessment summarized in Figures 2 and 3 were
generated by the robvis (visualization tool) which is a web application
designed for visualizing risk-of-bias assessments [19].
The quality of the included articles in the present review was
overall low. Although all the included studies described an improvement
in oral motor functions as well as a satisfactory effect
of the therapies followed, no clear consensus describing the
evaluation methods of these therapies has been well explained
and described. Assessment methods, plate designs, and treatment
times differ considerably in each study. Different variables of orofacial
functions were evaluated in each selected study.
Four included studies [6, 12-14] had moderate risk of bias as the
patients were randomized into control and treatment groups.
However, in these studies a non-standardized method was used,
and a large individual variation in the groups was identified. One
study [16] had high risk of bias, in this study no drop out informations
and a large variation in the study sample size were reported.
Figure 2. Risk of bias graph. (Green indicates “Low risk of bias, yellow indicates “some concerns of bias”).
Figure 3. Risk-of bias summary (Green indicates “Low risk of bias, yellow indicates “some concerns of bias”).
Discussion
Children with DS can present some orofacial features that, when
not treated and corrected, may interfere with their physical, psychological,
and social development [8].
The most common rehabilitation method for orofacial disorders
in patients with DS is the orofacial regulation therapy created by
Castillo Morales. The Castillo Morales method, combining elements
of sensorial rehabilitation, speech therapy exercises, activation
of mimic muscles and orthopedic treatment, has shown its
effectiveness in the treatment of orofacial neuromotor dysfunctionsfrom
the first days after birth [20-22].
This method consists of modeling exercises and therapeutic
exercises that prepare for good swallowing, stimulate neuromotor
trigger points of the face, activate mimic muscles and evoke
movements related to swallowing, chewing, articulation, closing
lips and tongue retraction [22-24].
The dentist’s role in orofacial therapy is the provision of palatal
plate therapy, which aims to improve oral musculature function
and hypotonia by stimulating the lip, tongue muscles and muscles
of mastication. Castillo-Morales designed the original palatal
plate. These appliances made of thin acrylic usually includes two
stimulators; posterior or lingual stimulators and a bowl-shaped
elevation at the border line between the hard palate and the velum
and it can be oval or round.This type of stimulator is usually
addedto the first plate used in the youngest children aged 3
months and with the third plate used in children aged from 9 to
13 months.
A Bead-type activator located in a more anterior position is generally
added to the second plate used in children aged from 6
to 9 months. Anterior or vestibular stimulators (ridges, knobs…)
positioned at the frontal-alveolar labial aspect of the plate ridges
varying in number, depth and thickness can be included in these
plates. Complementary activators can also be included in palatal
plates and most often with the third plates. These activators can
be pips or/and granulations located unilaterally or bilaterally. In
this third plate, a crater can also serve as activator [22, 24, 25].
Carlstedt et al. [12, 13] noted a significant improvement in mouth
closure after four years of treatment with PPT and a significant
reduction in tongue protrusion values during speech and nonspeech
activities.
Carlstedt et al.[14] reported also a statistically significant improvement
in facial expression with the palatal plate therapy group.
In the study of Carlstedt et al., the PPT was started between the
age 3 and 33 for 4 years for at least 1 hour twice a day, with palatal
plates designed with stimulation areas as knobs, pearls, and bowls
[14].
Treatment with PPT according to Castillo-Morales in Carlstedt
et al. studies [12-14] reported normalized position of the tongue,
muscle conditions and mouth closure, also language training and
articulation were more developed in children treated with PPT.
Ba¨ckman et al. [6,16] reported also a significant improvement in
facial expression and pre-requisites for speech.
In Ba¨ckman et al. studies [6,16] children with DS have been also
treated from the age of 6 months, with palatal plate used two to
three times a day for 30 minutes and in addition to speech therapy
exercises.
Matthews-Brzozowska et al. [15] reported a very important improvement
of the not only in tongue retraction and lip closure bit
also in memetic muscles.
Two different types of palatal plate were used and the results
showed that the plate with a cylinder with a “roller” produced the
best results about lip closure, and memetic muscles. The tongue
retraction was more pronounced after the use of a movable bead
but the duration and frequency of PPT was not specified.
In all the include studies in the present review, no negative effects
of the plaques were noted, but since the children are young and
growing, it was essential to adjust the used palatal plaques to improve
their retention and for some children making new adapted
plates was necessary.
All the included studies showed a visible improvement in oral motor
functions in children with DS. However, the results showed
that the effect of palatal plate therapy was achieved only in addition
to speech therapy and/or orofacial regulation therapy and
physiotherapy.
Indeed, to be effective, PPT must start as soon as possible from
the age of 3 months (before the age of 6 months) and until the
age of 4 years.
Different types of plates can be used depending on the child's age
and dentition.
For best results, the palatal plate should be used at least twice a
day for a few minutes (at least 30 min).
The palatal plates should be designed in accordance with the
shape of Castillo-Morales basic plates. Different type of simulators
can be integrated into the plates: ridges, knobs or bowls.
Complementary activators can also be included in palatal plates,
these activators can be substantial pips and granulations.
The included studies reported that the PPT was effective in improving
orofacial disorders in children with DS, but, the nonstandardized
studies design used and the large individual variation
in the groups identified using different palatal plate design leaded
to some bias risks.
The mean age of DS children at the start of studies ranged from
2 months to 13 years and the duration of palatal plate therapy
ranged from 12 to 58 months which make difficult to interpret the
findings for ideal treatment age and duration.
The treatment outcomes were evaluated by non-standardized
methods such as clinical examination, video recording and parental
questionnaire. These methods would be more reliable if the
examiners were calibrated and blinded.
Within these limitations, results suggest that early PPT in children
with DS implied favorable results but further trials with standardized
evaluation methods are recommended.
Conclusion
Various techniques of myofunctional stimulation and device therapy
have been proposed over the past 25 years to prevent orofacial
dysfunctions in infants and children with SD.
Among these techniques, palatal plate therapy has been suggested
and has been found to be effective in improving these orofacial
disorders if it is provided at a very young age and in collaboration
between speech therapists, physiotherapists and dentists.
Numerous types of plates designed according to the shape of
the Castillo-Morales base plates have been shown to be effective
when used before the age of 3 months for several minutes per day
in addition to speech therapy exercises.
Limitations
No consensus regarding the methods of evaluation in palatal
plates treatment was described in the included studies. Different
methods of evaluation such as clinical examination, video
registration and/or parental interview were used in the studies but none of these used methods are standardized. In addition,
children with this syndrome may present individual variations,
specific characteristics, and various clinical symptoms, although
no included study mentioned the aspect of individual variation
between the different children.
The non-randomized clinical studies included in the present review
did not allow to answer the complex question regarding the
start of treatment or the treatment duration, for this reason further
research is required.
References
-
[1]. Limbrock GJ, Fischer-Brandies H, Avalle C. Castillo-Morales' orofacial
therapy: treatment of 67 children with Down syndrome. Dev Med Child
Neurol. 1991 Apr;33(4):296-303. PubMed: 1828445.
[2]. Svensson H, Eriksson I. Oral motor therapy with palatal plates in children with Down syndrome.2017:38.
[3]. Marques LS, Alcântara CE, Pereira LJ, Ramos-Jorge ML. Down syndrome: a risk factor for malocclusion severity? Braz Oral Res. 2015;29:44. PubMed PMID: 25760064.
[4]. Limbrock GJ, Castillo-Morales R, Hoyer H, Stöver B, Onufer CN. The Castillo-Morales approach to orofacial pathology in Down syndrome. Int J Orofacial Myology. 1993 Nov;19:30-7. PubMed PMID: 9601231.
[5]. Alacam A, Kolcuoglu N. Effects of two types of appliances on orofacial dysfunctions of disabled children. The British Journal of Development Disabilities. 2007 Jul 1;53(105):111-23.
[6]. Bäckman B, Grevér-Sjölander AC, Bengtsson K, Persson J, Johansson I. Children with Down syndrome: oral development and morphology after use of palatal plates between 6 and 48 months of age. Int J Paediatr Dent. 2007 Jan;17(1):19-28. PubMed PMID: 17181575.
[7]. Macho V, Coelho A, Areias C, Macedo P, Andrade D. Craniofacial features and specific oral characteristics of Down syndrome children. Oral Health Dent Manag. 2014 Jun;13(2):408-11. PubMed PMID: 24984656.
[8]. Chad L. Critical Review: What are the effects of palatal plate therapy on orofacial features and speech in children with Down syndrome? In 2013.
[9]. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. PubMed PMID: 19621072.
[10]. Higgins JPT. Cochrane Handbook for Systematic Reviews of Interventions [Internet]. [cited 2021 Apr 14]. Available from: /handbook/current
[11]. Risk of bias tools - ROBINS-I tool [Internet]. [cited 2021 Apr 14]. Available from: https://www.riskofbias.info/welcome/home
[12]. Carlstedt K, Henningsson G, McAllister A, Dahllöf G. Long-term effects of palatal plate therapy on oral motor function in children with Down syndrome evaluated by video registration. ActaOdontol Scand. 2001 Apr;59(2):63-8. PubMed PMID: 11370751.
[13]. Carlstedt K, Henningsson G, Dahllof G. A longitudinal study of palatal plate therapy in children with down syndrome. Effects on motor function. Journal of Disability and Oral Health. 2007;8(1):13.
[14]. Carlstedt K, Henningsson G, Dahllöf G. A four-year longitudinal study of palatal plate therapy in children with Down syndrome: effects on oral motor function, articulation and communication preferences. Acta Odontol Scand. 2003 Feb;61(1):39–46.
[15]. Matthews-Brzozowska T, Cudzilo D, Walasz J, Kawala B. Rehabilitation of the orofacial complex by means of a stimulating plate in children with Down syndrome. AdvClinExp Med. 2015 Mar-Apr;24(2):301-5. PubMed PMID: 25931364.
[16]. Bäckman B, Grevér-Sjölander AC, Holm AK, Johansson I. Children with Down Syndrome: oral development and morphology after use of palatal plates between 6 and 18 months of age. Int J Paediatr Dent. 2003 Sep;13(5):327-35. PubMed PMID: 12924988.
[17]. Matthews-Brzozowska T, Walasz J, Matthews-Kozanecka M, Matthews Z, Kopczynski P. The role of the orthodontist in the early simulating plate rehabilitation of children with Down syndrome.Journal of Medical Science. 2014 Jun 30;83(2):145-51.
[18]. Carlstedt K, Dahllöf G, Nilsson B, Modéer T. Effect of palatal plate therapy in children with Down syndrome. A 1-year study. Acta Odontol Scand. 1996 Apr;54(2):122-5. PubMed PMID: 8739145.
[19]. McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021 Jan;12(1):55-61. PubMed PMID: 32336025.
[20]. Oliveira AC, Pordeus IA, Torres CS, Martins MT, Paiva SM. Feeding and nonnutritive sucking habits and prevalence of open bite and crossbite in children/ adolescents with Down syndrome. Angle Orthod. 2010 Jul;80(4):748- 53. PubMed PMID: 20482363.
[21]. Klingel D, Hohoff A, Kwiecien R, Wiechmann D, Stamm T. Growth of the hard palate in infants with Down syndrome compared with healthy infants- A retrospective case control study. PLoS One. 2017 Aug 10;12(8):e0182728. PubMed PMID: 28796822; PMCID: PMC5552113.
[22]. Korbmacher H, Limbrock J, Kahl-Nieke B. Orofacial development in children with Down's syndrome 12 years after early intervention with a stimulating plate. J OrofacOrthop. 2004 Jan;65(1):60-73. English, German. Pub- Med PMID: 14749890.
[23]. Rao D, Hegde S, Naik S, Shetty P. Malocclusion in Down syndrome - a review. 70(1):4.
[24]. Korbmacher HM, Limbrock JG, Kahl-Nieke B. Long-term evaluation of orofacial function in children with Down syndrome after treatment with a stimulating plate according to Castillo Morales. J ClinPediatr Dent. 2006 Summer;30(4):325-8. PubMed PMID: 16937860.
[25]. Hoyer H, Limbrock GJ. Orofacial regulation therapy in children with Down syndrome, using the methods and appliances of Castillo-Morales.ASDC J Dent Child. 1990 Nov-Dec;57(6):442-4. PubMed PMID: 2147926.