Prevalence Of Trigeminal Neuralgia Among Patients Treated For Orofacial Neuralgia - An Institutional Based Retrospective Study
B Aishwarya Reddy1, Sivakumar M2*, Nivethigaa B3
1 Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University, 162, Poonamallee High Road,
Chennai-600077, Tamil Nadu, India.
2 Assistant Professor, Department of Oral & Maxillofacial Surgery, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical
Sciences, Saveetha University, 162, Poonamallee High Road, Chennai-600077, Tamil Nadu, India.
3 Senior Lecturer, Department of Orthodontics, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences,
Saveetha University, 162, Poonamallee High Road ,Chennai-600077, Tamil Nadu, India.
*Corresponding Author
Sivakumar M,
Assistant Professor, Department of Oral & Maxillofacial Surgery, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University,
162, Poonamallee High Road, Chennai-600077, Tamil Nadu, India.
E-mail: sivakumarm@saveetha.com
Received: November 10, 2020; Accepted: December 15, 2020; Published: December 18, 2020
Citation: B Aishwarya Reddy, Sivakumar M, Nivethigaa B. Prevalence Of Trigeminal Neuralgia Among Patients Treated For Orofacial Neuralgia - An Institutional Based Retrospective Study. Int J Dentistry Oral Sci. 2020;7(12):1289-1293. doi: dx.doi.org/10.19070/2377-8075-20000255
Copyright: Sivakumar M©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Trigeminal neuralgia is one of the most excruciating pain syndromes afflicting the orofacial region. Neuropathic pain is the result of a lesion or disease of the somatosensory system in the peripheral or central nervous system. It usually happens in short, unpredictable attacks that can last from a few seconds to minutes. The attacks stop as suddenly as they start. The trigeminal nerve carries sensation from the face to the brain. It’ s most common in women aged over 50. Symptoms range from mild to severe facial pain, often triggered by chewing, speaking or brushing teeth.The aim of the study was to check the prevalence of trigeminal neuralgia among patients treated for orofacial neuralgia. A total of 36 patients were taken and analysed for orofacial neuralgia. The data collection was done from the patient management software. The data was reviewed by two reviewers. The results were tabulated and analysed using SPSS software by IBM.Chi square test was performed to compare the data and check for its distributions. The statistical significance of p value is set at 0.05.Out of 36 patients, 66.7% of the patients had trigeminal neuralgia and 33.3% of the patients did not have trigeminal neuralgia. 61.1% of the patients were males and 38.9% of the patients were females.The most prevalent age group for trigeminal neuralgia was 41 to 50 yrs with the prevalence of 27.8%. Prevalence of trigeminal neuralgia in the patients treated for orofacial neuralgia is at a higher rate. It is more prevalent in males than in females. The most prevalent age group for the trigeminal neuralgia is 40 to 50yrs.
2.Introduction
3.Material and Methods
4.Statistical Analysis
5.Results
6.Discussion
7.Conclusion
8.Refereces
Keywords
Prevalence; Orofacial Neuralgia; Trigeminal Nerve; Trigeminal Neuralgia.
Introduction
Neuropathic pain is the pain caused by somatosensory nervous
system injury or disease. It may be classified based on its temporal
aspect as episodic or continuous.Previous studies on effectiveness
of chlorhexidine and biomedical waste management have been
done , which let us gain experience to work on the present study
[1, 2]. It is characterized by a short duration electric shock pain
lasting from seconds to minutes. Previously we have done studies
on pterygomaxillary disjunction and oral squamous cell carcinoma,
which were helpful to work on the current study [3, 4]. In
general there is a zone of trigger point which may be intra or extra
oral and when provoked by mild non- traumatic stimulus is able to
produce moderate to severe paroxysmal pain. Pain management
is an emergency procedure followed by the dentist [5, 6]. In the
latter, pain originates in the neural structures, is constant, continuous
and burning, with different and fluctuating levels of intensity,
sometimes without total remission. Dental anxiety is seen in a
maximum number of patients [7, 8] .Trigeminal neuralgia is an extremely
painful yet rare orofacial pain condition, and clear understanding
of its mechanism and management remains an enigma.
Maxillofacial trauma might occur in different patterns [9, 10].
Originally known as “tic douloureux” due to its characteristic facial
tics, this disorder may be described as a paroxysmal unilateral
facial pain along the distribution of one or more branches of the
trigeminal nerve. Viral infections like varicella zoster can also lead to trigeminal neuralgia [11, 12]. The maxillary and mandibular
branches of the trigeminal nerve are most commonly affected,
followed by the ophthalmic branch. Patients with severe pain can
be diverted with the help of virtual reality method for ease of the
treatment [13-15]. Trigeminal neuralgia has a variety of etiologies,
mass effect from metastases, viral infection, trauma, autoimmune
processes are considered to lead to impaired trigeminal
nerve function, often attributed to demyelination. Previously we
have worked on 3D changes in pharyngeal airway, which helped
us gain experience to work on the current study [16]. Pain associated
with trigeminal neuralgia is described as severe, sharp, electric
and stabbing, is unilateral and usually remains within the anatomic
distribution of the affected nerve branch, regardless of remissions
and exacerbations [17].
Trigeminal neuralgia pain is often triggered by chewing and swallowing,
and may even be triggered by light touch to the face [18].
The pain is often relieved by sleep and may have periods of remission
lasting from weeks to years [19]. While symptoms of trigeminal
neuralgia are limited to pain, the quality of life for patients is
profoundly worsened, which puts them at a high risk of depression
and other psychological disorders [20]. Patients with trigeminal
neuralgia tend to be asymptomatic when asleep, suggesting
a bidirectionality between neuropathic pain and sleep. As sleep
quality improves, pain sensitivity will decrease [21, 22]. The severity
of pain associated with trigeminal neuralgia and its devastating
psychological effects make a prompt diagnosis and treatment
essential. Without a proper understanding of its clinical features
and medical course, it may go undiagnosed for years [23, 24]. The
aim of the study was to check the prevalence of trigeminal neuralgia
among patients treated for orofacial neuralgia.
Materials And Methods
This study was done under a university setting.And it is a single
centered retrospective study. The similar ethnicity of the study
is that it is done with pro available data of the population. The
disadvantage of this study could be the geographic locations, limitations
and trends.
Two reviewers are involved in this study. The samples were taken
from the patients who underwent treatment from June 2019 to
March 2020. We reviewed patient records and analysed the data
of 86000 patients between June 2019 and March 2020. The total
number of patients reported with orofacial disorder were shortlisted
to 36, based on inclusion criteria of patients treated for orofacial neuralgic disorder. The study was commenced after approval
from the scientific review board, and the ethical clearance
was obtained from the ethical committee of the university with
the following ethical approval number - SDC/SIHEC/2020/DIASDATA/
0619-0320.
The patient list was identified and the case sheets were verified
with the help of treatment notes.
The data is obtained from the category “orofacial neuralgia treatment”.
The data was collected, verified, tabulated and analysed.
The data was imported to SPSS and the statistical Chi square test
was done by using SPSS software by IBM. The type of analysis
done in this study is descriptive and association.
Results And Discussion
Orofacial neuralgia is an unpleasant sensation caused by a noxious
stimulus that is mediated only along a specific nerve pathway
into the central nervous system, where it is interpreted as
pain. This pain can be etiologically classified into three groups
as somatic pain, neuropathic pain psychological pain. There are
many types of orofacial neuralgia, namely trigeminal neuralgia,
glossopharyngeal neuralgia, sphenopalatine ganglion neuralgia,
postherpeticneuralgia,etc. Among all those mentioned earlier,
Trigeminal neuralgia accounts for overall orofacial neuralgic disorder.
Trigeminal neuralgia is a painful, chronic condition involving
the trigeminal nerve. The pain caused due to trigeminal neuralgia
can be brought on by mild stimulation of the face, such as
brushing.
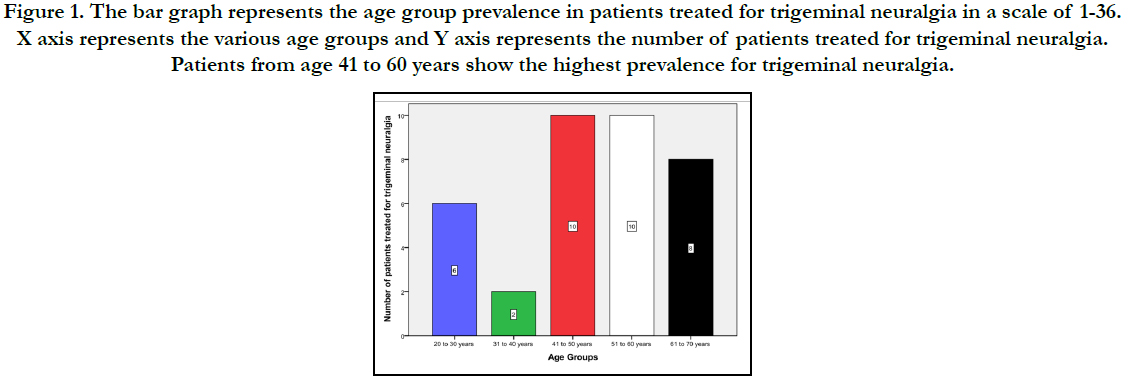
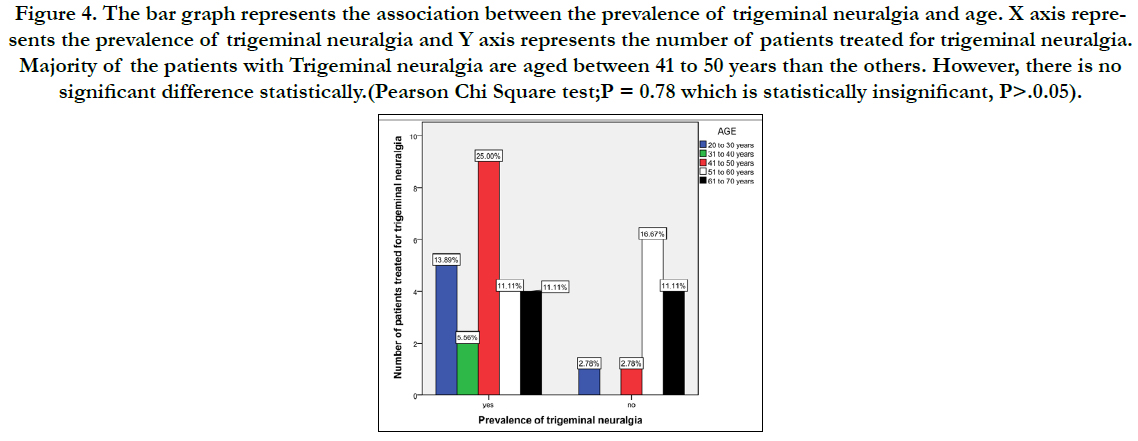
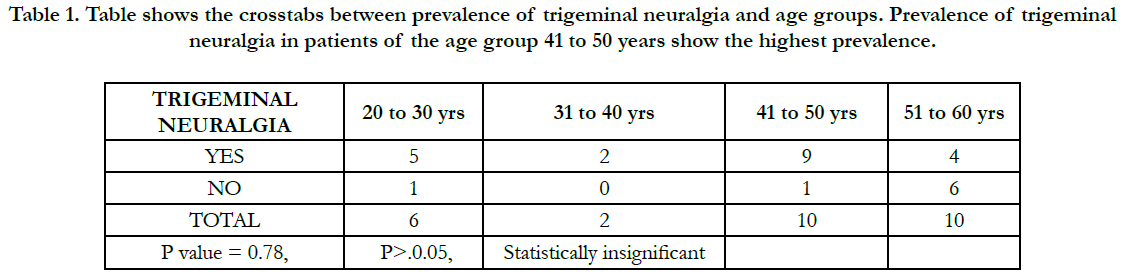
Trigeminal neuralgia occurs in the age groups ranging from 40 to
80 years and it is most common among 35 to 84yrs in males and 37
to 85yrs in females. The present study shows that the most prevalent
age group for Trigeminal l neuralgia was 41 to 50 yrs(red) and
51 to 60 yrs (white) with the percentage of 27.8%, followed by 61
to 70 yrs (black) with 22.2%, as depicted in Figure 1. A study by
Derafshi R, et.al, 2019 [25], also found that Trigeminal neuralgia
has been more common among 50 to 70 yrs (32%). Underlying
disease predisposing Trigeminal neuralgia could be due to multiple
sclerosis related neuralgia, traumatic neuroma,Cerebero-pontine
tumor and vascular lesion compressing trigeminal ganglion.
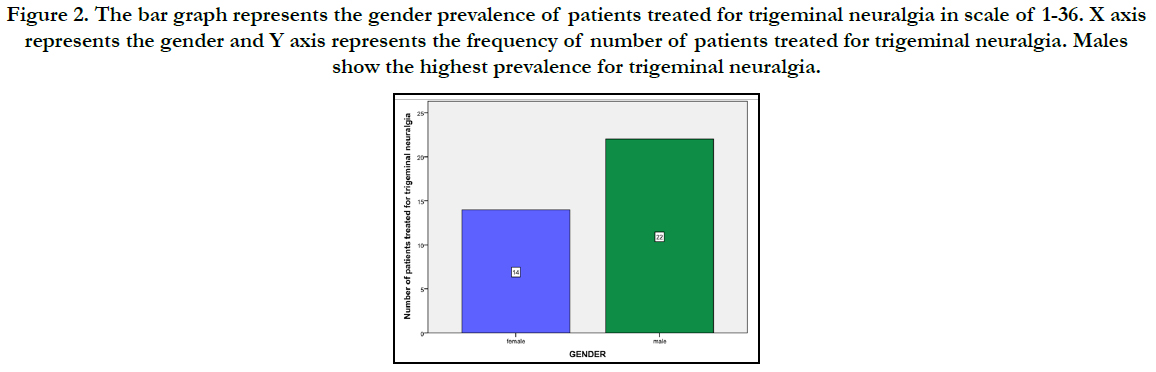
Out of the patients treated for Trigeminal neuralgia, 61.1% of the
patients were males(green) and 38.9% of them were females(blue)
as shown in Figure 2. According to the results, males show higher prevalence with 61.1% and females with 38.9%. Hence males are
more prevalent to Trigeminal neuralgia than females.When the
association analysis was done between age and prevalence of
trigeminal neuralgia, it was found patients from the age group
of 41 to 50 yrs(red) showed the highest prevalence for trigeminal
neuralgia in our institutional patient’s data. A study conducted
by ArpitaRai, et.al, 2017 [26], had similar results where the most
prevalent age group showing trigeminal neuralgia is 50 to 60 yrs
(33%) is in consensus with the present study.
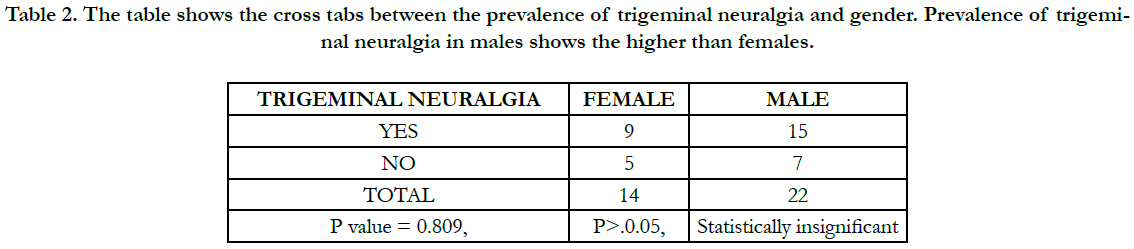
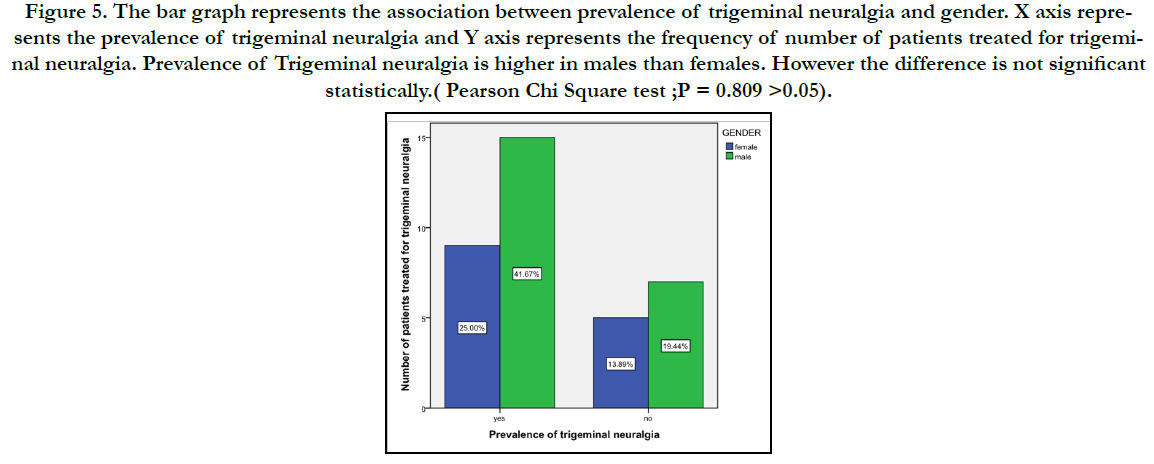
Association of gender and the prevalence of trigeminal
neuralgia,was assessed in the present study .Though it was
found not statistically significant, as shown in Table 2 and Figure
5,Males(green) showed higher prevalence with 62.5% than
females(blue) with 37.5%. A study given by Siqueira SR, et. al,
2009 [27], shows that females are more prevalent to trigeminal
neuralgia(65%). A study by Katheriya, et. al, 2019 [28], shows that
females are more prevalent (58.3%) to trigeminal neuralgia than males (41.7%). Previous studies are not in consensus. Out of 36
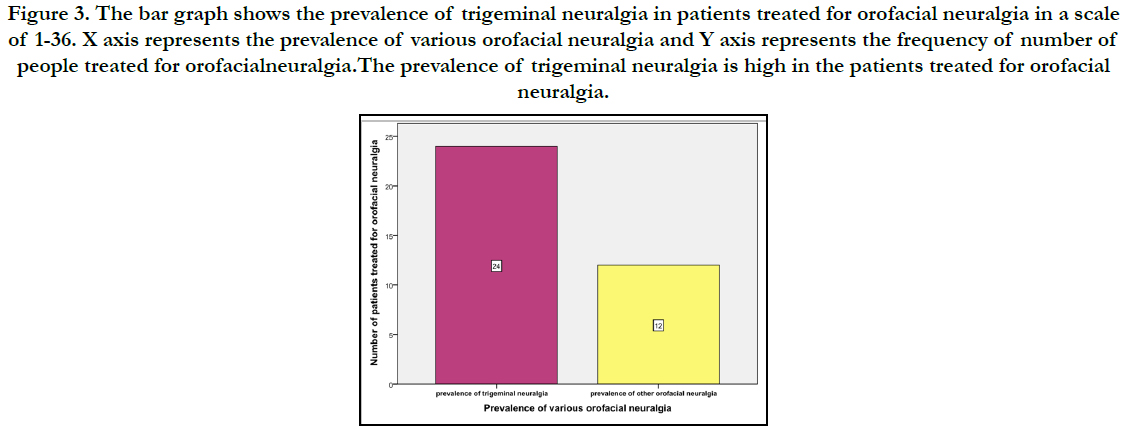
patients, the prevalence of trigeminal neuralgia is 66.7% (pink)
and 33.3% (yellow) of the patients did not have trigeminal neuralgia
as shown in Figure 3. In this study, prevalence of trigeminal
neuralgia is high (66.7%) among patients treated for orofacial
neuralgia.
Figure 1. The bar graph represents the age group prevalence in patients treated for trigeminal neuralgia in a scale of 1-36. X axis represents the various age groups and Y axis represents the number of patients treated for trigeminal neuralgia. Patients from age 41 to 60 years show the highest prevalence for trigeminal neuralgia.
Figure 2. The bar graph represents the gender prevalence of patients treated for trigeminal neuralgia in scale of 1-36. X axis represents the gender and Y axis represents the frequency of number of patients treated for trigeminal neuralgia. Males show the highest prevalence for trigeminal neuralgia.
Figure 3. The bar graph shows the prevalence of trigeminal neuralgia in patients treated for orofacial neuralgia in a scale of 1-36. X axis represents the prevalence of various orofacial neuralgia and Y axis represents the frequency of number of people treated for orofacialneuralgia.The prevalence of trigeminal neuralgia is high in the patients treated for orofacial neuralgia.
Figure 4. The bar graph represents the association between the prevalence of trigeminal neuralgia and age. X axis represents the prevalence of trigeminal neuralgia and Y axis represents the number of patients treated for trigeminal neuralgia. Majority of the patients with Trigeminal neuralgia are aged between 41 to 50 years than the others. However, there is no significant difference statistically.(Pearson Chi Square test;P = 0.78 which is statistically insignificant, P>.0.05).
Table 1. Table shows the crosstabs between prevalence of trigeminal neuralgia and age groups. Prevalence of trigeminal neuralgia in patients of the age group 41 to 50 years show the highest prevalence.
Table 2. The table shows the cross tabs between the prevalence of trigeminal neuralgia and gender. Prevalence of trigeminal neuralgia in males shows the higher than females.
Figure 5. The bar graph represents the association between prevalence of trigeminal neuralgia and gender. X axis represents the prevalence of trigeminal neuralgia and Y axis represents the frequency of number of patients treated for trigeminal neuralgia. Prevalence of Trigeminal neuralgia is higher in males than females. However the difference is not significant statistically.( Pearson Chi Square test ;P = 0.809 >0.05).
Zakrzewska JM, Linskey ME, 2009 , in their study have described that trigeminal neuralgia has the highest occurrence rate (43%) in patients treated for orofacial neuralgia. The present study where most of the patients reported with Orofacial neuralgia were finally diagnosed with Trigeminal neuralgia is in consensus with the previously mentioned study [29].
Hence it is very evident from the present study that the prevalence of trigeminal neuralgia is highly in the patients treated for orofacial neuralgia in the present study center. The most common age group affected is 41 to 50 yrs (red). Studies on more population should be done to explore the clinical features and treatment modalities in patients with trigeminal neuralgia.
Conclusion
From this retrospective study it can be concluded that prevalence
of trigeminal neuralgia in the patients treated for orofacial neuralgia
is at a higher rate. It is more prevalent in males than in females. The most prevalent age group for trigeminal neuralgia is 40 to
50yrs. Further a large sampled randomised control trial is necessary
to generalize the outcome of this study.
Acknowledgement
The authors sincerely acknowledge the Medical record department
faculties in helping and sorting out datas pertinent to this
study.
References
- Jesudasan JS, Wahab PU, Sekhar MR. Effectiveness of 0.2% chlorhexidine gel and a eugenol-based paste on postoperative alveolar osteitis in patients having third molars extracted: a randomised controlled clinical trial. Br J Oral Maxillofac Surg. 2015 Nov;53(9):826-30. PubmedPMID: 26188932.
- Kumar S, Rahman R. Knowledge, Awareness, And Practices Regarding Biomedical Waste Management Among Undergraduate Dental Students [Internet]. Asian Journal Of Pharmaceutical And Clinical Research. 2017; 10:341.
- Christabel A, Anantanarayanan P, Subash P, Soh CL, Ramanathan M, Muthusekhar MR, et al. Comparison of pterygomaxillarydysjunction with tuberosity separation in isolated Le Fort I osteotomies: a prospective, multi-centre, triple-blind, randomized controlled trial. Int J Oral Maxillofac Surg. 2016 Feb;45(2):180-5. PubmedPMID: 26338075.
- Marimuthu M, Andiappan M, Wahab A, Muthusekhar MR, Balakrishnan A, Shanmugam S. Canonical Wnt pathway gene expression and their clinical correlation in oral squamous cell carcinoma. Indian J Dent Res. 2018 May- Jun;29(3):291-297. PubmedPMID: 29900911.
- Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 2010 Aug;9(8):807-19. PubmedPMID: 20650402.
- Packiri S, Gurunathan D, Selvarasu K. Management of Paediatric Oral Ranula: A Systematic Review. J ClinDiagn Res. 2017 Sep;11(9):ZE06-ZE09. PubmedPMID: 29207849.
- Kumar S. Relationship between dental anxiety and pain experience during dental extractions. Asian Journal of Pharmaceutical and Clinical Research. 2017;10(3):458.
- Patil SB, Durairaj D, Suresh Kumar G, Karthikeyan D, Pradeep D. Comparison of Extended Nasolabial Flap VersusBuccal Fat Pad Graft in the Surgical Management of Oral Submucous Fibrosis: A Prospective Pilot Study. J Maxillofac Oral Surg. 2017 Sep;16(3):312-321. PubmedPMID: 28717289.
- Rao TD, Kumar MS. Analgesic efficacy of paracetamolvs ketorolac after dental extractions. Research Journal of Pharmacy and Technology. 2018 Aug 1;11(8):3375-9.
- Abhinav RP, Selvarasu K, Maheswari GU, Taltia AA. The Patterns and Etiology of Maxillofacial Trauma in South India. Ann Maxillofac Surg. 2019 Jan-Jun;9(1):114-117. PubmedPMID: 31293938.
- Kumar S, Sneha S. Knowledge And Awareness Regarding Antibiotic Prophylaxis For Infective Endocarditis Among Undergraduate Dental Students [Internet]. Asian Journal Of Pharmaceutical And Clinical Research. 2016. P. 154.
- Kumar S. The Emerging Role Of Botulinum Toxin In The Treatment Of Orofacial Disorders: Literature Update [Internet]. Vol. 10, Asian Journal Of Pharmaceutical And Clinical Research. 2017. P. 21.
- Kumar S. Knowledge, Attitude And Awareness Of Dental Undergraduate Students Regarding Hiv/Aids Patients [Internet]. Vol. 10, Asian Journal Of Pharmaceutical And Clinical Research. 2017. P. 175.
- Sweta VR, Abhinav RP, Ramesh A. Role of Virtual Reality in Pain Perception of Patients Following the Administration of Local Anesthesia. Ann Maxillofac Surg. 2019 Jan-Jun;9(1):110-113. PubmedPMID: 31293937.
- Patturaja K, Pradeep D. Awareness of Basic Dental Procedure among General Population. Research Journal of Pharmacy and Technology. 2016 Sep 1;9(9):1349.
- Vijayakumar Jain S, Muthusekhar MR, Baig MF, Senthilnathan P, Loganathan S, Abdul Wahab PU, et al. Evaluation of Three-Dimensional Changes in Pharyngeal Airway Following Isolated Lefort One Osteotomy for the Correction of Vertical Maxillary Excess: A Prospective Study. J Maxillofac Oral Surg. 2019 Mar;18(1):139-146. PubmedPMID: 30728705.
- Loeser JD, Treede RD. The Kyoto protocol of IASP Basic Pain Terminology. Pain. 2008 Jul 31;137(3):473-477. PubmedPMID: 18583048.
- Benoliel R, Heir Gm, Eliav E. Neuropathic Orofacial Pain [Internet]. Orofacial Pain And Headache. 2008. P. 255–94.
- D. Dw-sn. Trigeminal Neuralgia: A Natural Approach To Successful Nerve Pain Management. 2020. 108 P.
- Dash D. Differential Diagnosis of Trigeminal Neuralgia. InHandbook of Trigeminal Neuralgia 2019 (pp. 37-43). Springer, Singapore.
- HasslerRg, Albe-fessard Dg. Trigeminal Neuralgia: Pathogenesis And Pathophysiology. Edited By Rolf Hassler And A. Earl Walker. Contributions By D. Albe-fessard [Et Al.]. 1970. 196 P.
- The Pathophysiology Of Trigeminal Neuralgia [Internet]. Springerreference.
- Love S, Coakham HB. Trigeminal neuralgia: pathology and pathogenesis. Brain. 2001 Dec;124(Pt 12):2347-60. PubmedPMID: 11701590.
- Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, et al. American Academy of Neurology Society; European Federation of Neurological Society. AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol. 2008 Oct;15(10):1013-28. PubmedPMID: 18721143.
- Derafshi R, Rezazadeh F, Ghapanchi J, Basandeh Sharif D, Farzin M. Prevalence of Chronic Orofacial Pain in Elderly Patients Referred to Shiraz Dental School From 2005 to 2017. Anesth Pain Med. 2019 Dec 7;9(6):e91182. PubmedPMID: 32280612.
- Rai A, Kumar A, Chandra A, Naikmasur V, Abraham L. Clinical profile of patients with trigeminal neuralgia visiting a dental hospital: A prospective study. Indian Journal of Pain. 2017 May 1;31(2):94.
- Siqueira Sr, Teixeira Mj, Siqueira Jtt. Clinical Characteristics Of Patients With Trigeminal Neuralgia Referred To Neurosurgery [Internet]. Vol. 03, European Journal Of Dentistry. 2009. P. 207–12.
- Katheriya G, Chaurasia A, Khan N, Iqbal J. Prevalence Of Trigeminal Neuralgia In Indian Population Visiting A Higher Dental Care Center In North India. Natl J Maxillofac Surg. 2019 Jul;10(2):195–9.
- Zakrzewska Jm, Linskey Me. Trigeminal Neuralgia [Internet]. Orofacial Pain. 2009. P. 119–34.