Buccal Pad Of Fat - The Nature’s Gift For Oral Reconstruction
Subhashini Ramasubbu1*, Shivangi Gaur1, Abdul Wahab PU2, Madhulaxmi Marimuthu2
1 Post Graduate Student, Department of Oral and Maxillofacial Surgery, Saveetha Dental College And Hospitals, Saveetha Institute of Medical And
Technical Sciences(SIMATS), Saveetha University, Chennai, India.
2 Professor, Saveetha Dental College And Hospitals, Saveetha Institute of Medical And Technical Sciences(SIMATS), Saveetha University, Chennai, India.
*Corresponding Author
Dr. Subhashini Ramasubbu,
Post Graduate Student, Department of Oral and Maxillofacial Surgery, Saveetha Dental College And Hospitals, Saveetha Institute of Medical And Technical Sciences (SIMATS), Saveetha University, Chennai, India.
Tel: 9999286618
E-mail: meetsubha07@gmail.com
Received: July 29, 2020; Accepted: September 11, 2020; Published: September 30, 2020
Citation:Subhashini Ramasubbu, Shivangi Gaur, Abdul Wahab PU, Madhulaxmi Marimuthu. Buccal Pad Of Fat- The Nature’s Gift For Oral Reconstruction. Int J Dentistry Oral Sci. 2020;7(9):824-827. doi: dx.doi.org/10.19070/2377-8075-20000162
Copyright: Subhashini Ramasubbu©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The buccal pad of fat was initially believed to be an anatomic structure without any function, and was even considered to be a surgical nuisance. However with time, the buccal pad of fat has been used for various intraoral reconstructions. The buccal fat pad flap (BFP) is a simple and reliable flap because of its rich blood supply and location. It needs minimal dissection and can be mobilised easily. Good rate of epithelization and low failure rate makes it more favourable for oral reconstruction. The surgical procedure is simple and has shown very good results. Buccal pad of fat can be used for various surgeries like OAF closure, OSMF, Cleft Palate, Palatal Fistula, TMJ Surgery, Closure of small defects, Biological membrane for covering bone grafts. In this study we focused the clinical application of Buccal Pad of Fat in Oral and Maxillofacial Surgery.
2.Introduction
3.Anatomy
4.Case 1
5.Case 2
6.Case 3
7.Case 4
8.Discussion
9.Conclusion
10.References
Keywords
Buccal Pad of Fat; Buccal Pad Fat; Oral Reconstruction.
Introduction
The buccal pad of fat is the fat tissue that is located in profound
facial spaces. It lies behind zygomatic arch and it has four processes.
They are buccal process, pterygoid process, the superficial
process and the deep temporal process [1]. Pterygopalatie process
which stays in pterygopalatine fossa was found by Chinese scientists.
The volume may change throughout life.
The average weight of each buccal fat pad was found to be 9.3 g,
and its average volume was 9.6 ml [2, 3]. They stated that it serves
to line the masticatory space, separating the masticatory muscles
from each other and from the mandibular ramus and the zygoma.
This volume could be used to repair a defect measuring 4 x 4 x
3 cm in Maxilla & 7 x 5 x 2 cm. in mandible. Buccal pad of fat
chiefly owes its blood supply primarily to the small venules and
arterioles situated in the base, therefore both excessive manipulation
at the base and the rupture of surrounding vascular capsule
results in free fat transfer rather than vascular grafting.
Buccal Pad Of Fat is used in various Maxillofacial Surgeries [4]. It
has physiological functions which include filling deep tissue space,
and acts like a cushion for some structures from outer forces. It
also serves as a versatile flap in some reconstructive procedures.
The application of buccal pad of fat has increased rapidly in recent
years. It has been used in different kinds of surgeries. Now
the scientists have been working on regenerative properties of
buccal pad of fat [5].
With a rich case bank established over 3 decades we have been
able to publish extensively in our domain [6-16]. Based on this
inspiration we aim to present the following case series to highlight
the excellent properties of buccal pad of fat as a scaffold and
autogenous dressing in healing of intraoral defects like Oroantral
Fistula, after excision of a lesion in oral cavity, in the treatment of
OSMF and in Cleft Palate surgery.
Anatomy
Buccal pad of fat protrudes at the anterior border of the masseter
muscle and extends to the parotid duct, where it rests on the
buccopharyngeal fascia, which covers the buccinator muscle [1].
The main body is positioned along the posterior maxilla and it is
covered with a thin capsule. The parotid duct pierces the buccinator
at the anterior border of the buccal fat pad. The buccal fat
pad has abundant blood supplies from the maxillary artery and
the superficial and deep temporal artery. There are rich capillary
networks within the capsules that cover the fat pad. Arterioles
enter the capsule from several directions and break up into capillary
plexuses. Most of the blood from the fat pad drains into the
facial vein [17].
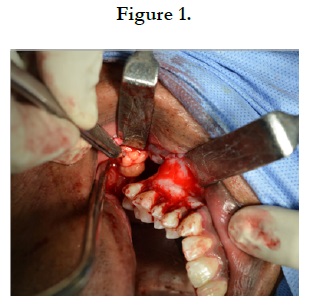
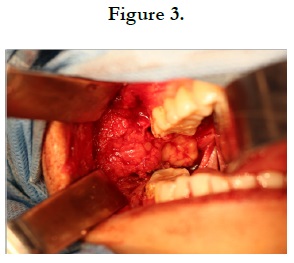
A 35 year old male patient came to the Department of Oral and
Maxillofacial Surgery with a chief complaint of Right hemifacial
pain and discharge from non healed orifice after extraction of
right upper third molar 6 months before. On examination, there
was a 5-6mm fistula which communicates the left maxillary sinus.
No pus or inflammation seen. Diagnosis was made as oroantral
Fistula. The treatment plan was to close the fistula using a buccal
pad of fat. Vestibular incision was given in relation to the right
upper first molar till third molar region. Full thickness muco periosteal
flap elevated and Fistula was noted. Buccal pad of fat was
harvested (Figure 1) and it was used to close the fistula. Simple
interrupted sutures were placed to secure the fat pad.
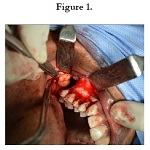
A 10 months old baby presented with Cleft Palate to the Department
of Oral and Maxillofacial Surgery for the primary repair.
Using Bardach’s technique, primary palatoplasty was done. Buccal
pad of fat can be used as a packing material to cover the raw
bone (Figure 2). Using blunt dissection, a buccal pad of fat was
harvested and then placed toward the area of the defect and sutured
with light pressure to the edge of the flap and left open
for the epithelialization. Satisfactory healing was noted postoperatively.
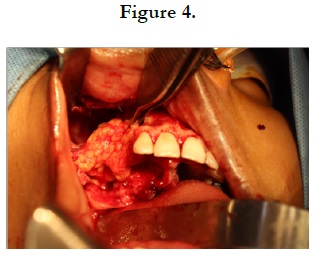
Different surgical procedures described in the literature claim different
success rates. The use of a Buccal pad of fat as a grafting
material is relatively good. The fibrous bands were detected
by digital palpation. Horizontal incision given along the occlusal
plane in buccal mucosa. Incision extends anteriorly from the corner
of the mouth till pterygomandibular raphe posteriorly. Using
fingers, bands were released. The mouth was then forced to
open with the mouth gag to an acceptable range of approximately
40 mm. A small amount of the lesions were excised and sent for
biopsy. The buccal pad of fat was harvested from the defect, that
is posterior to zygomatic buttress. After blunt dissection, buccal
pad of fat was gently mobilised until the required amount was
obtained to cover the defect. It should be covered without tension
(Figure 3). This can be done by gently pulling it using small artery
forceps. This pedicled fat pad was used to cover the areas. And
secured by placing horizontal mattress sutures using 3-0 Vicryl.
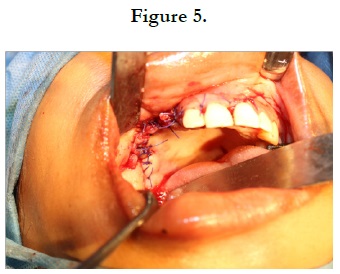
A 29 year old female patient reported to the Department of Oral
and Maxillofacial Surgery with a history of painless gradually progressive
swelling in the right side of the face for the past 3 years.
It was slow growing, no pain associated with it. On examination
it was diffuse, non-tender, bony hard swelling of approximately
5x6 cm extending from upper right canine till right upper molar.
Under general anesthesia, excision of the lesion done and sent for
histopathological examination. Buccal pad of fat was harvested
and used to cover the defect (Figure 4,5).
Discussion
The anatomy of the buccal pad of fat is complex. A detailed review
of anatomy was described by [18]. It has a main body and
four processes. The main body lies above the parotid duct on the
anterior border of the masseter muscle and extends deeply to lie
on the posterior maxilla and forward along the buccal vestibule.
The buccal extension is superficial and enters the cheek below
the parotid duct. It descends to the mandibular retromolar region
and overlies the buccinator muscle.
The pterygoid extension of the fat pad passes down and back to
lie on the lateral surfaces of the pterygoid plates. Its temporal extension
passes upwards below the zygomatic arch, and comprises
a deep and a superficial portion. The deep part lies directly on
the temporalis muscle and its tendon, separating the temporalis
muscle from the zygomatic arch. The blood supply of the BFP
is from three sources: the maxillary artery (buccal and deep temporal
branches), the superficial temporal artery (transverse facial
branch), and the facial artery (small branches). Once the fascial
envelope of the BFP is opened, spontaneous fat pad herniation
into the mouth occurs [2, 18].
[19] was the first surgeon to report the use of the buccal fat pad
as a pedicled graft for the closure of oro-antral and oronasal communications:
a split-thickness skin graft was used to line the oral
side of the fat pad [19, 20]. reported the use of the buccal fat pad
as a free graft for reconstruction of defects within the oral cavity
[18]. have shown that the buccal fat pad need not be covered by a
skin graft when brought into the mouth because of its quick epithelization
within 3 weeks. They have reported that the superficial
layer of fat tissue is replaced by granulation tissue and is finally
covered by stratified squamous epithelium.
[21] reported successful results with the use of the BFP in reconstruction
of both palatal and cheek defects. It can also be used
in medicine related osteoradionecrosis of the jaws (MRONJ) reported by [21-23] successfully reported the use of buccal pad
of fat in oroantral communication [24]. reported that the buccal
pad of fat was not affected by postoperative radiation therapy in
cancer patients.
[25] reported that this flap has significant potential to function
as an added vascularized tissue layer in cleft palate repair. Advantages
of using buccal pad of fat include it provides vascular
coverage to the denuded bone, it lacks scarring effect, serves as
a bed for secondary granulation, it obliterates dead space at the
alveolar defect.
[26-28] and various other authors reported the use of buccal pad
of fat in the treatment of OSMF [29-31]. reported that buccal pad
of fat provided better results compared to naso labial flap in the
treatment of OSMF.
Conclusion
From this study, We conclude that the buccal pad of fat is rapidly
healing, less invasive, easy to harvest & manipulate and also acts as
a reconstructive material which is free from significant postoperative
complications.
References
- Tostevin PM, Ellis H. The buccal pad of fat: a review. Clin Anat. 1995;8(6):403-6. Pubmed PMID: 8713160.
- Kumar R. Buccal fat pad graft in oral and maxillofacial surgery-A review. Asian Pacific Journal of Health Sciences. 2018 Dec 30;5(4):1-0.
- Arce K. Buccal Fat Pad in Maxillary Reconstruction [Internet]. Atlas of the Oral and Maxillofacial Surgery Clinics. 2007;15: 23–32. Available from: http://dx.doi.org/10.1016/j.cxom.2006.11.003
- Yousuf S, Tubbs RS, Wartmann CT, Kapos T, Cohen-Gadol AA, Loukas M. A review of the gross anatomy, functions, pathology, and clinical uses of the buccal fat pad. SurgRadiol Anat. 2010 Jun;32(5):427–36.PubmedPMID: 19937328.
- Salehi-Nik N, Rezai Rad M, Kheiri L, Nazeman P, Nadjmi N, Khojasteh A. Buccal Fat Pad as a Potential Source of Stem Cells for Bone Regeneration: A Literature Review. Stem Cells Int. 2017 Jul 5;2017:8354640.PubmedPMID: 28757880.
- Senthil Kumar MS, Ramani P, Rajendran V, Lakshminarayanan P. Inflammatory pseudotumour of the maxillary sinus: clinicopathological report. Oral Surg. 2019 Aug 10;12(3):255–9.
- Wahab PUA, Madhulaxmi M, Senthilnathan P, Muthusekhar MR, Vohra Y, Abhinav RP. Scalpel Versus Diathermy in Wound Healing After Mucosal Incisions: A Split-Mouth Study. J Oral Maxillofac Surg. 2018 Jun;76(6):1160– 4.PubmedPMID: 29406253.
- J PC, Marimuthu T, C K, Devadoss P, Kumar SM. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin Implant Dent Relat Res. 2018 Aug;20(4):531-4.Pubmed PMID: 29624863.
- Eapen BV, Baig MF, Avinash S. An Assessment of the Incidence of Prolonged Postoperative Bleeding After Dental Extraction Among Patients on Uninterrupted Low Dose Aspirin Therapy and to Evaluate the Need to Stop Such Medication Prior to Dental Extractions. J Maxillofac Oral Surg. 2017 Mar;16(1):48–52.PubmedPMID: 28286384.
- Marimuthu M, Andiappan M, Wahab A, Muthusekhar MR, Balakrishnan A, Shanmugam S. Canonical Wnt pathway gene expression and their clinical correlation in oral squamous cell carcinoma. Indian J Dent Res. 2018 May;29(3):291–7.PubmedPMID: 29900911.
- Jain M, Nazar N. Comparative Evaluation of the Efficacy of Intraligamentary and Supraperiosteal Injections in the Extraction of Maxillary Teeth: A Randomized Controlled Clinical Trial. J Contemp Dent Pract. 2018 Sep;19(9):1117–21.PubmedPMID: 30287714.
- Abhinav RP, Selvarasu K, Maheswari GU, Taltia AA. The Patterns and Etiology of Maxillofacial Trauma in South India. Ann Maxillofac Surg. 2019 Jan;9(1):114–7.PubmedPMID: 31293938.
- Sweta VR, Abhinav RP, Ramesh A. Role of Virtual Reality in Pain Perception of Patients Following the Administration of Local Anesthesia. Ann Maxillofac Surg. 2019 Jan;9(1):110-3. Pubmed PMID: 31293937.
- Abdul Wahab PU, Senthil Nathan P, Madhulaxmi M, Muthusekhar MR, Loong SC, Abhinav RP. Risk Factors for Post-operative Infection Following Single Piece Osteotomy. J Maxillofac Oral Surg. 2017 Sep;16(3):328–32. Pubmed PMID: 28717291.
- Ramadorai A, Ravi P, Narayanan V. RhinocerebralMucormycosis: A Prospective Analysis of an Effective Treatment Protocol. Ann Maxillofac Surg. 2019 Jan;9(1):192–6.PubmedPMID: 31293952.
- Patil SB, Durairaj D, Suresh Kumar G, Karthikeyan D, Pradeep D. Comparison of Extended Nasolabial Flap VersusBuccal Fat Pad Graft in the Surgical Management of Oral Submucous Fibrosis: A Prospective Pilot Study. J Maxillofac Oral Surg. 2017 Sep;16(3):312–21.Pubmed PMID: 28717289.
- Kim M-K, Han W, Kim S-G. The use of the buccal fat pad flap for oral reconstruction [Internet]. Maxillofacial Plastic and Reconstructive Surgery. 2017;39. Available from: http://dx.doi.org/10.1186/s40902-017-0105-5
- Tideman H, Bosanquet A, Scott J. Use of the buccal fat pad as a pedicled graft. J Oral Maxillofac Surg. 1986 Jun;44(6):435–40.PubmedPMID: 3457926.
- Egyedi P. Utilization of the buccal fat pad for closure of oro-antral and/or oro-nasal communications. J Maxillofac Surg. 1977 Nov;5(4):241–4. PubmedPMID: 338848.
- Neder A. Use of buccal fat pad for grafts. Oral Surg Oral Med Oral Pathol. 1983 Apr; 55(4):349–50. Pubmed PMID: 6574411.
- Stuzin JM, Wagstrom L, Kawamoto HK, Baker TJ, Anthony Wolfe S. The Anatomy and Clinical Applications of the Buccal Fat Pad [Internet]. Plastic and Reconstructive Surgery. 1990; 85: 29–37. Available from: http://dx.doi. org/10.1097/00006534-199001000-00006
- Rotaru H, Kim M-K, Kim S-G, Park Y-W. Pedicled Buccal Fat Pad Flap as a Reliable Surgical Strategy for the Treatment of Medication-Related Osteonecrosis of the Jaw [Internet]. Journal of Oral and Maxillofacial Surgery. 2015;73: 437-42. Available from: http://dx.doi.org/10.1016/j. joms.2014.09.023
- De Biasi M, Maglione M, Angerame D. The effectiveness of surgical management of oroantral communications: a systematic review of the literature. Eur J Oral Implantol. 2014 Winter;7(4):347–57.PubmedPMID: 25422823.
- Kim Y-K, Yun P-Y, Oh J-S, Kim S-G. Prognosis of closure of large sinus membrane perforations using pedicledbuccal fat pads and a resorbable collagen membrane: case series study. J Korean Assoc Oral Maxillofac Surg. 2014 Aug;40(4):188–94.Pubmed PMID: 25247149.
- Ladani P, Sailer H. Application of buccal fat pad for lining of lateral defect in cleft palate repair and review of literature [Internet]. Journal of Cleft Lip Palate and Craniofacial Anomalies. 2016;3: 63. Available from: http://dx.doi. org/10.4103/2348-2125.187507
- Mehrotra D, Pradhan R, Gupta S. Retrospective comparison of surgical treatment modalities in 100 patients with oral submucous fibrosis [Internet]. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2009;107: e1–10. Available from: http://dx.doi.org/10.1016/j.tripleo.2008.12.012
- Saravanan K, Narayanan V. The use of buccal fat pad in the treatment of oral submucous fibrosis: a newer method. Int J Dent. 2012 May 15;2012:935135. PubmedPMID: 22666254.
- Ebenezer V, Balakrishnan B, Prakash D, Julius A. Versatality of Buccal Pad Fat Grafts in Surgical Treatment of Oral Submucous Fibrosis [Internet]. Biosciences Biotechnology Research Asia. 2013;10: 465–9. Available from: http://dx.doi.org/10.13005/bbra/1154
- Vadepally AK. “A Comparative Clinical Evaluation of the Buccal Fat Pad and Extended Nasolabial Flap in the Reconstruction of the Surgical Defect in Oral Submucous Fibrosis Patients”: A Commentary [Internet]. Journal of Oral and Maxillofacial Surgery. 2018;76:1833.
- Agrawal D, Pathak R, Newaskar V, Idrees F, Waskle R. A Comparative Clinical Evaluation of the Buccal Fat Pad and Extended Nasolabial Flap in the Reconstruction of the Surgical Defect in Oral Submucous Fibrosis Patients [Internet]. Journal of Oral and Maxillofacial Surgery. 2018;76: 676.e1–676. e5. Available from: http://dx.doi.org/10.1016/j.joms.2017.11.013
- Pardeshi P, Padhye M, Mandlik G, Mehta P, Vij K, Madiwale G, et al. Clinical evaluation of nasolabial flap & buccal fat pad graft for surgical treatment of oral submucous fibrosis – a randomized clinical trial on 50 patients in Indian population [Internet]. International Journal of Oral and Maxillofacial Surgery. 2015;44: e121–2. Available from: http://dx.doi.org/10.1016/j. ijom.2015.08.733