Comparison Of Soft Tissue Treatment Changes between Twin Force Bite Corrector and Forsus Fatigue Resistance Appliance
Suvetha Siva1, Aravind S Kumar2*, Nivethigaa B3
1 Post-Graduate Student, Department of Orthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Velapanchavadi,
Chennai, India.
2 Professor and Head of the Department, Department of Orthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences,
Velapanchavadi, Chennai, India.
3 Senior Lecturer, Department of Orthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Velapanchavadi, Chennai,
India.
*Corresponding Author
Aravind S Kumar,
Professor and Head of the Department, Department of Orthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Velapanchavadi, Chennai,
India.
Tel: 9841299939
E-mail: aravindkumar@saveetha.com
Received: November 01, 2020; Accepted: December 03, 2020; Published: December 04, 2020
Citation:Suvetha Siva, Aravind S Kumar, Nivethigaa B. Comparison Of Soft Tissue Treatment Changes between Twin Force Bite Corrector and Forsus Fatigue Resistance Appliance. Int J Dentistry Oral Sci. 2020;7(12):1153-1159. doi: dx.doi.org/10.19070/2377-8075-20000229
Copyright: Aravind S Kumar©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: The aim of this study was to compare the soft tissue changes after two fixed functional appliances Twin Force Bite
Corrector and Forsus Fatigue Resistant Device treatment in patients with Class II division 1 malocclusion.
Materials and Methods: The sample consisted of 28 lateral cephalograms of 14 young adolescent patients, divided into two
groups. Group 1 consisted of 7 patients treated with fixed functional appliances associated with fixed appliances, Twin Force Bite
Corrector and initial mean overjet of 6.83 mm. Group 2 comprised 7 patients treated with fixed functional appliances associated
with fixed appliances, Forsus Fatigue Resistant Device and initial mean overjet of 7.01 mm. t-Tests were used to compare treatment
changes and the final cephalometric statuses between the groups.
Results: According to the results, there was no intergroup difference regarding the soft tissue changes.
Conclusion: Young adolescent patients treated with both the fixed functional appliances present similar soft tissue results. It is the
clinician choice to select the appliance pertaining to the type of patient he is treating.
Clinical Significance: Since there is a paradigm shift of considering the soft tissue profile for orthodontic treatment planning,
assessing the soft tissue changes is the new scope of research.
2.Introduction
3.Materials and Methods
4.Results and Discussion
5.Limitations
6.Acknowledgement and Declarations
7.Refereces
Keywords
Fixed Functional Appliance; Class II Malocclusion; Retrognathic Mandible; Soft Tissue Changes.
Introduction
In this contemporary society improvement in facial aesthetics has
become an aspect of utmost importance. Facial aesthetics has
also been recognized as one of the major motivations for seeking
orthodontic treatment [1-4]. In order to pursue an excellence in
facial aesthetic improvement, we are often faced with the need
to predict soft tissue profile changes resulting from a variety of
orthodontic appliances and techniques for the correction of the
same type of malocclusion, especially concerning the differences
between the treatment protocols [5]. This variety of options tends
to cause concerns as to which treatment modality will provide the
most improvement in the soft tissue profile.
Retrognathic profile is one of the characteristic features of class 2
division 1 patients. One of the goals of functional treatment is to
achieve a straight profile. For correction of skeletal class II with
retrognathic mandible either removable functional or fixed functional
appliances can be used. Fixed functional appliances have
the major advantage of not requiring patient compliance. They
can be used along with the brackets. Their disadvantages are that
they are difficult to clean and remove and are prone to breakage
[6].
The Forsus Fatigue Resistant Device (3M Unitek Corp Monrovia,
Calif) appliance consists of a push rod, that inserts into a
telescoping cylinder [7, 8]. It is available in various sizes, hence
a large inventory must be maintained, and chair side application
time is increased as size selection is needed. There are numerous studies that have evaluated the effects of the Forsus [9-11] and
compared it to intermaxillary elastics (Jones 2008) and untreated
controls [10].
The Twin Force Bite Corrector (TFBC; Ortho Organizers Inc,
Carlsbad, Calif) is a fixed, push-type intermaxillary appliance incorporating
ball-and-socket joints, which permits a wide range of
motion, lateral flexibility and full mandibular movement. There
are studies and case reports which have evaluated the treatment
effects of Twin Force Bite Corrector [12-16].
There are many previous studies which have evaluated the skeletal
and dental effects of Twin Force Bite Corrector appliance and
Forsus fatigue resistant device [11, 12, 17-19] but there are only a
very few studies which have evaluated its effects on soft tissues.
Previously our team had conducted numerous clinical trials [20]
[21-25], in vitro studies [26-29], reviews [30-32] and case reports
[33, 34] over the past few years. Now we are focusing on the paradigm
shift in orthodontics and conducting studies.The aim of the
study was to evaluate the changes in the facial soft tissues in skeletal
class II patients with retrognathic mandible after treatment
with the Twin Force Bite Corrector appliance and Forsus fatigue
resistant device.
Materials and Methods
This study was approved by the institutional Ethical committee.
A minimum sample size of 7 participants per group was proposed
for 80% power at a significance level of 0.05 to demonstrate
an inter-group post-treatment difference [35]. The sample
was prospectively studied in the Department of Orthodontics
and Dentofacial Orthopaedics, Saveetha Dental College, Chennai,
Tamilnadu, India. The Initial lateral cephalograms of 14 patients
with bilateral Class II molar relationship [36, 37] were divided into
two groups. Additional selection criteria included no agenesis, supernumerary
or lost teeth, maxillary arches without crowding,
mandibular arches with slight or no crowding at pretreatment.
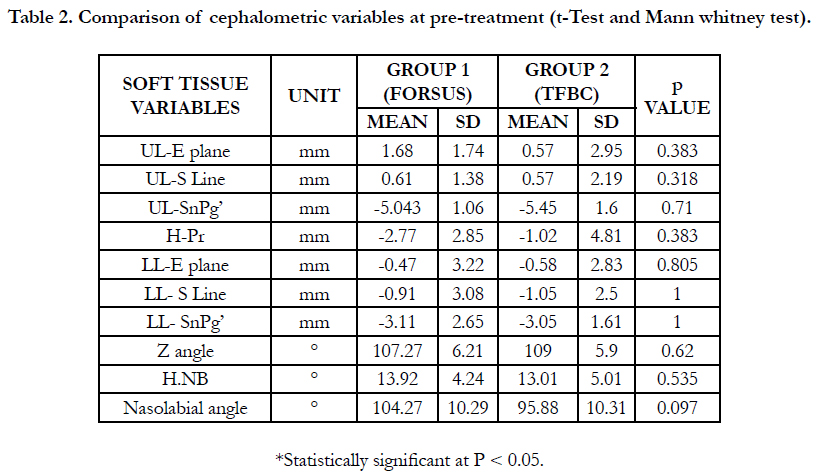
Group 1 consisted of 7 patients (3 boys, 4 girls) treated with Forsus
Fatigue Resistant device associated with fixed appliances with
initial and final mean ages of 12.71 and 15.16 years, respectively. The mean treatment time of fixed functional appliances was
0.72 years and the mean total treatment time was 2.44 years. This
group had initial and final mean overjets of 6.57 and 2.28 mm, respectively.
Four patients presented with complete bilateral Class II
malocclusion and three patients presented with bilateral ¾ Class
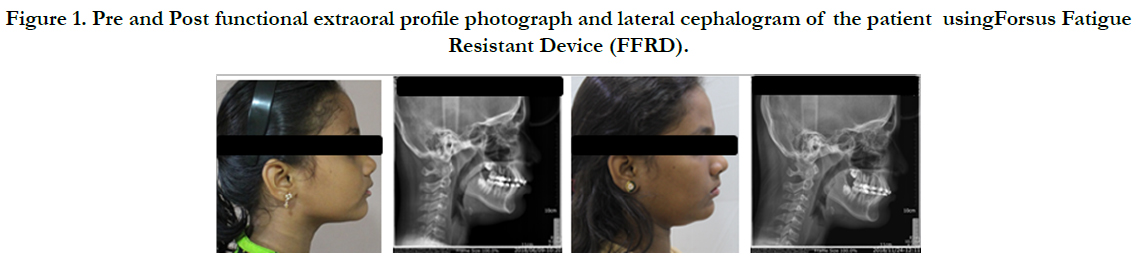
II malocclusion (Figure 1).
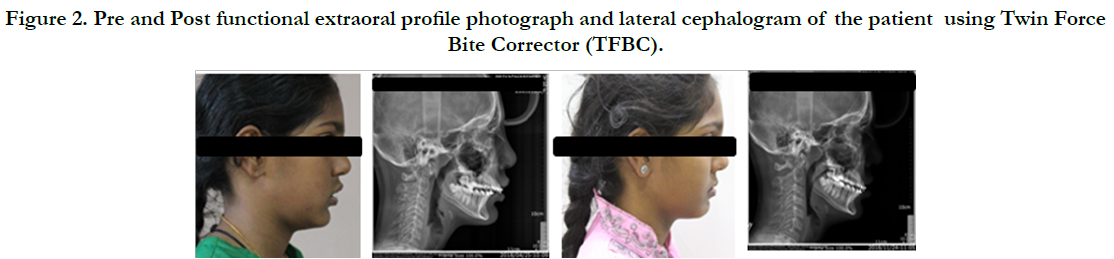
Group 2 consisted of 7 patients (1 boy, 7 girls) treated with Twin
Force Bite Corrector appliances associated with fixed appliances
with initial and final mean ages of 12.71 and 15.16 years, respectively.
The mean treatment time of fixed functional appliances
was 0.72 years and the mean total treatment time was 2.44 years.
This group had initial and final mean overjets of 7.28 and 2.57
mm, respectively. Five patients presented with complete bilateral
Class II malocclusion and two patients presented with bilateral ¾
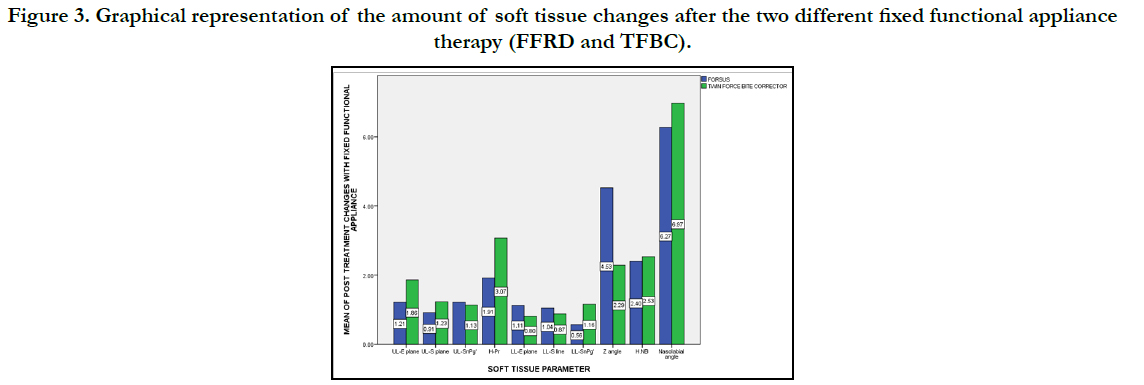
Class II malocclusion ( Figure 2 & 3).
Figure 1. Pre and Post functional extraoral profile photograph and lateral cephalogram of the patient usingForsus Fatigue Resistant Device (FFRD).
Figure 2. Pre and Post functional extraoral profile photograph and lateral cephalogram of the patient using Twin Force Bite Corrector (TFBC).
Figure 3. Graphical representation of the amount of soft tissue changes after the two different fixed functional appliance therapy (FFRD and TFBC).
The treatment sequence of the patients consisted of three treatment phases:
Phase 1: leveling and alignment of the maxillary and mandibular teeth ending with passive rectangular 19X25 stainless steel archwires.
Phase 2: placement of the fixed functional appliance that lasted until correction of the Class II anteroposterior discrepancy, with overcorrection of at least a quarter-cusp bilateral Class III molar relationship.
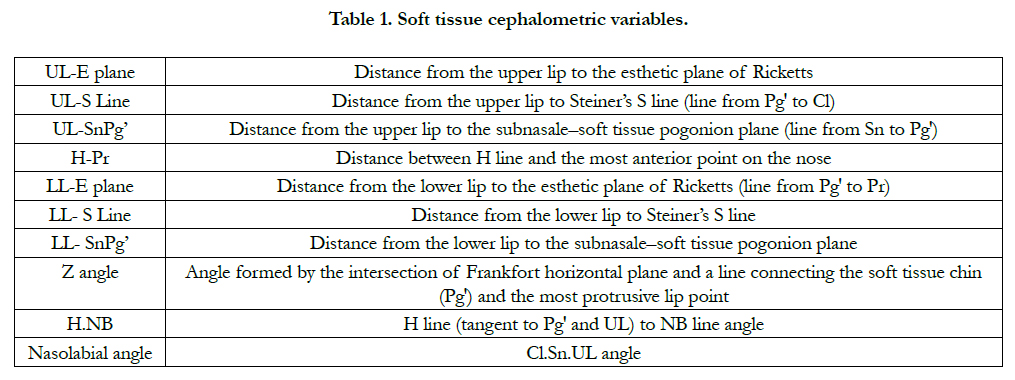
Phase 3: Active retention with the use of Class II intermaxillary elastics for 18 hours a day until the end of orthodontic treatment. The lateral cephalograms were obtained in centric occlusion, with the lips at rest. The initial and final lateral head films were digitally traced using FACAD software. (figure 1&2) Ten soft tissue variables were measured (Table 1). Skeletal maturity was assessed by using the cervical vertebral maturation (CVM) method [38].
Normal distribution was tested and confirmed. t-Tests and Mann-
Whitney test was used to compare the groups regarding the Class II malocclusion anteroposteriorocclusal severity and were also
used to compare the initial and final cephalometric characteristics
and the soft-tissue changes between the groups. Results were
considered statistically significant at P < 0.05. These analyses were
performed with SPSS Statistics software.
Results and Discussion
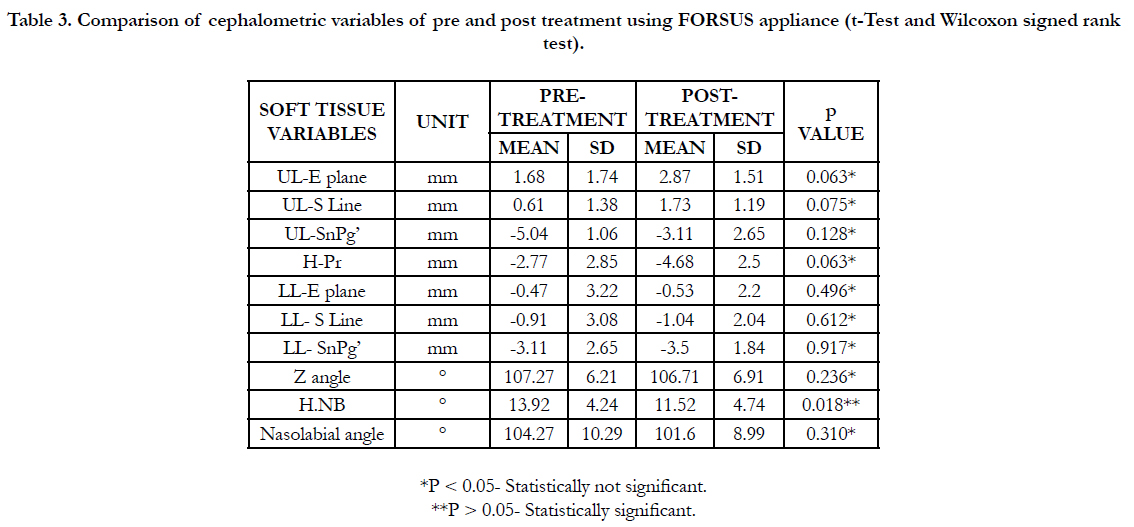
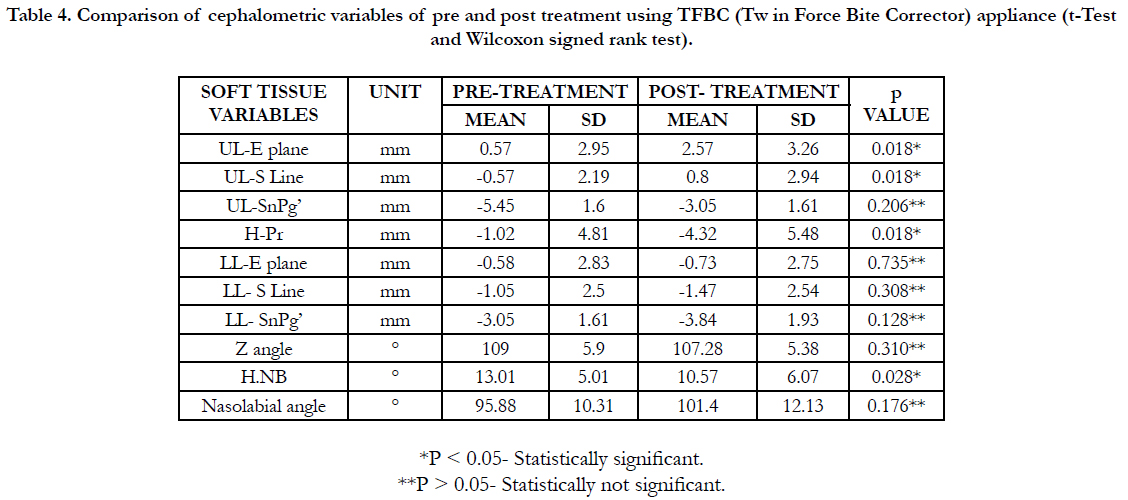
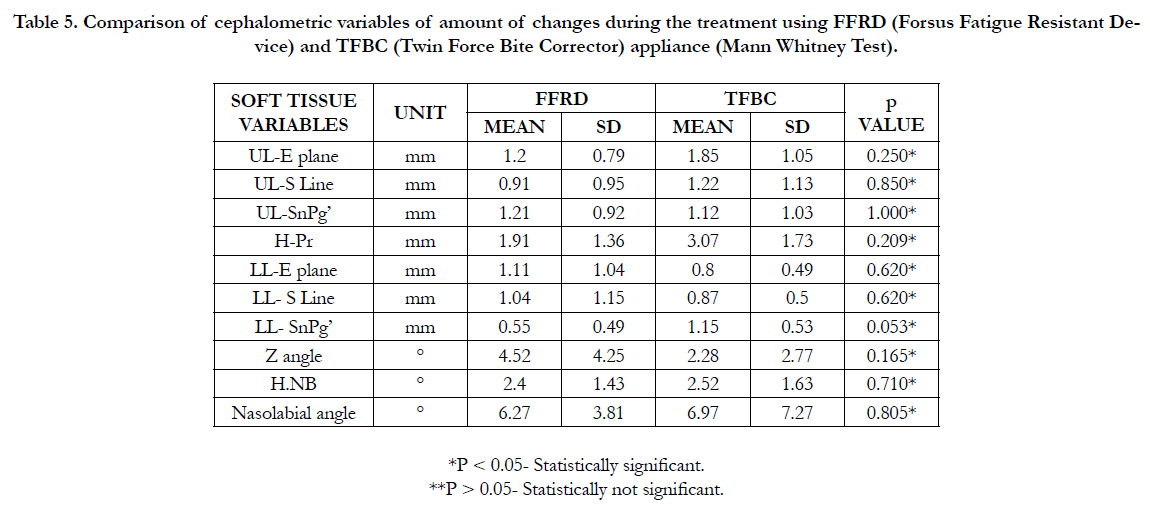
The results were compared regarding the pre and post treatment
soft tissue changes of two groups. ( figure 3) (Table 2, 3, 4 and
5). The results have shown that there is no statistically significant
difference between the two groups. But when the results were
compared within the groups, statistically significant results were
found in H.NB angle in Forsus group (p<0.05). In the TFBC
group, significant results were found in UL-E plane, UL-S Line,
H-Pr and H.NB values.
Table 3. Comparison of cephalometric variables of pre and post treatment using FORSUS appliance (t-Test and Wilcoxon signed rank test).
Table 4. Comparison of cephalometric variables of pre and post treatment using TFBC (Tw in Force Bite Corrector) appliance (t-Test and Wilcoxon signed rank test).
Table 5. Comparison of cephalometric variables of amount of changes during the treatment using FFRD (Forsus Fatigue Resistant Device) and TFBC (Twin Force Bite Corrector) appliance (Mann Whitney Test).
Ideally, the sample should include only patients with full cusp Class II malocclusions. However, to have strictly comparable initial morphologic characteristics between the groups, it was necessary to include patients with bilateral ¾ cusp Class II malocclusions because both the appliance group did not have enough patients that presented with initial full cusp Class II malocclusions. But the overjet was similar to or greater than the previous studies of the soft tissue profile changes [35, 39, 40]. The use of two different types of fixed functional appliances in group 1 and group 2 should not interfere with the results, because regardless of the device, their overall mechanisms of action and general effects are similar [39, 41-46]. obviously, there are small differences in the effects of the appliances. [47] However, specific treatment effect comparisons with the different appliances were not the focus of this study. The focus was only to investigate whether non-extraction treatment with two different fixed functional appliances would produce different soft tissue changes.
The little difference in skeletal and dentoalveolar changes did not produce any significantly different soft tissue changes between the groups. These similar soft tissue changes would be expected [4, 35, 40, 48-51] because the changes in the anteroposterior apical base relationship and overjet were similar between the groups [40-51]. However, one could speculate the amount of soft tissue changes within the group is more statistically significant in Group 2 (TFBC). The amount of changes in the upper lip position is more in the TFBC group. The improvement of facial profile is combined with the upper lip retrusion but not with changes in the lower lip position. They state that both lips are supported by the upper incisors, thus significantly participating in the anteroposterior position of the upper lip in particular, while the lower incisors have no significant effect on the position of the lower lip. Similar results have been obtained in the previous study [52] examining the effects of the Herbst appliance in young adults with class II, division 1 malocclusion. Upper incisors retrusion, lower incisor protrusion and forward movement of the lower jaw affect overjet reduction. It is the most important consequence to the correction and straightening of the lower facial third soft tissue.
Changes produced by fixed functional appliances seem to restrict forward movement of the upper lip [53]. A relative surface reduction of the upper lip is the consequence of a number of factors. Most patients targeted for fixed functional appliance therapy have class II malocclusions, hence the reduction in the surface of the upper lip is caused by upper incisors, retrusion as well as maxillary growth inhibition. It also increases due to lower lip forward movement. In a study by Siqueira et al [54], Mandibular advancement by the mandibular protraction appliance (MPA) produces satisfactory results by reducing facial convexity. The treatment effect of this appliance is the correction of malocclusion through mesial displacement of the first mandibular molars, with the consequent protrusion of the lower lip. The lower lip also moves forward because of lower lip position changes.
Similar soft tissue results had also been demonstrated in the comparison of Class II non-extraction treatment primarily by distalizing the maxillary teeth with two-maxillary premolar extractions [35, 40]. The results of this study differ from a previous study [39], that found some differences when comparing soft tissue changes in Class II malocclusion patients treated with the Forsus appliance versus two-maxillary premolar extractions and retraction of the anterior teeth using temporary anchorage devices. However, the mentioned study [39] only evaluated the patients during 14 months, from the insertion of the Forsus appliance or beginning of en masse retractions until removal of the Forsus appliance or completion of en masse retraction. The different results observed could be consequent to the use of temporary anchorage devices and to the smaller observation period of their study.
Skeletal, dental and soft-tissue changes induced by the Jasper Jumper appliance in late adolescence, that uses the E line as a reference line, were not found to produce significant antero-posterior changes of the upper lip [55]. However, statistically significant protrusion of the lower lip was noted which is contrary to the findings observed in the current study.
The results of this study helps in the decision for one of these protocols, considering other variables than changes in the soft tissue profile. Therefore, the decision between Class II malocclusion treatment with Forsus Fatigue Resistant Device or Twin Force Bite Corrector should be based on variables such as patient compliance, mandibular incisors tipping at pre-treatment, cost-benefit ratio, and orthodontist and patient treatment preferences.
Limitations
Despite the inclusion of some patients with initial ¾ Class II molar
relationship , it did not interfere with the results because the
overjet was similar in the groups, it would be ideal to include only patients with complete Class II molar relation . Further studies
with ideal sample compositions are necessary to confirm the current
results.
Acknowledgement and Declarations
Saveetha Dental College and hospitals for the support in doing
the research.
Conclusion
Soft tissue changes of Class II division 1 malocclusion treated
with both the fixed functional appliances associated with fixed
appliances are similar in all the patients.It is the clinician choice
to select the appliance pertaining to the type of patient he is
treating.
Clinical Significance
Since there is a paradigm shift of considering the soft tissue profile
for orthodontic treatment planning, assessing the soft tissue
changes is the new scope of research.Along with these parameters,
the chin throat angle should also be taken into consideration
to consider the soft tissue changes during treatment plan.
References
- Choi JW, Kim N. Clinical application of three-dimensional printing technology in craniofacial plastic surgery. Archives of plastic surgery. 2015 May;42(3):267.Pubmed PMID: 26015880.
- Marconi S, Pugliese L, Botti M, Peri A, Cavazzi E, Latteri S, et al. Value of 3D printing for the comprehension of surgical anatomy. SurgEndosc. 2017 Oct;31(10):4102-4110. PubmedPMID: 28281114.
- Azuma M, Yanagawa T, Ishibashi-Kanno N, Uchida F, Ito T, Yamagata K, et al. Mandibular reconstruction using plates prebent to fit rapid prototyping 3-dimensional printing models ameliorates contour deformity. Head Face Med. 2014 Oct 23;10:45. PubmedPMID: 25338640.
- Patel A, Levine J, Brecht L, Saadeh P, Hirsch DL. Digital technologies in mandibular pathology and reconstruction. Atlas Oral MaxillofacSurgClin North Am. 2012 Mar;20(1):95-106. PubmedPMID: 22365432.
- Sieira Gil R, Roig AM, Obispo CA, Morla A, Pagès CM, Perez JL. Surgical planning and microvascular reconstruction of the mandible with a fibular flap using computer-aided design, rapid prototype modelling, and precontoured titanium reconstruction plates: a prospective study. Br J Oral Maxillofac Surg. 2015 Jan;53(1):49-53. PubmedPMID: 25305795.
- Zimmerer RM, Ellis E 3rd, Aniceto GS, Schramm A, Wagner ME, Grant MP, et al. A prospective multicenter study to compare the precision of posttraumatic internal orbital reconstruction with standard preformed and individualized orbital implants. J Craniomaxillofac Surg. 2016 Sep;44(9):1485- 97. PubmedPMID: 27519662.
- Crafts TD, Ellsperman SE, Wannemuehler TJ, Bellicchi TD, Shipchandler TZ, Mantravadi AV. Three-Dimensional Printing and Its Applications in Otorhinolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg. 2017 Jun;156(6):999-1010. PubmedPMID: 28421875.
- Ledgerwood LG, Chao J, Tollefson TT. Prosthetic reconstruction of complicated auricular defects: use of a hybrid prosthetic fabrication technique. JAMA Facial PlastSurg 2014; 16(2): 153–154.Pubmed PMID:24311116.
- Lichtenstein JT, Zeller AN, Lemound J, Lichtenstein TE, Rana M, Gellrich NC, et al. 3D-Printed Simulation Device for Orbital Surgery. J Surg Educ. 2017 Jan-Feb;74(1):2-8. Pubmed PMID: 27986443.
- Mitsouras D, Liacouras P, Imanzadeh A, Giannopoulos AA, Cai T, Kumamaru KK, et al. Medical 3D printing for the radiologist. Radiographics. 2015 Nov 12;35(7):1965-88.Pubmed PMID:26562233.
- Aldaadaa A, Owji N, Knowles J. Three-dimensional Printing in Maxillofacial Surgery: Hype versus Reality. J Tissue Eng. 2018 Apr 20;9:2041731418770909. PubmedPMID: 29774140.
- Marro A, Bandukwala T, Mak W. Three-dimensional printing and medical imaging: a review of the methods and applications. CurrProblDiagnRadiol 2016; 45(1): 2–9.PubmedPMID: 26298798.
- Rengier F, Mehndiratta A, von Tengg-Kobligk H, Zechmann CM, Unterhinninghofen R, Kauczor HU, et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg. 2010 Jul;5(4):335-41. PubmedPMID: 20467825.
- Frame M, Huntley JS. Rapid prototyping in orthopaedic surgery: a user's guide. ScientificWorldJournal. 2012;2012:838575. PubmedPMID: 22666160.
- Farré-Guasch E, Wolff J, Helder MN, Schulten EA, Forouzanfar T, Klein- Nulend J. Application of Additive Manufacturing in Oral and Maxillofacial Surgery. J Oral Maxillofac Surg. 2015 Dec;73(12):2408-18. PubmedPMID: 25966454.
- Sharif F, Ur Rehman I, Muhammad N, MacNeil S. Dental materials for cleft palate repair. Mater SciEng C Mater Biol Appl. 2016 Apr 1;61:1018-28. PubmedPMID: 26838929.
- Whitcombe MJ, Kirsch N, Nicholls IA. Molecular imprinting science and technology: a survey of the literature for the years 2004-2011. J MolRecognit. 2014 Jun;27(6):297-401. PubmedPMID: 24700625.
- Xie XH, Wang XL, Zhang G, He YX, Leng Y, Tang TT, et al. Biofabrication of a PLGA-TCP-based porous bioactive bone substitute with sustained release of icaritin. J Tissue EngRegen Med. 2015 Aug;9(8):961-72. PubmedPMID: 23255530.
- Pedersen TH, Gysin J, Wegmann A, Osswald M, Ott SR, Theiler L, et al. A randomised, controlled trial evaluating a low cost, 3D-printed bronchoscopy simulator. Anaesthesia. 2017 Aug;72(8):1005-1009. PubmedPMID: 28603907.
- Ionita CN, Mokin M, Varble N, Bednarek DR, Xiang J, Snyder KV, Siddiqui AH, Levy EI, Meng H, Rudin S. Challenges and limitations of patientspecific vascular phantom fabrication using 3D Polyjet printing. InMedical Imaging 2014: Biomedical Applications in Molecular, Structural, and Functional Imaging . International Society for Optics and Photonics.2014 Mar 13 ;9038: 90380M.