Long Term Evaluation Of Modified Mucogingival Flap Technique With Novel Fish Derived Collagen Matrix And Connective Tissue Graft In Treatment Of Multiple Mandibular Class III Gingival Recession Defects- A Retrospective Study
Lakshmi Ramachandran1*, Harinath parthasarathy2, Anupama Tadepalli3
1 SRM Dental College, Ramapuram, Chennai, India.
2 SRM Dental College, Ramapuram, Chennai, India.
3 SRM Dental College, Ramapuram, Chennai, India.
*Corresponding Author
Lakshmi Ramachandran,
SRM Dental College, Ramapuram, Chennai, India.
Tel: +91 9884690298
E-mail: drlak.84@gmail.com
Received: September 21, 2021; Accepted: October 24, 2021; Published: November 03, 2021
Citation: Lakshmi Ramachandran, Harinath parthasarathy, Anupama Tadepalli. Long Term Evaluation Of Modified Mucogingival Flap Technique With Novel Fish Derived Collagen Matrix And Connective Tissue Graft In Treatment Of Multiple Mandibular Class III Gingival Recession Defects- A Retrospective Study. Int J Dentistry Oral Sci. 2021;8(10):4892-4896. doi: dx.doi.org/10.19070/2377-8075-21000989
Copyright: Lakshmi Ramachandran©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Achievement of root coverage in advanced gingival recession defects involving multiple mandibular anterior
teeth is often challenging. Long-term outcomes of xenogeneic collagen matrices and their effectiveness in comparison to connective
tissue grafts need to be explored.
Aim: To assess and compare the long-term outcomes of xenogenic collagen matrix or connective tissue grafts in conjunction
with the modified mucogingival flap procedure (MMGF) in the treatment of multiple mandibular gingival recession defects.
Materials and Methods: 38 systemically healthy patients presenting with multiple mandibular Miller’s class III gingival recession
were treated using MMGF along with either connective tissue graft (n=20) or xenogenic collagen matrix(n=18). Subjects
were followed up for 3 years post intervention. At the end of 3yrs, 30 subjects were examined for assessment of the changes
in recession height (RH), keratinized tissue width (KT), attached gingiva (AG), relative vestibular depth (RVD) and root coverage
percentage (RC%).
Results: Statistically significant improvement in all clinical parameters were noted in both test and control subjects at the end
of 1 and 3 years (p< 0.05). MMGF + CTG treated sites demonstrated a significantly greater RC% of 67.10 ± 22.90% than
MMGF +XCM sites (35.51 ± 16.14% ) at the end of 3 years (p<0.05).
Conclusion: Xenogenic collagen matrix along with MMGF yielded short term improvement in terms of root coverage than
when compared to the connective tissue graft while treating advanced multiple recession defects.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Gingival Recession; Mandible; Collagen Matrix; Connective Tissue Graft; Retrospective Study.
Introduction
Gingival recession is a composite phenomenon often associated
with other mucogingival conditions complicating therapeutic outcome
[1]. The anterior mandible is a challenging area for clinicians
especially when multiple gingival recessions are present. Association
of frenal pull, shallow vestibule, thin gingival biotype and
inadequate attached gingiva adversely influences the outcome of
conventional root coverage procedures [2]. There is significant
literature evidence indicating that mucogingival surgeries in recession
sites without interdental bone loss are more predictable in
achieving complete root coverage (Cairo et al. 2008, 2014, Chambrone
et al. 2012) [3, 4]. Inter-dental bone loss has been identified
as a major impediment in achieving complete root coverage (Miller
1985 & Wennstorm 1996) [5, 6]. Furthermore, a recent systematic
analysis by Fernandez et al 2021 revealed that long-term root
coverage stability is not guaranteed while treating Miller's Class III
recession and suggested the lack of insufficient clinical trials with
follow up beyond 12 months [7].
Subepithelial connective tissue graft CTG is considered as the
gold standard graft in mucogingival surgeries. However, procuring
an adequate dimension of graft is technically difficult in management
of multiple recessions especially in patients with a thinner
biotype. To overcome these limitations, newer biomaterials have been studied widely. Clinical trials employing xenogeneic collagen
biomaterials showed promising results as barrier membranes, as a
carrier for growth factors, in socket augmentation and also to enhance
keratinized tissue around implants [8]. Xenogenic collagen
matrix derived from marine origin, had been used previously in
socket augmentation and as an apical barrier in the management
of open apex [9-12]. This minimally cross linked type I collagen
matrix enhances wound healing and formation of granulation tissue,
thereby providing an ideal scaffold for regeneration and soft
tissue augmentation.
The scientific evidence on the long-term clinical effects of surgical
treatment of multiple recession defects in the anterior mandible is
limited. The aim of this retrospective study was to determine the
long-term clinical outcomes of the modified mucogingival flap
technique MMGF along with the use of connective tissue graft
(CTG) or xenogenic collagen matrix (XCM) in the treatment of
multiple mandibular Miller's Class III gingival recession defects.
Materials And Methods
The research protocol was approved by the institutional ethical
committee and review board. The treatment was carried out in
accordance with the principles of the declaration of Helsinki. All
the surgical procedures were carried out by a single experienced
periodontist between Jan 2015 and April 2017. 38 subjects presenting
with multiple miller’s class III gingival recession in mandibular
anterior teeth were treated using MMGF along with either
connective tissue graft (n=20) or xenogeneic collagen matrix
(n=18). Baseline details of subjects were retrieved from records
of the department of Periodontics. All the included subjects had
acceptable oral hygiene compliance during or after phase ? therapy
and were non smokers. Treated sites had periodontal probing
depth < 4mm, with absence of tooth mobility, caries, cervical
abrasion/restorations.
Clinical parameters such as recession height (RH), probing pocket
depth (PPD), clinical attachment level (CAL), width of attached
gingiva (AG), width of keratinized tissue (KT), relative vestibular
depth (RVD) were measured by using customized acrylic
stent with UNC 15 periodontal probe and expressed in nearest
mm. Recession height (RH) was measured as the distance from
cemento-enamel junction to gingival margin at the mid buccal
position of each site. Probing pocket depth (PPD) was defined
as the distance from gingival margin to base of the gingival sulcus
at the mid buccal position. Clinical attachment level (CAL)
was recorded as the distance from the cemento – enamel junction
to the base of the gingival sulcus. Keratinized gingiva (KT) was
noted as the distance from the gingival margin to the mucogingival
junction (evaluated using a chemical method –Lugol’s Iodine).
Attached gingiva (AG) was calculated by subtracting the probing
depth from the width of keratinized tissue. Relative vestibular
depth (RVD) was measured as the distance from base of stent to
the deepest position of the vestibule. Root coverage percentage
(RC%) was calculated according to the following formula.
Root coverage = [preoperative vertical recession height - postoperative
vertical recession height]/preoperative vertical recession
height] x 100
At baseline, a single investigator was calibrated with intra examiner
agreement (k=98%), and all clinical parameters were tested
by the same researcher at all time points.
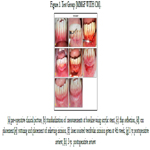
Intervention
After completion of cause related therapy study participants were
randomly treated with modified mucogingival flap (MMGF) technique
along with either connective tissue graft or xenogenic collagen
matrix (Control group), BIOFIL SPONGE® type I collagen
(Test group). The modified mucogingival flap technique MMGF
employed in this study was adapted from Marggraf ’s coronally
repositioned flap with a vestibuloplasty incision, modified from
Edlan & Mejcher technique to deepen the vestibule[13].Under
local anesthesia, horizontal crevicular incisions were made with
the help of scalpel using #15 C blade at the marginal gingiva of
involved teeth and laterally extended to one tooth on either side.
A full thickness mucoperiosteal flap was elevated beyond the
mucogingival junction relieving frenal/muscle attachments. Root
planning was carried out using curettes and recipient site dimensions
were measured using graduated periodontal probe. In the
control sites, connective tissue graft was harvested from the palate
using the single incision technique and the obtained graft was
trimmed to remove the fatty glandular tissue if present. In the test
group, sterile collagen matrix was trimmed in such a way that the
graft extends 2mm laterally and apically beyond the defect. The
CTG/XCM was placed on to the prepared root surfaces and was
firmly adapted to the recipient bed with finger pressure in order
to minimize the dead space. Flap margins were approximated using
independent sling absorbable sutures(5-0 polyglactin 910). A
superficial relieving incision was made approximately 7mm apical
to the marginal gingiva in order to release the tension at the
base of the flap. Two weeks following surgery, a vestibular incision
was made from 33 to 43 using diode LASER (3w power in
continuous mode). This procedure aided in prevention of muscle
reattachments in healing tissue during the remodelling period of
the CTG/CM. Periodontal dressing (coe-pak) was placed in order
to protect the surgical site.
Post operative instructions and home care
Patients were prescribed with Amoxicillin 500mg 8hrly and Paracetmol
500mg 8hrly for five days. Patients were advised not to
brush in the surgical area for 4 weeks post-surgically in order to
avoid trauma to the surgical site and prescribed to use chlorhexidine
mouthwash for 6 weeks. The periodontal dressing, sutures
were removed at the end of two weeks.
Healing was uneventful without any wound dehiscence at all the
treated sites. Patients were enrolled in a stringent post-operative
supportive care regimen and the clinical parameters were recorded
at the end of 1 year and at 3 years for retrospective analysis.
Statistical analysis
SPSS version 22.0 was used to analyze the data. Subject level statistical
analysis was carried out. Thirty of the 38 patients were
regularly monitored and examined for three years after surgery.
The statistical analysis was limited to the data of participants who
had completed a three-year follow-up. The descriptive parameters
were expressed in terms of mean and standard deviation. Kolmogorov
– Smirnov test and Shapiro – Wilks tests showed that
the current study data followed a parametric distribution. To com pare the mean values between groups independent t-test was used
and to compare the mean values between time points paired t-test
was used. Chi-Square analysis was used to compare proportions
between groups. Significance level was fixed as 5% (p < 0.05).
Results And Discussion
MMGF+CTG was used to treat 64 recession defects in 15 participants
with a mean age range of 39.53 ± 8.17yrs. MMGF+XCM
was used to treat 67 recession defects in 15 participants with a
mean age range of 40.20 ± 9.84yrs. Table 1 showed the mean
descriptive values of all the clinical parameters measured across
various time points. There was no statistical significant difference
between test and control subjects at baseline (p>0.05). At both
follow-up intervals, intergroup analysis revealed that control subjects
had a statistically significant reduction in gingival recession,
a higher percentage of root coverage, and a gain in clinical attachment
compared to test subjects. Further, significant improvement
in VD was noted in the control subjects at 3 years follow up
(p<0.05). Intra group analysis showed that both the interventions
resulted in significant improvement in all clinical parameters from
baseline to 1 and 3yrs time period (p < 0.001) (table 2)
The definitive goal of mucogingival therapy is not only aimed
at achieving root coverage, but also to gain a healthy and stable
mucogingival complex. Conventionally, management of advanced
recession defects associated with other mucogingival deformities
such as high frenal attachment and or shallow vestibular depth,
involves a two stage surgical protocol, where the initial procedure
targets to correct frenal adhesion/augment the vestibular depth
and keratinized tissue followed by root coverage. The MMGF
technique used in current study, aimed to deepen the vestibule
simultaneously augmenting the mucogingival complex. The vestibular
relieving incision neither exposed the deeper tissues nor
compromised the vascularity explaining the uncomplicated rapid
healing which occurred across all the subjects. The minimally invasive
laser assisted vestibular incision given during the early healing
period resulted in tension free remodeling of tissues which
aided in maintaining the deepened vestibule is in concordance
with study by Eftal et al 2014 [14].
The objectives of this retrospective study were primarily to assess
the changes in linear parameters such as RH, RC%, KT, and
VD. From baseline to 3 years, the MMGF + CTG group had a
significant reduction in mean RH of 1.76 ± 0.59mm, whereas
the MMGF+XCM patients had a significant mean variation in recession
height of 0.98 ± 0.43mm (p<0.05). However, intergroup
analysis revealed that the MMGF+CTG group had significantly
better outcomes than the test subjects at both 1 and 3 years.
(p<0.05).
In the current study, the mean root coverage percentage achieved
was 61.02±20.77%, 43.31±14.59% at 1 year and 67.10±22.90%,
35.51±16.14% at 3 years in control and test groups respectively.
There was a transient increase in root coverage percentage in the
control group from 1 to 3 years. This could be attributed to the
phenomenon of creeping attachment, described as postoperative migration of the gingival marginal tissue in a coronal direction,
covering partially or totally a previously denuded root, seen commonly
in narrow recession defects [15]. The mechanism of creeping
attachment could be attributed to the presence of aseptic inflammation
which favours an increase in the vascularization and
proliferation of viable cells [15].
Scientific reports investigating the outcomes of root coverage
procedures using CTG as augmentation material in miller’s class
III recession defects reported a mean RC% ranging from 73-
83% (Aroca), 78%. (Yaman),74% (Esteibar) [20-22] and 60-83%
(Moussa) [16-19]. In a recent systematic review by Fernandez et al
2021 comparing pre-twenty first century surgical techniques and
twenty - first century techniques in the management of Miller’s
class III gingival recession, CRC was achieved at 6 months on
half of the recessions (pre-twenty-frst: 57.60% vs. 21st: 51.11%),
which drastically reduced for twenty-frst century techniques at
the end of 12 months (pre-twenty-first: 63.82% vs. 21st: 32.87%)
[7].
Since, there were no clinical trials being done evaluating the efficacy
of fish derived collagen matrix in management of recession,
we couldn’t associate our outcomes with any other literature
reports. However, AlSarhan et al and Atieh et al analyzed 353 and
427 recession defects in their systematic reviews and suggested a
MRC% ofof 65.8% and 71 ± 21 to 94.32 ± 11.68%for xenogenic
collagen matrix in the management of class I and II gingival
recessions [20, 21].
The mean gain in KT was 1.74 ± 0.57mm and 1.44 ±0.64mm in
control and test subjects respectively at the end of 3 years. The gain
in KT was in line with the results obtained by Cardarapoli(CAF
+CTG,1.3 mm and CAF+CM, 1.2 mm) Paulo (MCAT+CTG,1.31
± 1.23 mm) and Sato(EMD +CTG, 1.5 mm) [23, 24]. A statistically
significant gain in mean vestibular depth of 1.27 ± 0.52 mm
was achieved in the CTG subjects over a mean gain of 0.76 ±
0.56 mm in the XCM subjects at the 3 year follow up. Only a few
study reports had reported the alterations of this parameter. In
the case series by Nicole et al in 2013, the authors evaluated the
use of a modified mucogingival flap with connective tissue graft in the management of class I and II mandibular recession defects
and they obtained an increase in VD of 0.9±0.5 mm which is in
concordance with our study [25].
Systematic review by Cairo and meta-analysis by Chambrone substantiate
the advantages of sub epithelial connective tissue grafting
in mucogingival surgeries [3, 4].
Due to limitations of autogenous graft harvesting, a non autologous
marine based xenogenic collagen matrix substitute had been
investigated. The rationale to use collagen matrix as a scaffold for
cell proliferation was based on its ability to enhance clot stability
and increase fibrin linkage. It is physiologically remodeled and
has a favorable effect on healing; thereby acting as a significant
barrier.
The XCM used in this study was being used as an adjunct to mucogingival
augmentation for the first time, it had good workable
characteristics, did not require any pre soaking and stabilization
sutures. At 1 year, the test subjects had a greater percentage of
root coverage than at 3 years, indicating the short term benefits
of MMGF+XCM. Thoma et al emphasized that inorder to establish
complete healing and remodeling the collagen matrices, scaffolds
should be able to remain for a longer duration [26]. Clinical
outcomes achieved with XCM could be further improved by way
of cross linking inorder to increase the resorption time thereby
making it a suitable prospective substitute for autogenous grafts.
Table 2. Mean variation of clinical parameters from baseline to 1 and 3-year time intervals among study groups.
Conclusion
It could be ascertained that the use of MMGF with CTG enabled
prolonged sustainment of the root coverage obtained along with
maintenance of keratinised tissue and vestibular depth in a long
term frame upto 3 years. Further studies are warranted with long
term follow up using collagen matrices in minimal recession defects
which may yield superior results and enhance the prospects
of using xenogenic collagen matrices in the field of mucogingival
surgery.
References
-
[1]. Dym H, Tagliareni JM. Surgical management of cosmetic mucogingival defects.
Dental Clinics of North America. 2012 Jan 31;56(1):267-79.
[2]. Stimmelmayr M, Allen EP, Gernet W, Edelhoff D, Beuer F, Schlee M, Iglhaut G. Treatment of Gingival Recession in the Anterior Mandible Using the Tunnel Technique and a Combination Epithelialized-Subepithelial Connective Tissue Graft--A Case Series. International Journal of Periodontics & Restorative Dentistry. 2011 Mar 1;31(2).
[3]. Cairo F, Pagliaro U, Nieri M. Treatment of gingival recession with coronally advanced flap procedures: a systematic review. Journal of clinical periodontology. 2008 Sep 1;35(s8):136-62.
[4]. Chambrone L, Pannuti CM, Tu YK, Chambrone LA. Evidence-based periodontal plastic surgery. II. An individual data meta-analysis for evaluating factors in achieving complete root coverage. Journal of periodontology. 2012 Apr;83(4):477-90.
[5]. Miller Jr PD. A classification of marginal tissue recession. The International journal of periodontics & restorative dentistry. 1985;5(2):8. [6]. Wennström JL. Mucogingival therapy. Annals of periodontology. 1996 Nov;1(1):671-701
[7]. Fernández-Jiménez A, García-De-La-Fuente AM, Estefanía-Fresco R, Marichalar-Mendia X, Aguirre-Urizar JM, Aguirre-Zorzano LA. Complete root coverage in the treatment of Miller class III or RT2 gingival recessions: a systematic review and meta-analysis. BMC oral health. 2021 Dec;21(1):1-8.
[8]. Lorenzo R, García V, Orsini M, Martin C, Sanz M. Clinical efficacy of a xenogeneic collagen matrix in augmenting keratinized mucosa around implants: a randomized controlled prospective clinical trial. Clinical Oral Implants Research. 2012 Mar 1;23(3):316-24.
[9]. Nisar N, Nilesh K, Parkar MI, Punde P. Extraction socket preservation using a collagen plug combined with platelet-rich plasma (PRP): A comparative clinico-radiographic study. Journal of Dental Research, Dental Clinics, Dental Prospects. 2020;14(2):139.
[10]. Ravi KS, Shashikiran ND, Choudhary P, Kulkarni V, Vanka A. Orthograde mineral trioxide aggregate (MTA) placement against an internal matrix of absorbable collagen matrix: outcome of a case series. Endodontic Practice Today. 2011 Dec 1;5(4).
[11]. Jaikailash, Kavitha. Simplified single step MTA apexification with collagen barrier and custom made GP condenser. Journal of Indian Dental Ass TN. 2012.
[12]. Mithra N.Hegde, Priyadarshini Hegde. Single step MTA apexification with collagen barrier– a case report american journal of oral medicine and radiology. 2015;2(2):89-92.
[13]. Marggraf E. A direct technique with a double lateral bridging flap for coverage of denuded root surface and gingiva extension. Journal of clinical periodontology. 1985 Jan 1;12(1):69-76.
[14]. Yilmaz E, Ozcelik O, Comert M, Ozturan S, Seydaoglu G, Teughels W, Haytac MC. Laser-assisted laterally positioned flap operation: a randomized controlled clinical trial. Photomedicine and laser surgery. 2014 Feb 1; 32(2): 67-74.
[15]. Matter, J., Cimasoni, G. Creeping after free gingival graft: A five year follow up study. J Periodontol, 1980.
[16]. Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi R, Etienne D. Treatment of class III multiple gingival recessions: a randomized-clinical trial. Journal of clinical periodontology. 2010 Jan 1;37(1):88-97.
[17]. Yaman D, Demirel K, Aksu S, Basegmez C. Treatment of Multiple Adjacent Miller Class III Gingival Recessions with a Modified Tunnel Technique: A Case Series. International Journal of Periodontics & Restorative Dentistry. 2015 Jul 1;35(4).
[18]. Esteibar JR, Zorzano LA, Cundín EE, Blanco JD, Medina JR. Complete root coverage of Miller Class III recessions. Int J Periodontics Restorative Dent. 2011 Jul 1;31:e1-7
[19]. Moussa, Ehab W.; Bissada, Nabil F. (2016). Comparative Outcomes of Class III Miller Gingival Recession Treatment Utilizing the Tunnel or CAF Approaches. A Case Report. Clinical Advances in Periodontics, (), 1–16. doi:10.1902/cap.2016.160023
[20]. AlSarhan MA, Al Jasser R, Tarish MA, AlHuzaimi AI, Alzoman H. Xenogeneic collagen matrix versus connective tissue graft for the treatment of multiple gingival recessions: A systematic review and meta-analysis. Clin Exp Dent Res. 2019;5(5):566-579. Published 2019 Jun 30. doi:10.1002/ cre2.210
[21]. Atieh MA, Alsabeeha N, Tawse-Smith A, Payne AG. Xenogeneic collagen matrix for periodontal plastic surgery procedures: A systematic review and meta-analysis. Journal of periodontal research. 2016 Aug;51(4):438-52. 24.
[22]. Cardaropoli D, Tamagnone L, Roffredo A, Gaveglio L. Treatment of gingival recession defects using coronally advanced flap with a porcine collagen matrix compared to coronally advanced flap with connective tissue graft: a randomized controlled clinical trial. Journal of periodontology. 2012 Mar;83(3):321-8
[23]. Carvalho PF, da Silva RC, Cury PR, Joly JC. Modified coronally advanced flap associated with a subepithelial connective tissue graft for the treatment of adjacent multiple gingival recessions. Journal of periodontology. 2006 Nov;77(11):1901-6.
[24]. Sato S, Yamada K, Kato T, Haryu K. Treatment of Miller Class III recessions with enamel matrix derivative (Emdogain) in combination with subepithelial connective tissue grafting. International Journal of Periodontics & Restorative Dentistry. 2006 Jan 1;26(1)
[25]. Bethaz N, Romano F, Ferrarotti F, Maria Mariani G, Aimetti M. A mucogingival technique for the treatment of multiple recession defects in the mandibular anterior region: a case series with a 2-year follow-up. International Journal of Periodontics & Restorative Dentistry. 2014 May 1;34(3).
[26]. Thoma DS, Jung RE, Schneider D, Cochran DL, Ender A, Jones AA, Görlach C, Uebersax L, Graf-Hausner U, Hämmerle CH. Soft tissue volume augmentation by the use of collagen-based matrices: a volumetric analysis. Journal of Clinical Periodontology. 2010 Jul 1;37(7):659-66.