Knowledge and Awareness on HIV/AIDS among College Students in A University Hospital Setting
Harsha L1, Vishnu Priya V2*, R.Gayathri3
1 Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India.
2 Professor, Department of Biochemistry, Saveetha Dental College and Hospitals, Saveetha Insti-tute of Medical and Technical Sciences, Saveetha University, Chennai, India.
3 Associate Professor, Department of Biochemistry, Saveetha Dental College and Hospitals, Sa-veetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India.
*Corresponding Author
Dr.Vishnu Priya.V,
Professor, Department of Biochemistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India.
E-mail: drvishnupriyav@gmail.com
Received: October 20, 2020; Accepted: December 01, 2020; Published: December 07, 2020
Citation:Harsha L, Vishnu Priya V, R.Gayathri. Knowledge and Awareness on HIV/AIDS among College Students in A University Hospital Setting. Int J Dentistry Oral Sci. 2020;7(12):1182-1186. doi: dx.doi.org/10.19070/2377-8075-20000234
Copyright: Vishnu Priya.V©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: The aim of the present survey is to assess the degree of knowledge and awareness about the basics of HIV virus, mode of
transmission and oral manifestations of AIDS among undergra-duate students at an university hospital setting, Chennai.
Materials and Methods: A Questionnaire based study was conducted to assess the de-gree of knowledge and awareness about
the basics of HIV virus, mode of transmission and oral manifestations of AIDS among 100 undergraduate students at an university
hospital setting, Chennai. All participants were provided with a pre structured questionnaire comprising of 28 questions related
to Human immunodeficiency virus (HIV) and Acquired immune deficiency syndrome ( AIDS) and answering was completely
self based. The questions were divided into 3 segments (a) basics of Human immunodeficiency virus (b) mode of transmission
and (c) oral manifestations of AIDS. The possible options chosen by the participants were tabulated and the percentile for each
question was calculated.
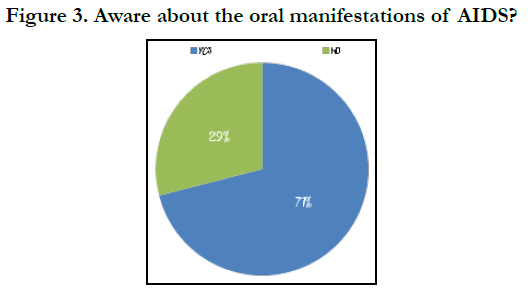
Results: Among the 100 participants, 95% of the participants gave correct answers for ques-tion on the basics of Human immunodeficiency
virus. 89% participants chose the correct answers under the section, mode of transmission and 71% of the participants
were aware about the oral manifestation of AIDS.
Conclusion: The study was to assess the knowledge of interns about HIV/AIDS. As dental surgeons are exposed to patients
with and without AIDS, its is essential that they are aware of the methods of transmission of this viral disease and also are able to
diagnose undiagnosed cases through oral manifestation. This would help prevent transmission of this deadly disease.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.Conclusion
7.Refereces
Keywords
AIDS; Autoimmunity; Humman Immunodeficiency Virus.
Introduction
Approximately 38.8 million people are living with HIV worldwide
and around 1.2 million deaths have been recorded unto 2015
[1]. The possibility of exposure to blood borne pathogens like
Hepa-titis B (HBV), Hepatitis C (HCV) and HIV put health care
workers at high risk [2-4] Similarly, patients are at risk of transmission
from health care workers but this risk is considered to
be ex-tremely low according to the available literature [2]. In particular,
dental care professionals are also exposed to a wide range
of infectious pathogens like HIV, HBV, Herpes B virus, HBC
virus and many others while performing dental procedures [5].
However, the risk of contracting HIV through needle stick or cut
exposure is extremely low (0.3%) as 99.7% of the exposures to
HIV contaminated blood do not cause infection [6]. Therefore,
the occupational risk of acquiring HIV/AIDS among dental care
providers is low but they are at ten folds greater risk than other
individuals for becoming carriers of HBV [7, 8].
Dental professionals including dental students should realize that
they are ethically liable to treat their patients’ with HIV/AIDS.
However, they should have adequate knowledge of HIV related
transmission and positive attitudes in order to deliver their responsibility
of treating patients with HIV/AIDS. It is important
to assess the knowledge and attitudes of dental students which
helps in understanding their preparedness for treating HIV/
AIDS patients and if any modifications have to be incorporated
into the dental curriculum to instil positive attitudes in dental
students. Thus, the current study evaluated the knowledge and
awareness of HIV/AIDS among college students in an university hospital setting.
Materials and Methods
A questionnaire consisting of 28 questions related to HIV/AIDS
was formulated. It was dividd into 3 segments, (a) basics of Human
immunodeficiency virus (b) mode of transmission and (c)
oral manifestations of AIDS.
The questionnaire was distributed to 100 interns at Saveetha dental
college and hospitals, Chen-nai. Students were asked to choose
the best answer from the options given. The date was then collected
and the percentile distribution for each question was represented
using pie charts.
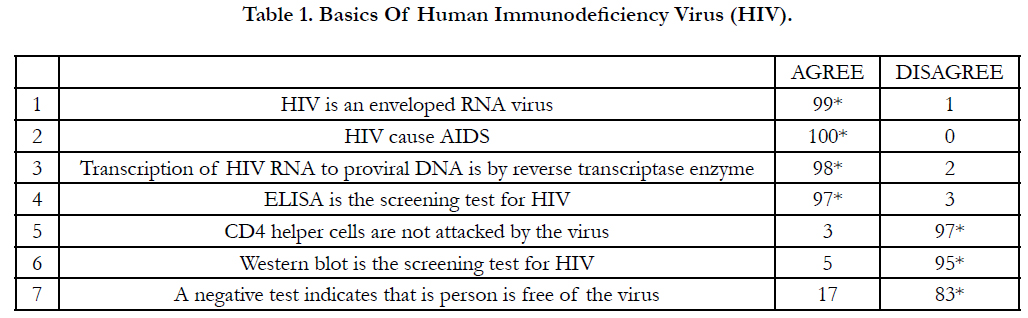
Out of the 100 participants in the present study, all of them were
aware of the fact that HIV causes AIDS( FIGURE 1). When
questioned about the structure of the virus, 99 participants gave
the correct answer as his being an enveloped RNA virus. 98 participants
chose reverse transcriptase as the enzyme involved in
transcription of HIV RNA to proviral DNA. 97 participants were
also aware that the cell group affected by the HIV virus are the CD4 helper cells. Questions with regard to the diagnosis of HIV/
AIDS was also put forth. 97 participants agreed that ELISA is the
screening test, and western blot is not. Western blot is a confirmatory
test for HIV/ADS.
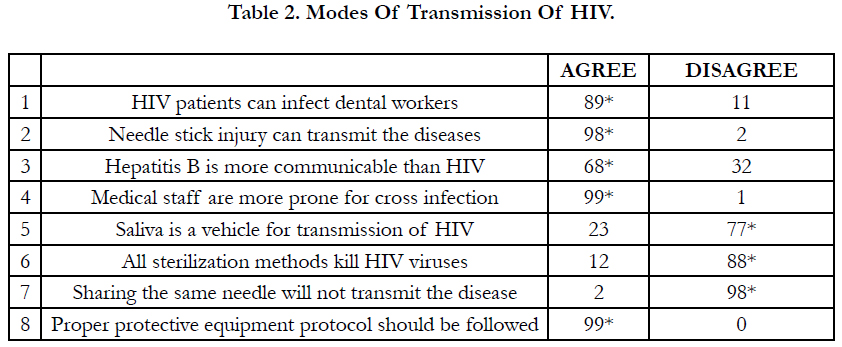
89% of the answers obtained were correct. When questions with
regard to transmission of the disease was put forth, 89 participants
on an average gave the correct answer. 98 participants agreed that
needle stick injuries could lead to the transmission of the virus. 99
participants agreed that medical professional are at a higher risk
of exposure to such an infectious disease. 77 partic-ipants contradicted
the fact that saliva could be a vehicle of transmission of the
disease. When questioned about sterilization protocols that must
be followed for affected patients, 88 partici-pants agreed that not
all sterilization procedures kill HIV viral spores. 99 % feel that
effective infection control is essential for prevention of transmission
of diseases( FIGURE 2).
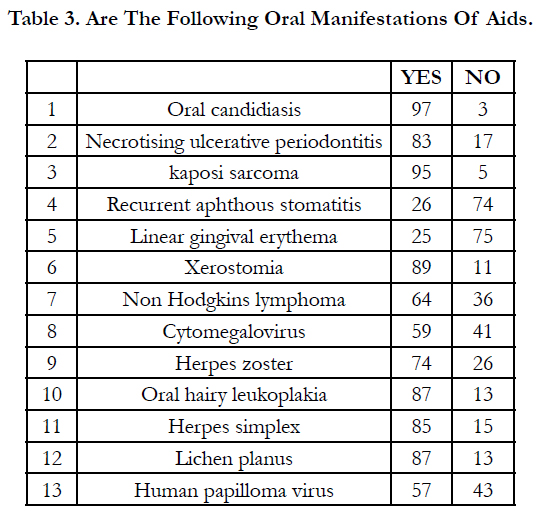
71% of the participants of the current study were about the oral
manifestations of AIDS (FIGURE 3).
Further questions with regard to each oral manifestation was put forth and the responses were tabulated.
Discussion
Newer diseases are having a profound worldwide impact on society
and on the delivery of medi-cal and oral health care. Acquired
immunodeficiency syndrome (AIDS), is caused by infection with
human immunodeficiency virus (HIV). Spread by blood borne
and sexual contact, HIV has infected over 36.1 million people in
the world and according to joint UNAIDS (United Nations Programme
on HIV/AIDS) and WHO, 1600 new cases are coming
up every day [9, 10].
HIV infection can be transmitted through unprotected sexual intercourse
with an infected part-ner. transmission routes also include injection or transfusion of contaminated blood or blood
products, infection through artificial insemination, skin grafts,
and organ transplants is also poss-ible(11), sharing unsterilized injection
equipment that was previously used by an infected person
[12] and maternal-fetal transmission (during pregnancy, at birth,
and through breastfeeding) [13]. Occupational HIV infections of
healthcare or laboratory workers may occur, but this mode of
infection is not frequent [14]. Transmission of HIV from an infected
patient to a health-care worker has been documented after
parenteral or mucous membrane exposure to blood. However,
this risk is less than 1%, is limited to exposure to blood, and can
be further minimized through the availability of more effective
Antiretroviral therapy (ART)[15].
Undiagnosed or untreated infection with HIV, results in progressive loss of immune function marked by depletion of the CD4+
T lymphocytes (CD4), leading to opportunistic infections and
malignancies characteristic of Acquired Immunodeficiency Syndrome
(AIDS)(16). Oral manife-stations of HIV are common
and have been important in identification of patients harboring
the HIV virus and in predicting the decline in their immune system.
Early recognition, diagnosis, and treatment of HIV-associated
oral lesions may reduce morbidity. Orofacial manifestations are
among the earliest and most common clinical signs of pediatric
HIV disease too. Early diagnosis of perinatally exposed infants
and children is especially important because the intervals between
infection, development of AIDS, and death are compressed in
pediatric patients. Early diagnosis allows prompt institution of
both multi-drug therapy, which appears to be most effective when
instituted early, and prophylactic therapy to forestall life-threatening
opportunistic infections.
Candidiasis: Candida albicans is the predominant yeast that colonizes
the oral cavity of both healthy subjects and HIV-infected
individuals in the developed and developing world. However, oral
pseudo-membranous candidiasis still remains the most common
fungal infection of HIV disease; it has been associated with more
frequent progression of HIV to AIDS and has been also used
as a clinical marker to define the severity of HIV infection [17],
with pseudomembranous candidiasis usually followed by erythematous
candidiasis.
Hairy Leukoplakia: Oral Hairy Leukoplakia (OHL) is a clinical
manifestation of Epstein-Barr virus (EBV) infection almost exclusively
found in patients with untreated advanced HIV disease
and typically occurs on the lateral border of the tongue of HIV
infected individuals and other groups of immunocom-promised
individuals [18].
Kaposi Sarcoma: Kaposi’s sarcoma (KS) is a malignant, multifocal
systemic disease that originates from the vas-cular endothelium
and has a variable clinical course. KS is caused by human herpes
virus 8 (HHV-8), which is transmitted sexually or via blood or
saliva. The most frequently involved site is the skin, but mucous
membranes, the lymphatic system, and viscera, in particular the
lung and gastrointestinal tract, can also be involved. In patients
with HIV disease, KS usually arises when the CD4+ T cell count
is less than 200 [19, 20].
Non Hodgkins Lymphoma: Non-Hodgkin’s Lymphoma
(NHL) is the second most common HIV-associated tumor. As
with KS, the frequency of this tumor has fallen with the introduction
of ART; however, it is still a very common tumor of HIVinfected
individuals in the developing world. A variety of NHLs
can arise in the mouth in HIV disease; in fact, a rare type called
plasmablastic lymphoma seems to nearly always arise exclusively
in the mouth [21].
Periodontal Diseases: Gingival and periodontal disease is common
in HIV infection, particularly in individuals residing in or
who have migrated from the developing world. HIV-gingivitis was
renamed as Linear gin-gival erythema, HIV-necrotising gingivitis
was renamed as Necrotising (ulcerative) gingivitis (NUG), HIVperiodontitis
was renamed as Necrotising (ulcerative) periodontitis
(NUP).
As the Oral manifestations are among the earliest and most important
indicators of HIV infec-tion, a better understanding of
these manifestations in both adults and children is a must for all
dental health care workers. Early recognition, diagnosis, and treatment
of HIV-associated oral lesions may reduce morbidity of the
adults. And for this, we need to be aware of the disease course of
HIV and AIDS.
The present study provides an insight of the degree of knowledge
and awareness of HIV/AIDS among interns at an university hospital
setting. This would help us in understanding if a need for the
use various other educational tools is required or not.
Conclusion
The study was a genuine endeavor to assess the knowledge of
dental interns about HIV/AIDS. As dental surgeons are exposed
to patients with and without AIDS, its is essential that they are
aware of the methods of transmission of this viral disease and
also are able to diagnose undiag-nosed cases through oral manifestation.
This would help prevent transmission of this deadly
dis-ease. The limitation of our study is that it was conducted in
one institute. Further assessment can be done by conducting surveys
in different universities and this was also help us know if
steps have to be taken to spread knowledge about the same.
References
- GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016 Oct 8;388(10053):1459-1544. Pubmed PMID: 27733281.
- Beltrami EM, Williams IT, Shapiro CN, Chamberland ME. Risk and management of blood-borne infections in health care workers. Clin Microbiol Rev. 2000 Jul;13(3):385-407. Pubmed PMID: 10885983.
- Cristina ML, Spagnolo AM, Sartini M, Dallera M, Ottria G, Perdelli F, Orlando P. Investi-gation of organizational and hygiene features in dentistry: a pilot study. J Prev Med Hyg. 2009 Sep;50(3):175-80.Pubmed PMID: 20411652.
- Singhal V, Bora D, Singh S. Hepatitis B in health care workers: Indian scenario. J Lab Phy-sicians. 2009 Jul;1(2):41-8. Pubmed PMID: 21938248.
- Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: a review. Ind Health. 2007 Oct;45(5):611-21. Pubmed PMID: 18057804.
- Gupta N, Tak J. Needlesticks injuries in dentistry. Kathmandu Univ Med J (KUMJ). 2011 Jul-Sep;9(35):208-12. Pubmed PMID: 22609509.
- Seacat JP, Inglehart MR. Education about treating patients with HIV infections/ AIDS: the student perspective. J Dent Educ. 2003 Jun;67(6):630-40. Pubmed PMID: 12856963.
- Kumar S, Tadakamadla J, Areeshi AYBH, Tobaigy HAWM. Knowledge and attitudes to-wards HIV/AIDS among dental students of Jazan University, Kingdom Saudi Arabia. Saudi Dent J. 2018 Jan;30(1):47-52. Pubmed PMID: 30166871.
- Aškinytė D, Matulionytė R, Rimkevičius A. Oral manifestations of HIV disease: A re-view. Stomatologija. 2015;17(1):21-8. Pubmed PMID: 26183854.
- National AIDS Control Organization .Prevention of HIV Transmission in health care Set-tings. In: Training Module on HIV Infection & AIDS for Medical Of cers.2003; 3-16.
- Najioullah F, Barlet V, Renaudier P, Guitton C, Crova P, Guérin JC, et al. Failure and suc-cess of HIV tests for the prevention of HIV-1 transmission by blood and tissue donations. J Med Virol. 2004 Jul;73(3):347-9. Pubmed PMID: 15170627.
- Metsch LR, Pereyra M, Purcell DW, Latkin CA, Malow R, Gómez CA, Latka MH; IN-SPIRE Study Team. Correlates of lending needles/syringes among HIV-seropositive injec-tion drug users. J Acquir Immune Defic Syndr. 2007 Nov 1;46 Suppl 2:S72-9. Pubmed PM-ID: 18089987.
- Salvatori F, De Martino M, Galli L, Vierucci A, Chieco-Bianchi L, De Rossi A. Horizontal transmission of human immunodeficiency virus type 1 from father to child. AIDS Res Hum Retroviruses. 1998 Dec 20;14(18):1679-85. Pubmed PMID: 9870322.
- Fraser VJ, Powderly WG. Risks of HIV infection in the health care setting. Annu Rev Med. 1995;46:203-11. Pubmed PMID: 7598457.
- Marcus R, Kay K, Mann JM. Transmission of human immunodeficiency virus (HIV) in health-care settings worldwide. Bull World Health Organ. 1989;67(5):577-82. Pubmed PM-ID: 2692871.
- Patton LL. HIV disease. Dent Clin North Am. 2003 Jul;47(3):467-92. Pubmed PMID: 12848460.
- Ranganathan K, Hemalatha R. Oral lesions in HIV infection in developing countries: an overview. Adv Dent Res. 2006 Apr 1;19(1):63-8. Pubmed PMID: 16672552.
- Lin HC, Corbet EF, Lo EC. Oral mucosal lesions in adult Chinese. J Dent Res. 2001 May;80(5):1486-90. Pubmed PMID: 11437225.
- Martró E, Esteve A, Schulz TF, Sheldon J, Gambús G, Muñoz R, Whitby D, Casabona J; Euro-Shaks study group. Risk factors for human Herpesvirus 8 infection and AIDS-associated Kaposi's sarcoma among men who have sex with men in a European multicentre study. Int J Cancer. 2007 Mar 1;120(5):1129-35. Pubmed PMID: 17154170.
- Leão JC, Hinrichsen SL, de Freitas BL, Porter SR. [Human herpes virus 8 and Kaposi’s sarcoma]. Rev Assoc Med Bras.1999; 45: 55-62.
- Navarro CM, Shibli JA, Ferrari RB, d'Avila S, Sposto MR. Gingival primary extranodal non-Hodgkin's lymphoma as the first manifestation of acquired immunodeficiency syn-drome. J Periodontol. 2008 Mar;79(3):562-6. Pubmed PMID: 18315441.