Interproximal Contact Area and Width: Relationship to Periodontal Parameters
Normah Yacob1, Raja Azman Awang2*, Mohd Zulkarnain Sinor2
1 Klinik Pergigian Jalan Gambut, Ministry of Heath, Malaysia.
2 School of Dental Sciences, Health Campus, Universiti Sains Malaysia, 16150 Kubang Kerian, Kelantan, Malaysia.
*Corresponding Author
Raja Azman Awang,
School of Dental Sciences, Health Campus, Universiti Sains Malaysia, 16150 Kubang Kerian, Kelantan, Malaysia.
Tel: +60179700316
E-mail: rjazman@usm.my
Received: August 22, 2020; Accepted: September 16, 2020; Published: September 23, 2020
Citation:Normah Yacob, Raja Azman Awang, Mohd Zulkarnain Sinor. Interproximal Contact Area and Width: Relationship to Periodontal Parameters. Int J Dentistry Oral Sci. 2020;7(9):804-808. doi: dx.doi.org/10.19070/2377-8075-20000158
Copyright: Raja Azman Awang©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: This study focuses on investigating the influence of the interproximal contact area and width on periodontal
parameters.
Materials and Methods: A total of 30 periodontitis subjects were involved in the study, and 661 teeth were selected for
analysis. Periodontal parameters such as plaque score, gingiva score, clinical probing depth and radiographic bone level were
recorded for each tooth. Upper and lower impressions were taken for construction of study models which were used for the
measurement of interproximal contact area and width. simple linear regression (SLR) and multiple linear regressions (MLR)
analysis were used to evaluate the relationship between periodontal parameters and interproximal dimension.
Results: The SLR analyses consistently showed that the interproximal contact area and width were both significantly related
with plaque score, gingiva score and bone level, and MLR analyses confirmed that both the interproximal contact area and
width were significant predictors for each plaque score, gingiva score and bone level model.
Conclusion: Within the limitation of the study, we can conclude that the interproximal contact area and width have a significant
relationship with the presence of dental biofilm, gingival bleeding and bone level in the subjects susceptible to periodontal
disease.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.Conclusion
7.Acknowledgement
8.References
Keywords
Periodontitis; Periodontal Disease; Gingivitis; Interdental Papilla; Periodontal Index; Dental Plaque Index; Periodontal Pocket.
Introduction
The periodontal disease initiation and progression is mainly influenced
by the shifts and stability of dental biofilm community
[1]. However, not all patients with equal exposure to dental biofilm
community are susceptible to the disease. Furthermore, it has
been shown that in patients who were susceptible to periodontitis,
not all of their teeth were equally affected by the disease [2]. Studies
have demonstrated that the retentiveness, maturity and composition
of dental biofilm are highly variable in each colonised
tooth, which eventually alters the periodontium health [3]. These
variabilities were found to be associated with local factors such
as oral hygiene, tooth malposition, tooth anatomy and gingival
contours [4, 5].
It is perceived that periodontitis onset and progression occur
more frequently at the interproximal surface [6]. The dimension
of the interproximal area appears to play some roles in the establishment
of the periodontal disease. This dimension is determined
by an area of interproximal contact, a horizontal distance between
neighbouring teeth and vertical distance from the alveolar bone
crest [7], which is occupied by interdental papilla. The papilla is an
essential biological barrier that protects the periodontal structure,
and also acts as a physical barrier against food impaction. The imperfection
in shape and size of the interproximal dimension may
lead to problems in maintaining the integrity of the interproximal
area, which could lead to dental biofilm and later on periodontal
disease. However, to the best of our knowledge, there is limited
study, if any, on the relationship between the interproximal dimension
and periodontal variables.
Most of the clinical studies to date investigate the inter-subject relationship between dental biofilm retentive factors and periodontal
health, where subjects are simply grouped into cohorts
of health and disease. This is quite problematic as the individual
heterogeneity is not considered in the analysis [8]. Therefore,
intra-subject studies investigating periodontal health in the same
patient are invaluable [9]. Unfortunately, studies that use this approach
are lacking, and no studies to date have investigated the
relationship between the plaque retentive factors and periodontal
disease using this method.
In clinical settings, understanding the relationship between local
factors such as interproximal dimension and periodontal disease
is essential in communication between clinician and patient about
oral health education and treatment plan. Personalised oral hygiene
regimen can be formulated and proposed if it is proven
that these local factors do have an impact on disease progression.
It is generally agreed that periodontitis can be prevented, easily
diagnosed and successfully controlled if appropriate prevention,
diagnosis and treatment are applied [10]. Periodontal diagnosis
should include a thorough assessment of possible risk factors
to promote early detection of disease and providing the earliest
treatment possible. This study focuses on investigating the influence
of interproximal contact area and width on the periodontal
parameters including plaque score, gingiva score, clinical probing
depth and bone level.
Materials and Methods
A total of 17 men and 13 women were involved in the study, and
661 teeth were selected for analysis. The subjects were periodontitis
patient with basic periodontal examination (BPE) score of
at least 3 or 4 at one of the sextant and had not lost more than 4
teeth. All subjects did not receive periodontal therapy within the
last six months and had no underlying medical problems. Written
informed consent was obtained from all subjects after the study
had been explained. The study was approved by the Human Research
Ethics Committee (JEPeM) of Universiti Sains Malaysia
(USM/JEPeM/16110483).
All teeth, except wisdom teeth, were subjected to evaluation of
clinical and radiographic periodontal parameters, which include
plaque score, gingiva score, clinical probing depth and radiographic
bone level. An impression of the upper and lower jaw was
then taken using alginate impression material (Kromopan, Lascod
S.P.A. Lab., Italy). Dental models were constructed using type III
dental stone, Pro - Solid® (Saint-Gobain Formula, Germany),
which were later used for measurement of the interproximal contact area and width. Prior to the start of actual measurement, a
calibration session was held to enumerate intra-examiner reliability
for measurement of periodontal parameters. In all analyses,
the percent agreement and kappa score were between 90 to 100%
and 0.80 to 1.00, respectively.
The plaque score was assessed using O'Leary plaque index [11],
and the gingiva score was assessed using Ainamo's Gingival Bleeding
Index [12]. Four surfaces were evaluated for each tooth, which
was mesial, distal, facial and lingual/palatal. The tooth plaque and
gingival score were either 0, 0.25, 0.5, 0.75 or 1, based on the number
of a surface with plaque or gingival bleeding.
Clinical probing depth (CPD) was recorded at six sites of a tooth:
mesiobuccal, distobuccal, mesiolingual, distolingual, midlingual
and midbuccal, and the average CPD was the tooth's pocket
depth score. Furthermore, the dental panoramic tomography
(DPT) image of each subject was used for the measurement of
a radiographic bone loss, which is a distance between the cementoenamel
junction and bone crest, using the Image J software
(National Institutes of Health, University of Wisconsin). The demarcation
between a more radiodense enamel and less radiodense
root cementum in the cervical region of teeth in the radiograph
was marked as the cementoenamel junction [13].
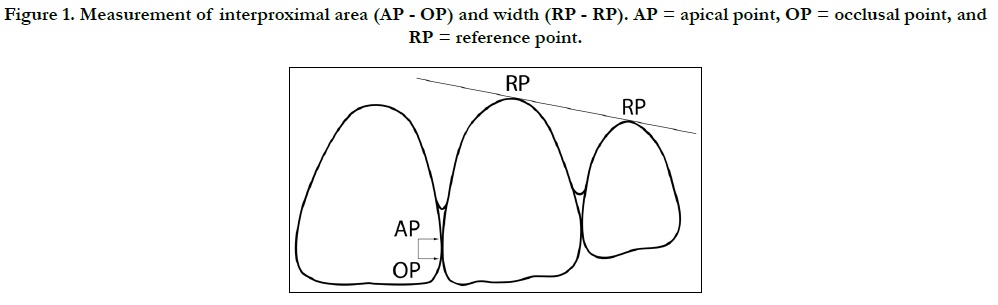
The interproximal contact area is the zone in which two adjacent
teeth meet (Foulger et al., 2010). It was measured as a distance in
millimetres between the apical point (AP) and the occlusal point
(OP) of the contact area, using a digital calliper (Figure 1). The
AP and OP were references for the interdental papilla tip and
initiation of the interdental occlusal embrasure, respectively [14].
For the measurement of interproximal width, gingival zenith,
the most apical part of gingiva scallop was marked as a reference
point (RP). The interproximal width was measured as the
horizontal distance between the RP of two adjacent teeth. The
interproximal width values were assigned to the tooth on the mesial
[15].
Figure 1. Measurement of interproximal area (AP - OP) and width (RP - RP). AP = apical point, OP = occlusal point, and RP = reference point.
Statistical analyses were carried out using IBM SPSS (Statistical
Package for the Social Sciences) Version 24.0. The influence of
the interproximal contact area and width on periodontal parameters were analysed using simple linear regression (SLR) and stepwise
multiple linear regressions (MLR) analysis. The unmeasurable
surface on the dental model and radiograph was reported as
a missing value. Significant level was set at p = 0.05.
Results
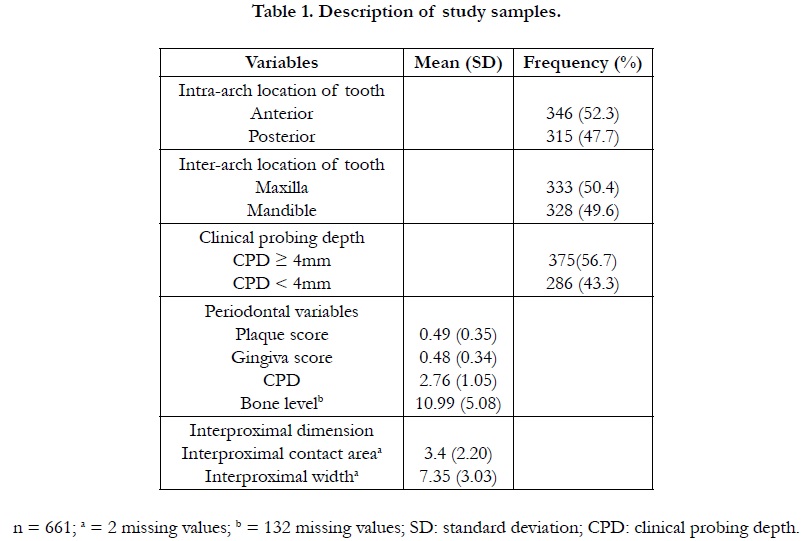
From 30 participants involved, 661 teeth were selected as study
samples. The prevalence of periodontally affected teeth (CPD ≥
4mm) in this study samples was 56.7%, which was comparable
to 43.3% prevalence of the healthy gingiva/gingivitis (CPD <
4mm). The mean (standard deviation) plaque score and gingiva
score were 0.49 (0.35) and 0.48 (0.34), respectively. Detail description
of the study sample is shown in Table 1.
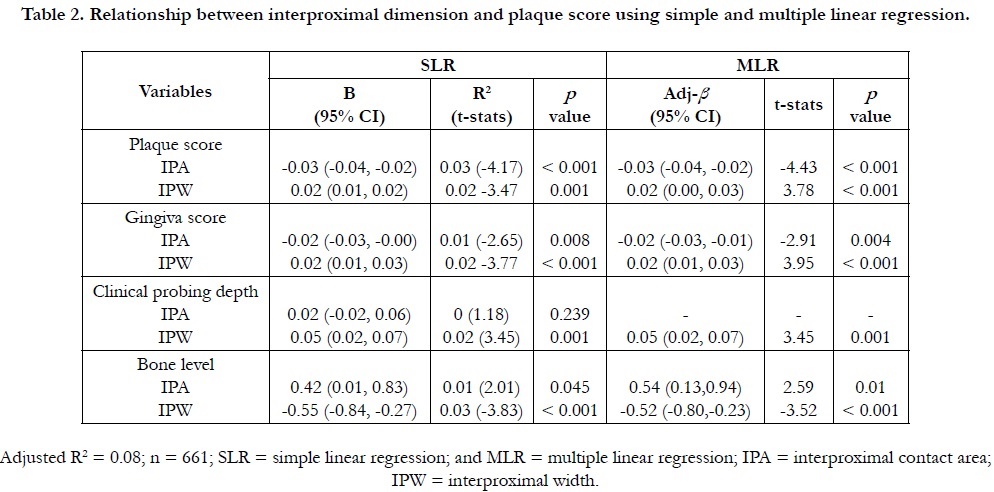
Simple (SLR) and multiple linear regression (MLR) analyses were carried out to investigate the relationship between the interproximal dimension and periodontal parameters (Table 2). The SLR analyses consistently showed that the interproximal contact area and width were both significantly related with plaque score, gingiva score and bone level, and MLR analyses confirmed that both the interproximal contact area and width were significant predictors for each plaque score, gingiva score and bone level model. Only in the clinical probing depth model, the interproximal contact area was found not a significant predictor.
Table 2. Relationship between interproximal dimension and plaque score using simple and multiple linear regression.
Discussion
The interproximal space is a pyramidal shape dimension bordered
by the interproximal contact area at the peak, interproximal tooth
surfaces on the mesial and distal sides, and alveolar bone crest at
the base [16]. In the ideal condition, this space should be filled
entirely by interdental papilla. Clinically, a precise measurement of
the interproximal space is very difficult to achieve if not impossible.
Researchers used various measurement methods in an attempt
to obtain a close estimation of the interproximal dimension. For
example, instead of measuring the surface contact area, the measurement
of the interproximal contact area can be represented by
the length of contact in an apicoincisal direction [14]. Depending
on the objective of the study, the height of the interproximal
space can be measured from the interproximal contact area to
either; the alveolar bone crest using transgingival probing, radiograph
methods or flap reflection methods [17-19]; or the gingival
zenith line connecting adjacent teeth [15, 20 21]. Since our study
was comparing the healthy and periodontally affected tooth, the
gingival zenith line method is thought to be more suitable because
of a stable reference point and non-invasiveness. However, due to
technical error in the measurement process, data on the interproximal
height were excluded from this manuscript. The horizontal
distance of the space is even harder to measure since there was no
actual marking ever documented for interproximal space. Some
studies used the gap between two adjacent roots for the estimation
of the horizontal distance of interproximal space [19, 22, 23].
In this study, the distance between gingival zenith points was used
to measure the horizontal distance of the interproximal area [24].
The interproximal space is not always fully occupied by the interdental
papilla. Observation by Tarnow et al. showed that when
the papilla reaches a certain height, the reduced amount of house
papilla started to be noticed [18], which usually presented with a
round or flat papillary tip, a black triangle. Apart from the obvious
aesthetic problem, the black triangle creates an unprotected interproximal
area [25], which leads to food impaction that reaches
from the facial or lingual/palatal direction. In addition, the reduced
fill interdental papilla area complicates the patient oral hygiene
care, hence encouraging dental biofilm retention. This study
explores how the interproximal space contributes to the biofilm
retention and establishment of periodontal disease.
We found in this study that the length of the interproximal contact
area has a strong negative relationship with the plaque and gingiva
score. The relation was found very weak with periodontal pocket,
and no relation was found with bone level. We were unable to
locate any similar study that evaluates the relationship between
the interproximal contact area and periodontal parameters. However,
the presence of the contact point was previously reported
in old studies to associate with lesser dental biofilm retention and
periodontal tissue inflammation [26, 27]. The size, position and
shape of the interproximal contact areas are varied, depending
on the factors like location and shape of the contact and tooth
contour [28]. A good interproximal contact will stabilise the tooth
in the alignment and prevents the contact from separation during
function. Thus, acting as an interproximal barrier against food
impaction. The small interproximal contact area was also found
to associate with increased height of the interproximal area and
reduced fill of interdental papilla [29, 30], where the reduced fill of interdental papilla is believed to associate with food impaction
and possibly biofilm retention.
In our study, the interproximal width was found to has a strong
positive relation with plaque score, gingival score and probing
depth, but a negative relation with the bone level. Through our
thorough literature search, we have not found any study that specifically
looked at the relationship between interproximal width
and the periodontal parameters. However, our finding could be
explained by the presence of a known direct relationship between
the interproximal contact area and width. Increased in the interproximal
width means an increase in the distance between teeth,
which is most probably associated with a loss or weak in the interproximal
contact and reduced the interdental papilla fill. These
conditions eventually drive to the dental biofilm formation and
retention, and periodontal inflammation [26, 31]. This inferential
statement is supported by our multiple regression analyses that
showed the interproximal contact area and width are the significant
predictors for the models of plaque score, gingiva score and
bone level (Table 2).
Interestingly, our data also showed that interproximal width was
negatively associated with bone level, contradicting with the finding
on clinical probing depth. This is probably best explained by
the understanding of the root proximity rule. A human histologic
study showed that the quality and quantity of the interproximal
bone are determined partially by the distance between the neighbouring
teeth, interproximal distance [32]. The close proximity
of the bone will reduce the thickness of lamina dura and cause
to the meagreness in cancellous bone, which was proposed to
create the vulnerability of interdental bone to external forces and
inflammation [33, 34]. Lack of cancellous bone quality was also
found to associate with reduced bone repair capability and bone
loss [22, 33].
This study evaluated the relationship between periodontal parameters
and the interproximal dimension in the subjects known
susceptible to periodontal disease. This intrasubject evaluation
approach is advantageous as we can reduce the effect of subject
heterogeneity factors such as genetics, age, diet, smoking, alcohol
intake or individual oral hygiene practices to the pathogenesis
of the periodontal disease [8, 35, 36]. On the other hand, the
study used a purposive sampling method, which is subjective and
non-probability in nature. This sampling method sets limitations
to the study as it creates the possibility of the researcher's bias
in making sample selection. Also, in the periodontal parameter
measurements, this study used the dichotomous, ordinal scale for
measuring plaque and bleeding on probing, which was derogatory.
This scale only allows us to determine the presence or absence
of plaque and bleeding on probing, and it does not give a true
quantitative measure of those variables.
Conclusion
Within the limitation of the study, we can conclude that the interproximal
contact area and width have a significant relationship
with the presence of dental biofilm, gingival bleeding and bone
level in the subjects susceptible to periodontal disease. The understanding
of the role of interproximal dimension in periodontal
inflammation may help the clinician in predicting the susceptible
teeth for periodontal disease and providing a personalised oral hygiene instruction as well as treatment planning. This data gives a
preceding for the future studies looking at the role of local factors
such as tooth rotation, crowding, drifting and displacement in the
susceptibility of periodontal disease.
Acknowledgement
The study was supported by the Universiti Sains Malaysia (USM)
through the USM research grant, Grant no: 304/PPSG/61313137.
References
- Kumar PS, Leys EJ, Bryk JM, Francisco J Martinez, Melvin L Moeschberger, Ann L Griffen. Changes in periodontal health status are associated with bacterial community shifts as assessed by quantitative 16S cloning and sequencing. J Clin Microbiol. 2006; 44:3665–3673. PMID: 17021095.
- Papapanou PN, Wennstrom JL, Grondahl K. Periodontal status in relation to age and tooth type. A cross-sectional radiographic study. J Clin Periodontol. 1988; 15:469–478. PMID: 3263400.
- Shi B, Chang M, Martin J, Makedonka Mitreva, Renate Lux, Perry Klokkevold, et al. Dynamic changes in the subgingival microbiome and their potential for diagnosis and prognosis of periodontitis. 2015; 6(1):e01926- 14. PMID: 25691586.
- Kornman KS, Loe H. The role of local factors in the etiology of periodontal diseases. Periodontol 2000. 1993; 2:83–97. PMID: 9673183.
- Albandar JM. Global risk factors and risk indicators for periodontal diseases. Periodontol 2000. 2002; 29:177–206. PMID: 12102708.
- Lindhe J, Okamoto H, Yoneyama T, A Haffajee, S S Socransky. Periodontal loser sites in untreated adult subjects. J Clin Periodontol. 1989; 16: 671– 678. PMID: 2613936.
- Gonzalez MK, Almeida AL, Greghi SL, Luiz Fernando Pegoraro, Jose Mondelli, Tatiana Moreno. Interdental papillary house: a new concept and guide for clinicians. Int J Periodontics Restor Dent. 2011; 31:e87-93. PMID: 22140673.
- Taba Jr. M, Souza SL, Mariguela VC. Periodontal disease: a genetic perspective. Braz Oral Res. 2012; 26 Suppl 1:32–38. PMID: 23318742.
- Silva-Boghossian CM, Colombo AP, Tanaka M, Carolina Rayo, Yizhi Xiao, Walter L Siqueira. Quantitative proteomic analysis of gingival crevicular fluid in different periodontal conditions. PLoS One. 2013; 8:e75898. PMID: 24098404.
- Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol. 2017; 44: 456–462. PMID: 28419559.
- O’Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972; 43:38. PMID: 4500182.
- Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975; 25:229–235. PMID: 1058834.
- Vandana KL, Haneet RK. Cementoenamel junction: An insight. J Indian Soc Periodontol. 2014; 18:549–554. PMID: 25425813.
- Stappert CF, Tarnow DP, Tan JH, Chu SJ. Proximal contact areas of the maxillary anterior dentition. Int J Periodontics Restor Dent. 2010; 30:471–477. PMID: 20814600.
- Olsson M, LJndhe J, Marinello CP. On the relationship between crown form and clinical features of the gingiva in adolescents. J Clin Periodontol. 1993; 20:570–577. PMID: 7691897.
- Takei HH. The interdental space. Dent Clin North Am. 1980; 24:169–176. PMID: 6928830.
- De Rouck T, Eghbali R, Collys K, Hugo De Bruyn, Jan Cosyn. The gingival biotype revisited: transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingiva. J Clin Periodontol. 2009; 36:428–433. PMID: 19419444.
- Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992; 63:995–996. PMID: 1474471.
- Cho HS, Jang HS, Kim DK, Joo-Cheol Park, Heung-Joong Kim, Seong-Ho Choi, et al. The effects of interproximal distance between roots on the existence of interdental papillae according to the distance from the contact point to the alveolar crest. J Periodontol. 2006; 77:1651–1657. PMID: 17032106.
- de Santana RB, de Miranda JLC, de Santana CMM. The relationship between open versus normal contact point and inter-proximal papilla dimensions in periodontally healthy young adults: A controlled clinical trial. J Clin Periodontol. 2017; 44:1164–1171. PMID: 28800146.
- Spear FM. Maintenance of the interdental papilla following anterior tooth removal. Pr Periodontics Aesthet Dent. 1999; 11: 21–8. PMID: 10218048.
- Tal H. Relationship between the interproximal distance of roots and the prevalence of intrabony pockets. J Periodontol. 1984; 55: 604–607. PMID: 6593454.
- Trossello VK, Gianelly AA. Orthodontic treatment and periodontal status. J Periodontol. 1979; 50: 665–671. PMID: 294480.
- Yin XJ, Wei BY, Ke XP, Zhang T, Jiang MY, Luo XY, et al. Correlation between clinical parameters of crown and gingival morphology of anterior teeth and periodontal biotypes. BMC Oral Health. 2020; 20:59.
- Nozawa T, Yamaguchi S, Ookame Y, Koichi Shimada, Koji Tanaka, Koichi Ito. The distances between the facial and palatal papillae in the maxillary anterior dentition. Eur J Esthet Dent. 2011; 6: 88–93. PMID: 21403929.
- Hancock EB, Mayo C V, Schwab RR, Wirthlin MR. Influence of interdental contacts on periodontal status. J Periodontol. 1980; 51:445–449. PMID: 6931204.
- Koral SM, Howell TH, Jeffcoat MK. Alveolar bone loss due to open interproximal contacts in periodontal disease. J Periodontol. 1981; 52:447–450. PMID: 6943330.
- Dörfer CE, von Bethlenfalvy ER, Staehle HJ, Pioch T. Factors influencing proximal dental contact strengths. Eur J Oral Sci. 2000; 108:368–377. PMID: 11037752.
- Chen MC, Liao YF, Chan CP, Yen-Chen Ku, Whei-Lin Pan, Yu-Kang Tu. Factors influencing the presence of interproximal dental papillae between maxillary anterior teeth. J Periodontol. 2010; 81:318–324. PMID: 20151812.
- Sharma AA, Park JH. Esthetic considerations in interdental papilla: remediation and regeneration. J Esthet Restor Dent. 2010; 22:18–28. PMID: 20136942.
- Jernberg GR, Bakdash MB, Keenan KM. Relationship between proximal tooth open contacts and periodontal disease. J Periodontol. 1983; 54:529– 533. PMID: 6579279.
- Heins PJ, Wieder SM. A histologic study of the width and nature of interradicular spaces in human adult pre-molars and molars. J Dent Res. 1986; 65:948–951. PMID: 3458748.
- Nielsen IM, Glavind L, Karring T. Interproximal periodontal intrabony defects. Prevalence, localization and etiological factors. J Clin Periodontol. 1980; 7:187–198. PMID: 6933161.
- Kim T, Miyamoto T, Nunn ME, Raul I Garcia, Thomas Dietrich. Root proximity as a risk factor for progression of alveolar bone loss: the Veterans Affairs Dental Longitudinal Study. J Periodontol. 2008; 79: 654–659. PMID: 18380558.
- Marsh PD. The significance of maintaining the stability of the natural microflora of the mouth. Br Dent J. 1991; 171:174–177. PMID: 1910971.
- Kinane DF, Preshaw PM, Loos BG. Host-response: understanding the cellular and molecular mechanisms of host-microbial interactions - consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol. 2011; 38 Suppl 1:44–48. PMID: 21323703.