Surgical Treatment of a Severe Bilateral Coronoid Process Hyperplasia with 5-Year Follow-Up
Pereira, Rafael MA1*, Marangon JR, Helvécio1, Rodrigues, Vitor C2, Campos, Gabrielle S2, Bizarria, Vitor D2, Mascarenhas, Gustavo M3
1 Adjunct Professor, School of Dentistry, University Center of Patos de Minas (UNIPAM), Patos de Minas, Minas Gerais, Brazil.
2 DDS student, School of Dentistry, University Center of Patos de Minas (UNIPAM), Patos de Minas, Minas Gerais, Brazil.
3 Private Practice, Salvador, Bahia, Brazil.
*Corresponding Author
Rafael Martins Afonso Pereira DDS, MSc,
Adjunct Professor, School of Dentistry, University Center of Patos de Minas (UNIPAM), Patos de Minas, Minas Gerais, Brazil.
Tel/Fax: +55 (34)3826-2500
E-mail: rafaelmap@unipam.edu.br
Received: March 31, 2020; Accepted: July 10, 2020; Published: July 23, 2020
Citation:Pereira, Rafael MA, Marangon JR, Helvécio, Rodrigues, Vitor C, Campos, Gabrielle S, Bizarria, Vitor D, Mascarenhas, Gustavo M. Surgical Treatment Of A Severe Bilateral Coronoid Process Hyperplasia With 5-Year Follow-Up. Int J Dentistry Oral Sci. 2020;7(7):781-784. doi: dx.doi.org/10.19070/2377-8075-20000153
Copyright: Pereira, Rafael MA©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
2.Case Report
3.Discussion
4.Conclusion
5.References
Introduction
Coronoid hyperplasia can be defined as an abnormal bony elongation
of a histologically normal coronoid process, mainly resulting
in progressive limitation of mouth opening but can also cause
pain and limitation of the mandibular movements [1-4].
It´s etiopathogenesis is still unknown and several hypotheses are
discussed, e.g.:trauma, temporal muscle hyperactivity, endocrine
system influence, genetic inheritance and temporomandibular
dysfunction. Coronoid hyperplasia is often confused with other
entities like osteoma, exostoses, osteochondroma and temporomandibular
joint disorders [5, 6].
Severe bilateral hyperplasia of the mandibular coronoid process is
a rare condition of development.
Case Report
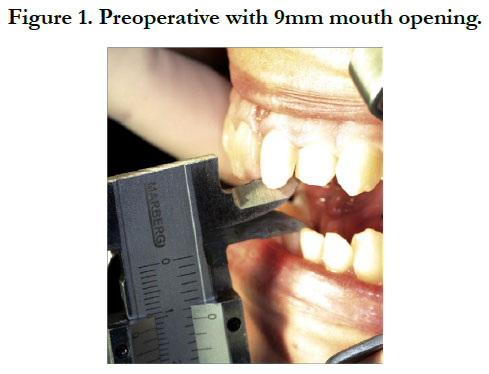
A 20 years old patient was referred for evaluation for the third
molar removal. Clinical exams showed a limited open mouth, referred
by the patient as a gradual limitation of mouth opening.
The patient first noticed the difficulty opening his mouth 2 years
earlier, but he did not realise it could become a problem. Clinical
examination revealed limitations of mandibular excursions and
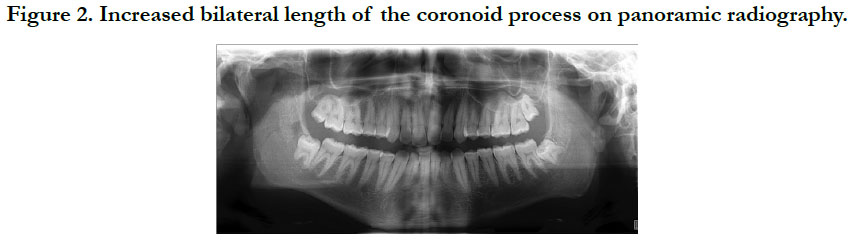
9mm mouth opening (Figure 1). Orthopantomography radiography
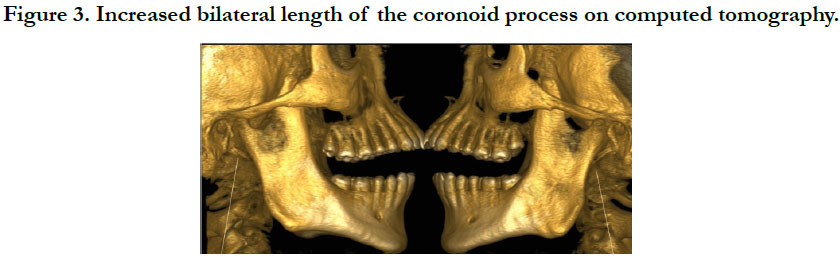
showed bilateral increase in the length of the mandibular
coronoid process. Computed tomography demonstrated the contact
of both coronoids processes with both left and right zygomatic
bones in mouth open position (Figures 2 and 3). There was
no history of maxillofacial injury or familial occurrence of similar
problems. treatmentindicated was surgical.
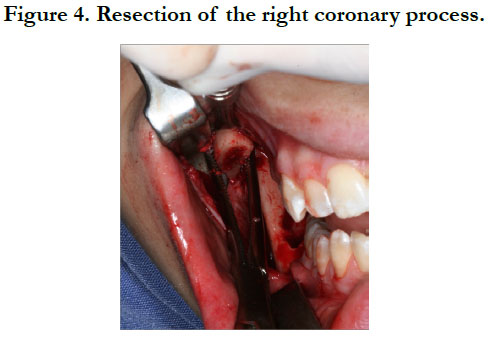
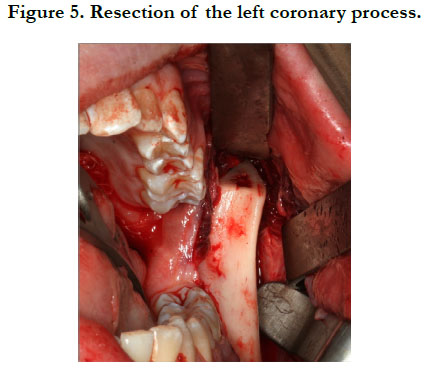
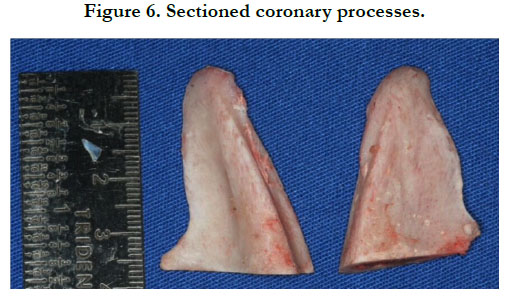
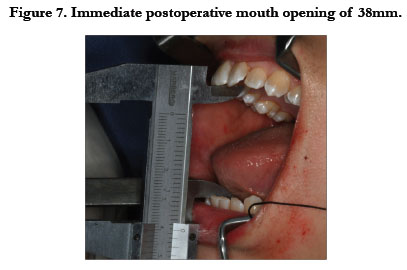
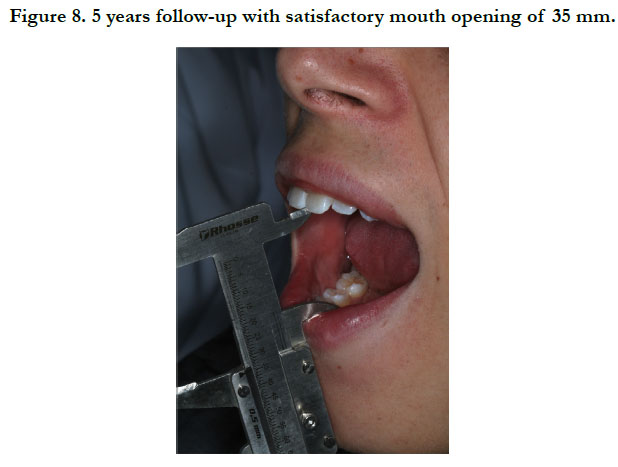
Bilateral coronoidectomy, consisted byremoving the coronoidmalar interferences by osteotomies at the base of the coronoid processes. A horizontal osteotomy was iniciated in the left sidewith a 702 bur and completed with a reciprocating saw. After completing the left side osteotomy, a Koscher clamp was left in place holding the coronoid process and the same technique was performed in the right side. After finishing both sides osteotomies, the mouth immediately opened, allowing a better approach to remove the large amount of bone needed.The temporalis muscle was detached and approximately 35mm length of the coronoid processes were intraorally removed in each side (Figures 4, 5 and 6). Combined removal of the impacted third molars were performed to actually treat the patients first complaint. The patient immediately evolved with significant improvement of mouth opening, achieving 38mm of mouth opening (Figure 7). The patient was referred for postoperative follow-up with a physical therapist. The removed material was sent for anatomopathological examination, and the clinical diagnosis of coronoid process hyperplasia was confirmed. After 5 years of postoperative follow-up, the patient has a stable condition, with no recurrence of hyperplasia of the coronoid processes, with satisfactory mouth opening of 35mm, demonstrating stability of the surgical treatment (Figure 8).
Discussion
Hyperplasia of the mandibular coronoid process is characterized
by cellular enlargement of bone considered histologically normal
[1, 3, 5, 7-9]. The symptoms, caused by this anomaly, gradually appears.
8. This condition results in contact of the hyperplastic coronoid
process withthe posterior portion of the zygomatic bone [3,
10-12], thus causing limitation in the mouth opening [13].
This abnormal growth can be classified as unilateral, usually more
reported in women, or bilateral, more often in men. The bilateral form has a 4.7:1 incidence when compared to the unilateral. The
male to female ratio is 5:1.1. The possibility of this abnormality
occur in the second decade of life has been more frequently
reported [9, 14], and its highest degree of severity occurs in the
third decade of life [15, 16].
The relapse of this condition has been exposed a few times. Thus,
authors have suggested hypotheses of its cause, such as a postoperative
bruise, ineffective physical therapy or inadequate nutrition.
Therefore, supervision with the aid of imaging exams is necessary
to monitor the regression of the abnormality [16].
The diagnosis of hyperplasia of the mandibular coronoid process
is usually made in youth, between childhood and adolescence.
However, as the patient progresses slowly, it may take up to 09
years to seek treatment in bilateral cases and approximately 07
years in unilateral cases [17].
Over time, hyperplasia of the mandibular coronoid process causes
significant problems, one of them being the difficulty in cleaning
the oral cavity, thus leading to an increased incidence of caries
and other diseases. In addition, due to a very sharp reduction in
mouth opening, the reach of the posterior teeth is compromised,
making much of the procedures performed by the dentist difficult.
The lower is the patient's ability to open the mouth, the
greater is the complexity of performing intubation for general
anesthesia, becoming necessary in many cases to perform nasal
intubation using a bronchofibroscope [18].
Because it is a condition whose signs and symptoms resemble
other diseases, the diagnosis of hyperplasia of the mandibular
coronoid process becomes difficult, and complementary examinations
are essential [18]. It is possible to observe, through radiographic
examinations, an exacerbated volume of the coronoid process [2, 19-21]. By means of computed tomography in threedimensional
reconstruction, it is possible to visualize, with greater
accuracy, not only the degree of deformity of the mandible [22],
but also the contact between the structures that are generating a
physical barrier to the mouth opening [20, 21-23].
Differential diagnosis of mandibular coronoid process hyperplasia
with other conditions such as ankylosis, osteoma, osteochondroma,
trauma, irradiation, thickened coronoid processes, nonreducing
anterior disc displacement, post-neurosurgical temporal
muscle fibrosis, and foreign body reaction is critical [1, 9, 14, 24,
25].
The treatment of mandibular coronoid process hyperplasia is basically
surgical and its objective is the removal of the coronoid
process and, consequently, the elimination of the mechanical barrier
that limits the mouth opening [18]. The most used surgical
procedure is the coronoidectomy, as it is an intervention that will
remove the impact that exists between the coronoid process and
the zygomatic bone [4].
Surgical access can be performed intraorally, being considered the
best approach and performed in 90% of cases [1, 4], or extraorally,
and the surgeon may choose submandibular, pre-auricular access,
bi-temporal or coronary plane [18, 19].
According to the patient's condition, with reduced temporal muscle
functions, postoperative physical therapy is recommended to
have a more satisfactory prognosis [3, 12, 17, 20, 25].
For hyperplasia of the mandibular coronoid process, intraoral access
coronoidectomy is recommended, followed by postoperative
physiotherapy, as it is possible to reestablish natural muscle physiology
and prevent the development of scar tissue [8, 9, 20].
The use of medication is also opportune, such as muscle relaxants,
which help in the physiotherapy phase. The use of bisphosphonates
may be an option as they act on alkaline phosphatase
levels, decreasing osteoclast action and bone turnover [16].
Conclusion
In conclusion, bilateral hyperplasia of the mandibular coronoid
process is a condition that deserves the attention of dental surgeons
because it is often confused with other diseases and negatively
influence the quality of life of patients. Complementary
examinations for correct diagnosis is necessary, especially panoramic
radiographyand computed tomography. In this case, surgical
coronoidectomy with intraoral approach, associated with
postoperative physiotherapy, proved to be the best approach for
the definitive treatment of bilateral mandibular coronoid hyperplasia,
presenting satisfactory and stable results after 05 years of
follow-up.
References
- PM McLoughlin, C Hopper, NB Bowley. Hyperplasia of the mandibular coronoid process: an analysis of 31 cases and a review of the literature. J Oral Maxillofac Surg. 1995 Mar;53(3):250-5.Pubmed PMID: 7861274.
- M Gross , A Gavish, S Calderon, E Gazit. The coronoid process as a cause of mandibular hypomobility-case reports. J Oral Rehab. 1997 Oct;24(10):776- 81. Pubmed PMID:9372469.
- CH Mulder, SI Kalaykova, RA Th Gortzak. Coronoid process hyperplasia: a systematic review of the literature from 1995. Int J Oral Maxillofac Surg. 2012 Dec;41(12):1483-9. Pubmed PMID:22608198.
- Da Silva JR, dos Santos Pereira R, Águeda C, Nunes PM, Marin C, Hochuli- Vieira E. Bilateral coronoid hyperplasia in a 43-year-old patient treated with intraoral coronoidectomy. J Craniofac Sur. 2017 Jun 1;28(4):e402-3.
- Iqbal S, Hamid AL, Purmal K. Unilateral coronoid hyperplasia following trauma: a case report. Dent Traumatol. 2009 Dec;25(6):626-30.
- Ilguy M, Kursoglu P, Ilguy D. Three cases of elongated mandibular coronoid process with different presentations. Iran J Radiol. 2014;11(1):e4031.Pubmed PMID:24693298.
- Costa YM, Porporatti AL, Stuginski-Barbosa J, Cassano DS, Bonjardim LR, Conti PC. Coronoid process hyperplasia: an unusual cause of mandibular hypomobility. Braz Dent J. 2012;23(3):252-255.Pubmed PMID:22814695.
- Romano M, Porcellini G, Rossi D,A Bolzoni , A B Giannì , F J Silvestre , et al. Bilateral coronoid hyperplasia: a report of six cases. J Biol Regul Homeost Agents. 2017;31(2 Suppl 1):139-145.Pubmed PMID:28691465.
- Ozkaya O, Colak O, Sutcu M, Akan M. The outcome of coronoidectomy in bilateral coronoid process hyperplasia. Cranio. 2018;36(1):53-60.Pubmed PMID:28220716.
- Alves RD, Silva PF, Veiga PH, Daher CR. The effectiveness of the physiotherapeutic resources in the gain of the amplitude of bucal opening in patients with craniomandibular dysfunctions. Rev Odontol UNESP.2013 Jun 4;39(1):55-61.
- Chakranarayan A, Jeyaraj P. Coronoid hyperplasia in chronic progressive trismus. Med Hypotheses. 2011;77(5):863-868. Pubmed PMID:21864990.
- Kim SM, Lee JH, Kim HJ, Huh JK. Mouth opening limitation caused by coronoid hyperplasia: a report of four cases. J Korean Assoc Oral Maxillofac Surg. 2014;40(6):301-307.Pubmed PMID:25551096.
- Starch-Jensen T, Kjellerup AD. Bilateral Elongated Mandibular Coronoid Process and Restricted Mouth Opening: A Case Report. Open Dent J. 2017;11:670-678.Pubmed PMID:29387283.
- Tolentino MC, Assis JS, Manzi FR. Mandibular coronoid process hyperplasia: a case report. Revista CEFAC. 2018 May;20(3):400-5.
- Giacomuzzi D. Bilateral enlargement of the mandibular coronoid processes: review of the literature and report of case. J Oral Maxillofac Surg. 1986;44(9):728-731.Pubmed PMID:3462364.
- Smyth AG, Wake MJ. Recurrent bilateral coronoid hyperplasia: an unusual case. Br J Oral Maxillofac Surg. 1994;32(2):100-104. Pubmed PMID:8199139.
- Choi MG, Kim DH, Ki EJ, Cheon HM. Trismus Due to Bilateral Coronoid Hyperplasia. Maxillofac Plast Reconstr Surg. 2014;36(4):168-172.Pubmed PMID:27489829.
- Ghazizadeh M, Sheikhi M, Salehi MM, Khaleghi A. Bilateral coronoid hyperplasia causing painless limitation of mandibular movement. Radiol Case Rep. 2017;13(1):112-117.Pubmed PMID:29487645.
- Hayter JP, Robertson JM. Surgical access to bilateral coronoid hyperplasia using the bicoronal flap. Br J Oral Maxillofac Surg. 1989;27(6):487-493. Pubmed PMID:2597660.
- Fernández Ferro M, Fernández Sanromán J, Sandoval Gutierrez J, Costas López A, López de Sánchez A, Etayo Pérez A. Treatment of bilateral hyperplasia of the coronoid process of the mandible. Presentation of a case and review of the literature. Med Oral Patol Oral Cir Bucal. 2008;13(9):E595- E598.Pubmed PMID: 18758406.
- Torenek K, Duman SB, Bayrakdar IS, Miloglu O. Clinical and radiological findings of a bilateral coronoid hyperplasia case. Eur J Dent. 2015;9(1):149- 152.Pubmed PMID:25713499.
- Mutoh Y, Ohashi Y, Uchiyama N, Terada K, Hanada K, Sasaki F. Threedimensional analysis of condylar hyperplasia with computed tomography. J Craniomaxillofac Surg. 1991;19(2):49-55.Pubmed PMID:2037691.
- Monevska DP, Benedetti A, Popovski V, Naumovski S, Grcev A, Bozovic S,et al. Mandibular Movement Restoration in a Child with Bilateral Coronoid Hyperplasia: A Case Report. Open Access Maced J Med Sci. 2016;4(2):293- 295.Pubmed PMID:27335604.
- Tavassol F, Spalthoff S, Essig H, Bredt M, Gellrich NC, Kokemüller H. Elongated coronoid process: CT-based quantitative analysis of the coronoid process and review of literature. Int J Oral Maxillofac Surg. 2012;41(3):331- 338.Pubmed PMID:22192388.
- Domingos V, Freitas CF, Fenyo-Pereira M, Raitz R. Perception of professionals in the assessment of coronoid hyperplasia by computed tomography. Acta Odontol Latinoam. 2015;28(1):58-63.Pubmed PMID:25950164.