Management of Compromised Esthetic Zone with Modified Bio-Col Procedure
Rajeev Arunachalam*, Vini Rajeev, Sivadas Ganapathy, Vaishnavi Vedam
Senior Lecturer, Faculty of Dentistry, Asian Institute of Medicine, Science and Technology (AIMST) University, Malaysia.
*Corresponding Author
Rajeev Arunachalam,
Senior Lecturer, Faculty of Dentistry, Asian Institute of Medicine, Science and Technology (AIMST) University, Malaysia.
Tel: + 60164055204
E-mail: rajeevarun80@gmail.com
Received: October 05, 2021; Accepted: October 22, 2021; Published: October 30, 2021
Citation: Rajeev Arunachalam, Vini Rajeev, Sivadas Ganapathy, Vaishnavi Vedam. Management of Compromised Esthetic Zone with Modified Bio-Col Procedure. Int J Dentistry Oral Sci. 2021;8(10):4876-4880. doi: dx.doi.org/10.19070/2377-8075-21000986
Copyright: Rajeev Arunachalam©2021. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Following extraction of tooth, a considerable change in alveolar ridge anatomy occurs pertaining to morphology and dimension in a short span of time. These variations can significantly affect future rehabilitation process if not planned. An implant placement may become more complicated if bone resorption is more. Tissue engineering aims to reestablish functional, healthy tissues and structures in order to supplant unhealthy, dying, or deceased tissues. Diverse tissue regenerative techniques have been established for rectifying bone defects with the intention of creating an efficient and appealingly agreeable pontic or implant restoration situates. A simple minimally invasive procedure immediately following tooth extraction known as Bio-Col alveolar ridge preservation technique decreases the necessity for reestablishing challenging ridge defects. This case represents a revised technique of preserving socket in periodontally compromised situation using a combination of platelet rich fibrin, collagen scaffold and bone graft followed by rehabilitation with implant for esthetic replacement. Clinically and radiographically efficacious restoration of the alveolar ridge, with the ability to receive functionally and esthetically acceptable implant site was demonstrated.The modification simplifies the technique without negotiating the esthetic outcome. This procedure is beneficial in maintaining alveolar bone and soft tissue architecture.
2.Introduction
3.Materials and Methods
3.Results
4.Discussion
5.Conclusion
5.References
Keywords
Atraumatic Extraction; Esthetics; Fixed Partial Denture; Implant; Osseointegration.
Introduction
Periodontally compromised tooth with hopeless prognosis may
institute therapeutic extractions. The functional and esthetic
replacement of the teeth being removed and their supporting
tissues should be taken into prior notice, when extractions are
planned. Fixed bridge options were the benchmark for esthetic
replacements previously. Increased awareness and widespread use
of dental implants have made preservation of both alveolar bone
and essential gingival contours possible for esthetic restoration.
Use of minimally invasive technique ensures an atraumatic extraction
which is the first possible step ensuring a better esthetics and
function. This holds true if an implant is planned for extraction
site. Adopting an appropriate technique enables the treatment in a
shorter time and with fewer surgical procedures thereby preserving
the alveolar ridge anatomy, aiding the prosthetic management.
Ridge preservation should be considered in strategically essential
sites to maintain the prospect of an implant preference for the
patient in the future.
The goal of the site-preservation technique is to minimize damage
of alveolar ridge contours secondary to osseous remodeling,
increase bone regeneration within the extraction socket, and prevent
soft tissue collapse associated with tooth loss. The bio-col
alveolar ridge preservation procedure takes the benefit of the
synergistic effect of merging surgical and prosthetic site- conservation
protocols. The surgical procedure makes sure the conservancy
of both hard and soft tissues at the period of tooth removal,
and it reduces or eradicates the bone resorption that normally
follows. The prosthetic protocol uses interim restorations to support
the soft tissues neighboring the extraction site, thereby averting
the ridge collapse during maturation. The usage of grafting
material in any stoichiometric form is suggested as it clues to reduced
resorption of alveolar crest. The advantage using an array
of regenerative materials like bone graft within a collagen scaffold
will give more structured bone with no signs of in growth other than bone. This may be related to collagen material functioning
as a barrier to the ingrowth of surrounding tissue that could have
impeded the process of bone regeneration. The original Bio-col
technique grosses the benefit of the above principle and recommends
atraumatic extraction without perforation of the socket
wall followed by condensation graft and collagen material [1].
The natural healing phenomenon after tooth removal involves resorption
and remodeling of the alveolar ridge, which is physiologically
detrimental plus certainly inevitable and can have negative
impact on implant placement [2, 3]. This holds true in maxillary
anterior region, where the vestibular wall can be damaged more
frequently during tooth removal due to prominent root position
which is generally accompanied by an extremely fine and fragile
buccal wall [4]. The maturation and mineralization of the recently
formed bone in the extraction socket can be hastened or enhanced
by ridge preservation. In areas where there is an osseous defect,
the predictability and outcome of the implant procedure is largely
determined by the shape of the defect. Pertaining to extraction
sites the osseous defects can be classified based on morphology as
favorable or unfavorable [5]. There is distinct treatment protocol
variability among above mentioned defects. In favorable sites additional
site preparation surgeries are not required during implant
placement whereas the unfavorable defects at aesthetic sites mandates
site- development procedures.
Creating a strong foundation for osseointegrated implants by preserving
the socket and alveolar ridge anatomy is the primary purpose
of surgical bone grafting techniques [6]. It is important for
dentist to decide at what time and where forthcoming implants
must be located. For the above an understanding of hard and
soft tissue alterations of post-extraction sockets and the form of
anatomy of the future implant site is needed. Not only osseointegration
but also an appealing restoration that is unwavering over
time is the current focus for implant therapy [7]. Preoperative
planning of various factors should be made and the scheduling
of implant placement post-extraction is crucial which influences
the aesthetic outcome [8].
This clinical report highlights the rehabilitation of maxillary anterior
tooth of a young male patient with a history of tooth loss
due to road traffic accident in a periodontally compromised tooth
using modified bio-col technique and subsequent prosthodontic
management with dental implant.
Case Presentation
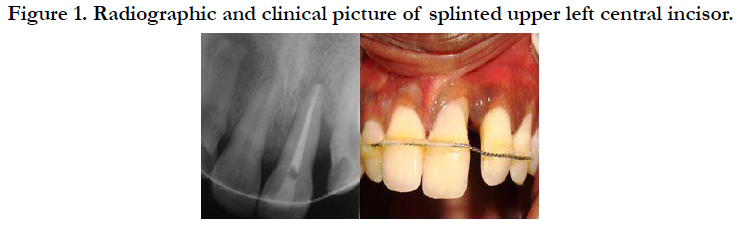
A 26 year old male patient was referred to prosthodontist with
a complaint of mobility of upper left central incisor following
a road traffic accident. Dental history was significant for recent
trauma to upper left central incisor in a road traffic accident but
the tooth had not been avulsed. There was no significant medical
history. Upon assessment and diagnosis of the traumatized
tooth, it was determined that the tooth showed grade II mobility
with supraeruption. Patient’s history revealed that prior to accident
the spacing was seen been two upper central incisors and
was gradually increasing with mild supraeruption in relation to
upper left central incisor. Radiographic assessment was done and
angular pattern of bone loss was seen in relation to distal aspect
of root extending more than half of root length (Figure 1). Since
the patient was seen on an emergency basis the traumatized tooth
had been splinted to the adjacent teeth using composite resin and
wire (Figure 1). The patient was subjected to complete scaling and
thorough root planning under LA and oral hygiene instructions
were given and was decided to be reviewed after 4 weeks to evaluate
the prognosis and definite management. Following 4 weeks,
evaluation was done and as the grade of mobility and supraeruption
worsened, the tooth was deemed hopeless and planned for
extraction. Restoration options included endosseous implant in
relation to upper left central incisor, fixed partial denture, or removable
partial denture (RPD). The patient voiced a strong need
to have the tooth replaced with implants. The patient was nonsmoker.
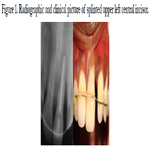
As the tooth had periodontal involvement atraumatic extraction
was planned and in order to maximize the amount of available
bone for implant placement, socket augmentation procedure was
decided where a variant from conventional Bio-Col technique was
suggested. As radiograph have revealed extensive bone loss pertaining
to the distal aspect a two stage/ late implant was decided.
The procedure was explained to the patient and the consent was
obtained for the same. Routine blood investigations were done.
Prior to surgery PRF preparation was done [9]. Once PRF preparation
is completed the patient is advised to rinse for 60 seconds
with a 0.12% chlorhexidine mouth wash. After local anesthesia was achieved, sulcular incision with a 15C surgical blade was made
circumferentially around upper left central incisor extending apically
to the osseous crest. Next the tooth was extracted atraumatically
utilizing a sharp Busar periosteal elevator and periotome
(Figure 2) followed by the removal of granulation tissue and inspection
of the socket.
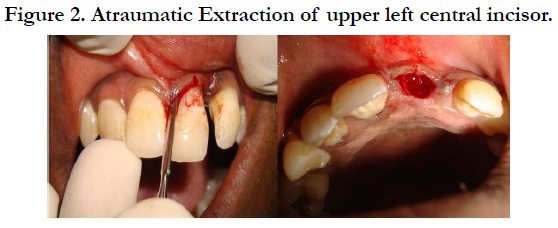
A Lucas surgical curette is used to perform thorough curettage
of the socket to remove any granulation tissue. Site was inspected
for socket wall defects and for evidence of spontaneous bleeding.
As spontaneous bleeding was not present, using small carbide
bur socket walls were perforated for fresh bleeding .Bio-Oss bone
graft was mixed with PRF over which the collagen dressing material
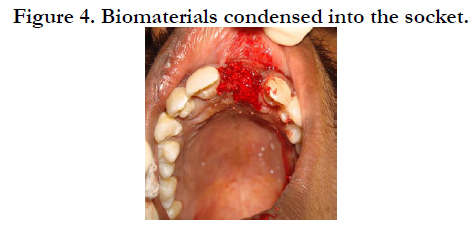
[collaplug] was dipped in so that is uniformly soaked (Figure
3).Then the biomaterials were packed into the socket (Figure 4)
with the finger pressure given over the facial gingiva to provide a
“solid stop” to condense the graft against. Socket is closed with
horizontal mattress sutures. Interim acrylic RPD with ovate pontic
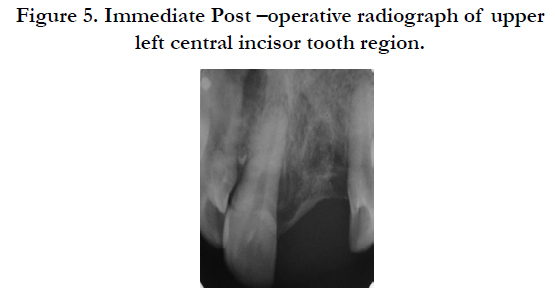
design was inserted. Immediate post-op IOPA radiograph was
made pertaining to upper left central incisor [Figure 5]. Post-surgery
instructions and removable partial denture instructions were
provided. After 4 weeks, clinical examination showed no significant
edema or infection and a satisfactory healing was noted.
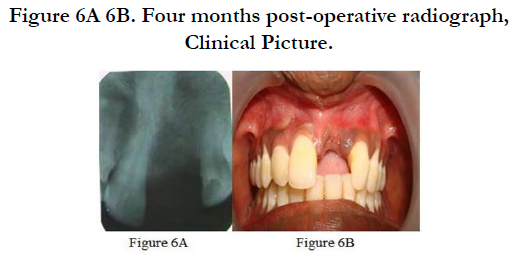
A thorough follow up of 2 and 4 months revealed increased
quantity of bone and good soft tissue contour (Figure 6A, 6B)
and hence the implant placement was planned. After evaluating
the clinical and radiographic findings, a tapered – self thread implant
of 13mm length and 4.5 mm diameter was considered ideal.
Scaling and polishing was executed 2 weeks preceding to surgery.
The prefabricated surgical stent was prepared to direct the implant
placement in correct angulation. After anesthetizing the
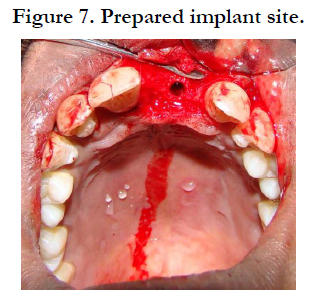
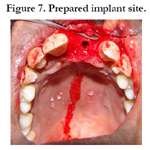
operating site via infiltration anesthesia, a full thickness (mucoperiosteal
flap) was raised placing a horizontal paracrestal incision
on the palatal part of the alveolar ridge. The flap was reflected
to the labial surface to uncover the underlying bone. Opening on
the occlusal area of the prefabricated surgical stent permitted the
surgical burs to be positioned and angled correctly in the implant
receiver site. The point of insertion on the bone was marked with
the aid of a round bur introduced through the occlusal opening
of the stent. This was followed by a the use of a 2mm spiral drill
at a bur speed of 800rpm to 1000 rpm with profuse irrigation
with normal saline. The depth stop of all instruments was placed
at 13 mm corresponding to the designated implant length. The
2mm spiral drill was taken to the predetermined depth followed
by a 3 mm spiral drill which enlarged the opening along the angulations
determined by the previous spiral drill. The recipient
site was prepared to the final diameter (4.5mm) by using manual
osteotome of decided diameter by gentle tapping with the surgical
mallet to successive increase in diameters. (Figure 7)
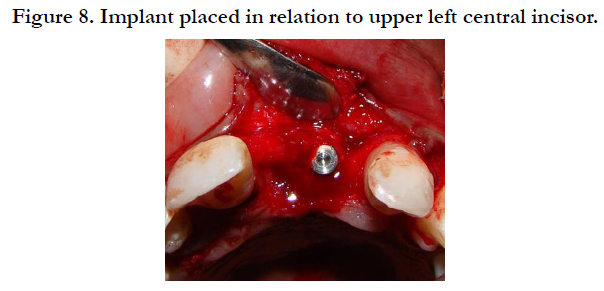
The implant was removed from the sterile packaging and placed
in the prepared osteotomy site using implant carrier and manually
screwed using torque wrench until the implant fitted snugly and
could be rotated into place. After implant insertion, the covering
screw was eased into position (Figure 8). The flap was closed over
the implant and sutured using interrupted sutures. A temporary
restoration was fabricated and used during the transitional period
i.e. period of healing. After a healing period of 4 months, a minimal
horizontal crestal incision just enough to expose the cover
screw was made. The titanium covering screw was detached and
swapped with a gingiva former which would allow the gingival
margin to form properly during the healing period and guarantee
an ideal emergence profile around the future crown abutment.
The gingiva former after 2 weeks was interchanged with a transfer
coping and impression was made with syringe material around
the transfer coping and a heavy body material was positioned in
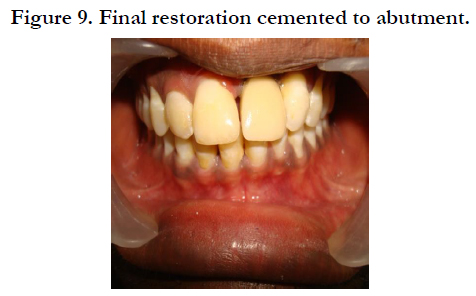
the tray for the rest of the dentition. The gingiva former was negotiated
back into the implant till the seating of the fabricated
crown was to be done. The implant analog was united with the
implant coping and secured with fastening screw. The abutment
screws were threaded into position in the implant after removing
the gingiva former and the final restoration was cemented to the
abutment (Figure 9) The patient was kept on systematic maintenance
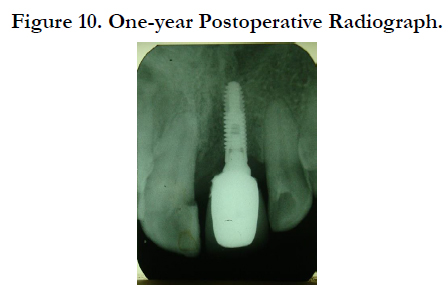
appointments during which the esthetics & functioning of
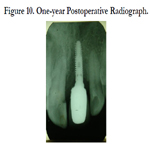
the restoration were found acceptable. A one-year postoperative
radiograph showed maintenance of adequate bone level and density
around the implant (Figure 10).
Discussion
The method offered in this article is a variant of the Bio-Col
Technique first published by Sclar (1999) which preserves as
much as possible the patient’s existing alveolar bone and gingival
contours during extraction [1]. Collagen dressing material serve
as a matrix for soft tissue healing at the site. Usage of collagen
wound dressing material was recommended not only to protect
the graft material as majority of it may be lost due to configuration
of the extraction socket but also to induce blood clot formation
and stabilize the wound [10, 11]. High biocompatibility and
hemostatic ability that can enhance platelet aggregation thereby
facilitating clot formation and wound stabilization makes collagen
dressing most preferable under these conditions [12]. Moreover
high chemotactic function of collagen for fibroblasts will promote
cell migration and accelerate primary wound coverage [13].
PRF concentrates have been extensively used as an addition to tissue
regeneration procedures [14, 15]. The histologic analysis done
on various studies showed a bone growth and a better trabecular
organization in areas treated with PRF and FDBA, compared to
control areas which where only treated with FDBA thereby decreasing
the healing time so much that implant could be already
placed 4 months after surgery [16]. The present case report demonstrated
good radiographic bone fill, better soft tissue contours
with faster healing time enabling the site to receive implant in a
shorter time span supporting the literature.
Periodontally compromised states which mandates therapeutic
extraction are one among the important clinical situations in
which delayed implant placement is indicated. Clinician should
recognize that considerable esthetic risk is associated with immediate
replacement under these conditions, each of which can
compromise the esthetic outcome secondary to soft recession
and early or late osseous remodeling. Bone resorption rate will
be more during the first 6 months following tooth extraction, unless
a socket augmentation procedure is performed or implant is
placed [17].
In general delayed implant placement is indicated when primary
implant stability is not feasible due to acute infection, periodontal
infection like abscess, defects of socket wall, bone defects like
dehiscence and fenestration in the esthetic areas which can compromise
the integrity of the buccal ridge crest. It is advisable to
reevaluate the site augmented by Bio-Col technique after three
months so that any site-development procedures if needed can
be noted after inspecting the alveolar ridge contours and any residual
esthetic defect that may have developed. Osseous defects at
sites can be classified as favorable or unfavorable based on their
morphology [5].
Regenerative potential of favorable defects are more as there is
sufficient interdental bone remaining at these site to provide vascularity
and cellularity to provide repair across the gap whereas in
defects with unfavorable morphology interdental bone volume is
less as the width of the wall defect is more than one third regenerative
potential to provide complete osseous repair is difficult even
when biomaterials such as grafts and barrier membranes are used.
In esthetic sites managed with Modified Bio-Col technique if
defects are favorable 4-6 months healing time is given prior to
implant placement whereas if defects are unfavorable the Bio-Col
technique serve as a space maintainer preventing the soft tissue
collapse and scarring of the site making it suitable for site development
procedures prior to implant placement.
Atraumatic preparation of the implant site determines quantity
of vital bone surrounding the implant [18]. The threshold temperature
level for bone survival is 47 degree C for 1 minute which
when exceeded can result in osteolysis; this may contribute to a
delay in osseointegration which explains detrimental effects of
motorized drills used during osteotomy preparation of implant
site [18-20]. Osteotomes are surgical instruments that can be used
effectively to enhance the placement of dental implants [21, 22].
These instruments generally cut, compress or deform bone to
assist in placement of implants. Deforming bone to accommodate
the placement of an implant takes advantage of a unique molecular property of bone collagen by breaking the polymeric
chains termed as sacrificial bonds between the collagen molecules.
If the bone deformation associated implant placement can be accomplished
without compromising blood supply healing of bone
will not be jeopardized [23]. This study have utilized the same
principle of using a combination of drill sequence along with osteotome
usage to minimize bone resorption and maximize healing.
Another reason is that these instruments gives the surgeon
a tactile sense of the bone quality when compacting the bone
, resulting in greater bone density, which is beneficial for initial
implant support. In contrast to rotary instruments they serve to
extend the apical floor of the osteotomy and have added advantage
of not generating heat during use [24]. Hence preparation
of an implant bed through the protocol followed in the current
study through combination of initial rotary instruments followed
by expansion- condensing osteotomes guarantees the maximum
preservation of the remaining bone, improvement of primary implant
stability, increased tactile sensitivity and major visibility and
control of the job.
Conclusion
Accomplishment of a fruitful esthetic outcome and good patient
satisfaction is a very challenging procedure, particularly when
dealing with the esthetic area. Placement of a dental implant in
the anterior esthetic zone is a technique-sensitive procedure with
little room for error. The described variant of the Bio-Col technique
in the study is a straightforward and reproducible procedure
that has a biologic basis for success to potentiate sites for delayed
implant placement. This standardized protocol allows successful
and predictable long-term successful functional outcomes regarding
alveolar bone regeneration and implant rehabilitation.
References
-
[1]. Sclar A. Ridge preservation for optimum esthetics and function. The Bio-Col
technique. Postgrad Dent. 1999;6(1):3-11.
[2]. Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, Nedic M. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. Journal of periodontology. 1998 Sep;69(9):1044-9.Pubmed PMID:9776033.
[3]. Aimetti M, Romano F, Griga FB, Godio L. Clinical and histologic healing of human extraction sockets filled with calcium sulfate. International Journal of Oral & Maxillofacial Implants. 2009 Oct 1;24(5). PubmedPMID: 19865631.
[4]. Van der Weijden F, Dell'Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. Journal of clinical periodontology. 2009 Dec;36(12):1048-58.
[5]. Sclar AG. The Bio-Col Technique. In: Soft Tissue and Esthetic Considerations in Implant Therapy. Carol Stream, IL: Quintessence Publishing Co., 2003:75-112.
[6]. Norton MR, Wilson J. Dental implants placed in extraction sites implanted with bioactive glass: human histology and clinical outcome. International Journal of Oral & Maxillofacial Implants. 2002 Mar 1;17(2).
[7]. Tonetti, MS, Hammerle, CH. European Workshop on Periodontology Group C. Advances in bone augmentation to enable dental implant placement: Consensus Report of the Sixth European Workshop on Periodontology. Journal of Clinical periodontology., 2008; 35(Suppl): 168–172. PubmedPMID: 18724849.
[8]. Chen, ST,Buser, D. Clinical and esthetic outcomes of implants placed in postextraction sites. The International Journal of Oral & Maxillofacial Implants., 2009 ;24(Suppl): 186–217. PubmedPMID:19885446.
[9]. Dohan DM, Choukroun J, Diss A, DohanSL, Dohan AJ, Mouhyi J, et al.Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral RadiolEndod., 2006; 101:e37-44. PubmedPMID:16504849.
[10]. Wang HL, Kiyonobu K, Neiva RF. Socket augmentation: rationale and technique. Implant Dentistry. 2004 Dec 1;13(4):286-96.
[11]. Gupta D, Gundannavar G, Chinni DD, Alampalli RV. Ridge Preservation done ImmediatelyfollowingExtraction using Bovine Bone Graft, Collagen Plugand Collagen Membrane. International Journal of Oral Implantology and Clinical Research. 2012 Jan 1;3(1):8-16.
[12]. Sabelman EE. Biology, biotechnology and biocompatibility of collagen. Biocompatibility of tissue analogs. 1985:21-66.
[13]. Postlethwaite AE, Seyer JM, Kang AH. Chemotactic attraction of human fibroblasts to type I, II, and III collagens and collagen-derived peptides. Proceedings of the National Academy of Sciences. 1978 Feb 1;75(2):871-5. [14]. Sakka S, Coulthard P. Bone quality: a reality for the process of osseointegration. Implant dentistry. 2009 Dec 1;18(6):480-5. Pubmed PMID: 20009601.
[15]. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2006 Mar 1;101(3):e45-50.
[16]. Inchingolo F, Tatullo M, Marrelli M, Inchingolo AM, Scacco S, Inchingolo AD, et al. Trial with Platelet-Rich Fibrin and Bio-Oss used as grafting materials in the treatment of the severe maxillar bone atrophy: clinical and radiological evaluations. Eur Rev Med Pharmacol Sci. 2010 Dec 1;14(12):1075- 84.
[17]. Schwartz-Arad D, Chaushu G. The ways and wherefores of immediate placement of implants into fresh extraction sites: a literature review. Journal of periodontology. 1997 Oct;68(10):915-23.
[18]. Iyer S, Weiss C, Mehta A. Effects of drill speed on heat production and the rate and quality of bone formation in dental implant osteotomies. Part I: Relationship between drill speed and heat production. Int J Prosthodont. 1997; 10:411–414. Pubmed PMID:9495159.
[19]. Iyer S, Weiss C, Mehta A. Effects of drill speed on heat production and the rate and quality of bone formation in dental implant osteotomies. Part II: Relationship between drill speed and healing. Int J Prosthodont., 1997; 10:536–540. Pubmed PMID:9495174.
[20]. Tehemar S. Factors affecting heat generation during implant site preparation: a review of biologic observations and future considerations. Int J Oral MaxillofacImplants., 1999; 14:127–136. Pubmed PMID:10074763.
[21]. Garg AK. The use of osteotomes: a viable alternative to traditional drilling. Dent Implantol Update. 2002; 13:33-40. Pubmed PMID:12060956.
[22]. Saadoun AP, Le Gall MG.Implant site preparation with osteotomes: principles and clinical application. Pract Periodontics Aesthet Dent. Jun-Jul 1996;8(5):453-63.Pubmed PMID:9028267.
[23]. Yin XM, Dai JX, Wang XH, Xu DC, Zhong SZ. Observation of blood supplies system to mandible in transparent specimen. Shanghai kouqiangyixue= Shanghai journal of stomatology. 2003 Aug 1;12(4):266-8.
[24]. Hahn J. Clinical uses of osteotomes. Journal of Oral Implantology. 1999 Jan;25(1):23-9.