Prevalence Of Gingivitis In Patients Undergoing Orthodontic Treatment Of Ages 18-25 Years- A Retrospective Study
Kirtana Gopalasamy1, Jaiganesh Ramamurthy2*, Pradeep D3
1 Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India.
2 Professor and Head, Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
3 Associate Professor, Department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical
Sciences, Saveetha University, Chennai, 600077, India.
*Corresponding Author
Jaiganesh Ramamurthy,
Professor and Head, Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai,
600077, India
Tel: +91 9840443463
E-mail: jaiganeshr@saveetha.com
Received: November 10, 2020; Accepted: December 15, 2020; Published: December 18, 2020
Citation: Kirtana Gopalasamy, Jaiganesh Ramamurthy, Pradeep D. Prevalence Of Gingivitis In Patients Undergoing Orthodontic Treatment Of Ages 18-25 Years- A Retrospective Study. Int J Dentistry Oral Sci. 2020;7(12):1231-1235. doi: dx.doi.org/10.19070/2377-8075-20000243
Copyright: Jaiganesh Ramamurthy©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The use of fixed Orthodontics made of wire and brackets is a common treatment that can affect the gingival health . The constant irritation and poor maintenance in patients may lead to gingival inflammation if not maintained properly .Improper oral hygiene during the course of orthodontic treatment is the leading reason for the cause of gingivitis . 18- 25 years is the most common age where majority of the current population undergo orthodontic treatment for aesthetic look , this makes it an appropriate age of study to see the improper oral hygiene leading to be the cause of gingivitis in many .The purpose of this study was to evaluate the association of orthodontic treatment and gingival health in those patients .Evaluation of 225 patients of age group 18-25 years undergoing Orthodontic treatment in Saveetha Dental College between June 2019 to March 2020 was done and they were also evaluated for the presence of gingivitis . Excel tabulation was done and data was imported to SPSS to generate results From the study we were able to evaluate and see that gingivitis was most often present in patients undergoing orthodontic treatment .Gingival Heath is very important and in patients undergoing orthodontic treatment , due to poor maintenance , presence of plaque increases hence leading to gingivitis.
2.Introduction
3.Material and Methods
4.Statistical Analysis
5.Results
6.Discussion
7.Conclusion
8.Refereces
Keywords
Biofilm; Dental Plaque; Gingiva; Gingivitis; Oral Hygiene; Orthodontic Treatment.
Introduction
Periodontics and Orthodontic treatment interrelationship has
been a subject to a lot of theories and investigation over the last
decade until today, and still remains debatable. Dental and skeletal
malocclusion has over the years shown to affect the gingival and
periodontal health directly and indirectly [1-5]. The main aim of
orthodontic treatment is at the betterment of occlusion inorder
to improve dental health and prolong the health and life of dentition
[6-11]. Orthodontic treatment aims at the betterment of
dental hygiene and this is mainly done by correcting the dental
malocclusion and this helps in reducing the occlusal trauma. Occlusal
trauma when reduced helps in reducing the trauma to the
gingiva and periodontitis and helps in preventing the inflammation.
As the malocclusion is corrected the reduction in crowding
or cross bite or other malocclusion features helps in reducing the
trauma with the patients able to maintain their teeth better and
hence improving dental health [12].
There needs to be maintained a proper balance between health
and disease in the periodontium. This depends on the absence or
presence of supra and sub gingival plaque accumulation. Accumulation
of supra gingival plaque leads to gingivitis [13]. In some
studies, poor oral hygiene increased the occurrence of gingival
enlargement [14, 15]. Other clinical studies concluded that overall
gingival changes during orthodontic treatment are transient with
no permanent damage to the periodontal supporting tissues [16-
21]. The presence of orthodontic brackets and wires directly or
indirectly led to development of gingivitis and periodontitis. It
takes skill and effort to maintain oral hygiene during orthodontic
treatment especially in the interproximal surfaces. Previously
done microbiological studies show that when fixed orthodontic appliances are placed, the potential for quantitative [22, 23] and
qualitative [24, 25] changes in the microbial composition of these
areas increases. Therefore, periodontal inflammation might be
elicited by a change in the microbiological environment.
Plaque composition is greatly dependent on the host and response.
Initial plaque formation is mainly due to the pioneer species
which adhere to the salivary proteins and to the glycoproteins.
The pioneer species include Neisseria, Streptococci predominantly
S.sanguis, Soralis and S.mitis. These initial pioneer species grow
and multiply leading to the secondary colonisation by Gram positive
and negative species creating a biofilm [26].
The role of bacteria in dental caries was proven through experimentation
by match, leading to the formation of white spot lesions.
In a study conducted by [27] he suggested that up to 50%
of the patients who underwent orthodontic treatment developed
white spot lesions during the treatment. In the previous years as
seen in the literature, epidemiological and experimental studies
have shown a strong association between the presence of dental
plaque in the oral cavity leading to the development of gingival
and periodontal diseases [28]. There are mainly two types of periodontal
disease of which, gingivitis is associated with reversible
destruction of the periodontal tissues and periodontitis which is
associated with irreversible pattern of destruction in the form of
periodontal attachment loss [29]. The hypothesis mainly shows us
that the inflammation leads to increased flow of gingival crevicular
fluid which leads to an increase in pH and temperature which
helps in the growth of proteolytic obligate anaerobic species associated
with periodontal diseases [26].
Orthodontic appliances , as well as procedures involving correction
of tooth are Prone to local soft tissue responses in the gingiva.
The close proximity of orthodontic appliances to gingival sulcus
increases the plaque accumulation on improper maintenance
leading to plaque formation [30, 31]. Following the insertion
of orthodontic appliances in the oral cavity it can contribute to
chronic infection, inflammatory hyperplasia, loss of attachment,
gingival recession. Many investigations have shown that gingival
recession to be associated with labial movement of mandibular
incisors and have been associated with risk factors for gingival
recession [32, 33].
The age range of the following study is very important as 18-
25 years is one of the most important phases where a patient
can either choose to maintain their oral health properly or not.
The strong inclination of plaque accumulation in 18-25 years and
towards gingivitis and eventually periodontitis in the later adult
years If not treated properly and looked after now is one of the
important factors in this study.
Gingival overgrowth is a very common condition in the orthodontic
population that is characterised by gingival enlargement
possibly resulting in pseudo-pocketing with or without attachment
loss. When involving the anterior region, it may have an
impact on oral health-related quality of life [34]. The presence
of gingival enlargement in the interdental papillae can be due to
the application of continuous compressive or retraction forces
to correct crowding and spacing. Orthodontic space closure of
extraction sites may result in gingival invagination or growth of
gingival tissue [35, 36].
Mucogingival surgery during orthodontic treatment corrects soft
tissue characteristics in order to create more favourable conditions
for the mechanical stress resistance. Even though improved
gingival characteristics may not guarantee the absence of gingival
recession after orthodontic therapy especially when significant
dental arch expansion or labial proclination is performed and a
second surgery may be needed after the end of orthodontics. Mechanical
forces applied during the course of orthodontic treatment
results in bone changes such as resorption, and changes in
the periodontal ligament and osseous structure. Mild orthodontic
forces along with proper strict oral hygiene may control the bone
changes.
The aim of this study was to evaluate the relationship between
orthodontic treatment and gingivitis in the age group of 18-25
years.
The study was conducted with the approval of the Institutional
Ethics Committee [SDC/SIHEC/2020/DIASDATA/
0619-0320]. The study consisted of one reviewer, one assessor
and one guide.
The study was designed to include all dental patients of the ages
18-25 years undergoing orthodontic treatment. The patients who
did not fall into this inclusion criteria were excluded.
The study was based on a non probability consecutive sampling
method. To minimise sampling bias, all case sheets of patients
who underwent Orthodontic treatment were reviewed and included.
Data Collection was done using the patient database with the
timeframe work 01 June 2019 and 31 march 2020. About 225 case
sheets were reviewed and those fitting under the inclusion criteria
were included. Cross verification was done with the help of Photographs
and radiographic evidence. To minimise sampling bias
all data were included. The exclusion criteria was patients with
systemic illness. Data was downloaded from DIAS and imported
to Excel, Tabulation was done. The values were tabulated and
analysed.
Descriptive statistics were performed using SPSS by IBM on the
tabulated values. Chi-Square test was performed and the p value
was determined to evaluate the significance of the variables it was
used to evaluate the association between the age and gender with
the prevalence of gingivitis in patients undergoing orthodontic
treatment. The results were obtained in the form of graphs and
tables.
Results And Discussion
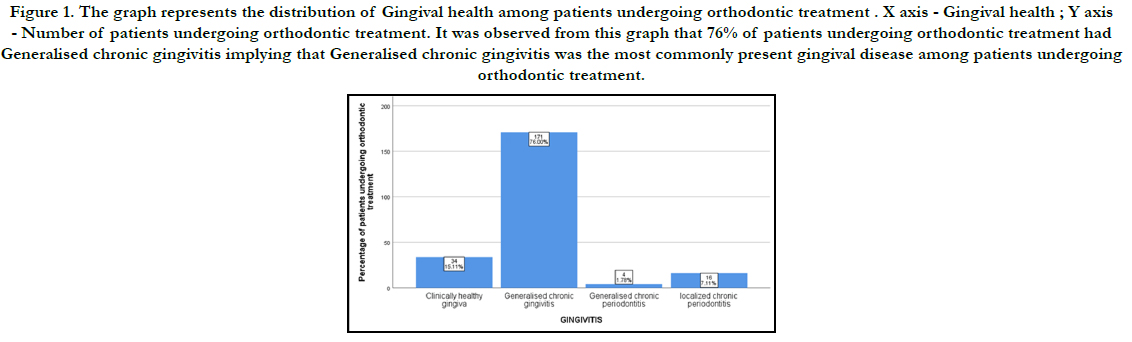
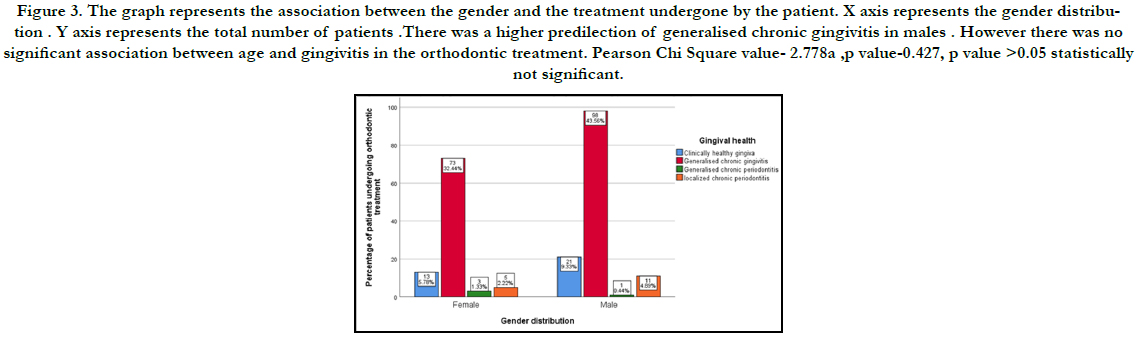
It was seen that out 225 patient that were undergoing orthodontic
treatment, 76% of the patients, had generalised chronic gingivitis,
15% of them had clinically healthy gingiva, 7% of them had
localised chronic periodontitis and 2% of them presented with
generalised chronic periodontitis.
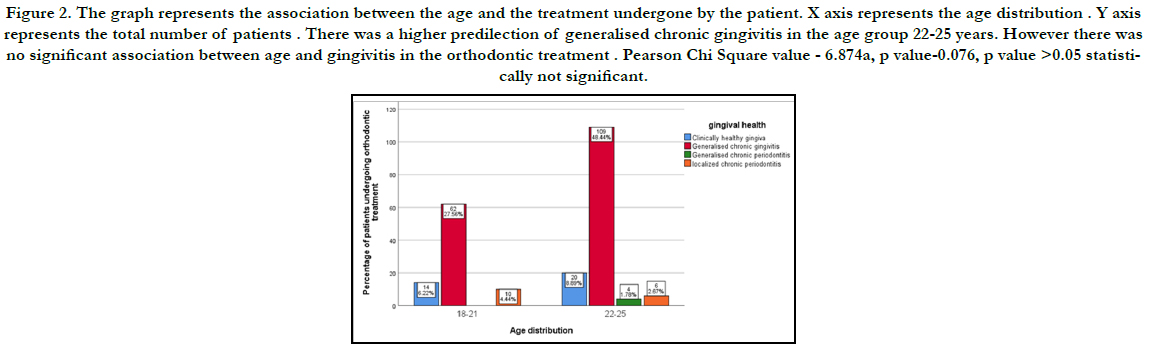
The research also helps us see that on the basis of age, generalised
chronic gingivitis was the most common gingival condition seen
in both the age groups. While localised chronic periodontitis was
high in the age group 22-25 years and generalised chronic periodontitis
was also seen only in the 22-25 years age group.
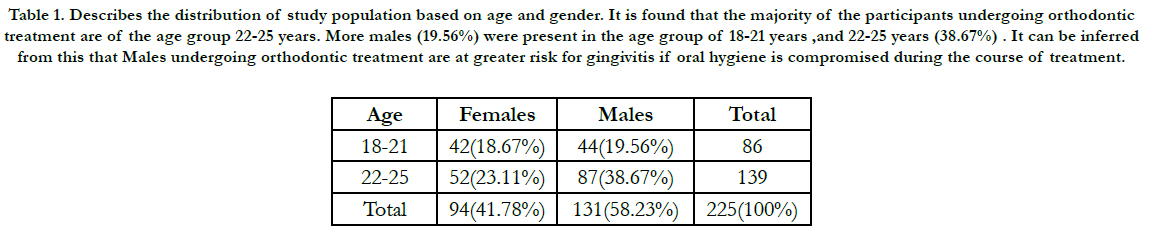
Based on gender wise distribution of gingivitis among patients
undergoing orthodontic treatment, gingivitis was present at a
higher number in males. While in females generalised chronic periodontitis
was seen to be higher in females while localised chronic
periodontitis was seen to be higher in males.
The main reason why orthodontic treatment is done is to improve
facial aesthetics and dental health and function in a review conducted
by Bollen et al., [12], it was seen that there was a correlation
between the presence of a malocclusion and periodontal disease.
Subjects with greater malocclusion have more severe periodontal
disease.The patient’s inability to clean his or her teeth adequately
around fixed orthodontic devices promotes plaque accumulation
that can then lead to gingival inflammation. An overall increase in
salivary bacterial counts, especially Lactobacillus, has been shown
after orthodontic appliance [37] placement. Similarly, one study
showed an early increase in anaerobes and Prevotellaintermedia,
and a decrease in facultative anaerobes [38].
From the study we were also able to see that the lower anterior
region was the area most susceptible for gingival inflammation
and also localised chronic periodontitis in severe cases. They were
statistically significant in patients undergoing orthodontic treatment
. According to a study done by Zachrisson et al ,1972 [39,
40] it was seen that even after maintaining excellent oral hygiene,
patients usually experience Mild to moderate gingivitis within 1-2
months on placing the orthodontic appliance.
Based on another study conflicted by Liu et al, 2011 [41] he suggested
that in patients undergoing orthodontic treatment there
resulted in dental plaque and calculus deposition eventually leading
to gingival inflammation leading to gingivitis and eventually
periodontitis. There being a sufficient increase in the plaque index
and gingival index. Based on another study reported by Davies et
al, 1991 [42] showed the difference in the gingival health in patients
undergoing orthodontic treatment when compared to those
not undergoing orthodontic treatment, and regular visits to the
dentist showed improvement in dental health.
When a comparative evaluation was done orthodontic tooth
movement and gingival recession has been mentioned in both orthodontic
and periodontal literature, with some reports arguing
on behalf of a causal connection and others arguing against it
[43-45]. The age limit in our study was kept at 18 years at the baseline
of orthodontic treatment. In a study conducted by Vassali et
al. [46]. He reported that treatment duration, treatment type, the
skeletal or dental relationship did not affect the development of
recessions during treatment. Presence of gingival inflammation and baseline recession narrow keratinized gingiva [33].
Based on a few studies conducted to evaluate the relationship
between gingival recession and orthodontic treatment, it showed
that gingival recession there was an increase in their prevalence in
older adolescents and adults undergoing orthodontic treatment.
But there was a more favourable outcome in the older age group.
According to a study conducted by Dorfman et al [32]. It was
seen that proclination of the lower incisors during the orthodontic
treatment had a detrimental effect on the periodontal health,
where studies showed that proclined teeth had higher probability
to show gingival inflammation then the untreated teeth.
Oral hygiene instruction and demonstrations must effectively take
place during orthodontic treatment. Certain patients need to be
reminded to concentrate on cleaning the cervical area of their
teeth below the brackets. A continuous increase in oral hygiene
awareness not only will reduce the prevalence and severity of iatrogenic
tissue damage but also will extend the long-term benefits
of orthodontic therapy. From a study conducted by Rajan K et
al [47]. He reported that about 68% of the patients that he assessed
did not visit a dental hygienist during their orthodontic
treatment. Hence this leading to the increase in gingivitis among
patients undergoing orthodontic treatment is negligence to their
oral health. Orthodontic patients, in particular, must be trained in
proper oral hygiene maintenance and their brushing procedures
must be checked regularly.
In a study conducted by Sallum et al. [48], have reported a significant
reduction in plaque index, bleeding on probing, and probing
depth, the three most important parameters indicating clinical
gingival health, once orthodontic appliances are removed. From
our study we were able to see that orthodontic treatment played
an impact in gingival health and plaque accumulation over the
orthodontic appliance is responsible for causing gingival inflammation.
The presence of gingivitis was very common in young
adolescents and adults and the age group 18-25 years. Hence orthodontic
patients should be reinforced to follow strict oral hygiene
protocol to maintain optimal gingival health.
Figure 1. The graph represents the distribution of Gingival health among patients undergoing orthodontic treatment . X axis - Gingival health ; Y axis - Number of patients undergoing orthodontic treatment. It was observed from this graph that 76% of patients undergoing orthodontic treatment had Generalised chronic gingivitis implying that Generalised chronic gingivitis was the most commonly present gingival disease among patients undergoing orthodontic treatment.
Figure 2. The graph represents the association between the age and the treatment undergone by the patient. X axis represents the age distribution . Y axis represents the total number of patients . There was a higher predilection of generalised chronic gingivitis in the age group 22-25 years. However there was no significant association between age and gingivitis in the orthodontic treatment . Pearson Chi Square value - 6.874a, p value-0.076, p value >0.05 statistically not significant.
Figure 3. The graph represents the association between the gender and the treatment undergone by the patient. X axis represents the gender distribution . Y axis represents the total number of patients .There was a higher predilection of generalised chronic gingivitis in males . However there was no significant association between age and gingivitis in the orthodontic treatment. Pearson Chi Square value- 2.778a ,p value-0.427, p value >0.05 statistically not significant.
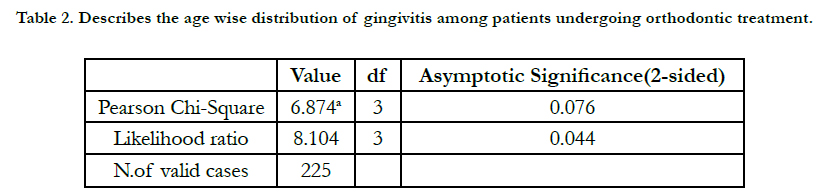
Table 1. Describes the distribution of study population based on age and gender. It is found that the majority of the participants undergoing orthodontic treatment are of the age group 22-25 years. More males (19.56%) were present in the age group of 18-21 years ,and 22-25 years (38.67%) . It can be inferred from this that Males undergoing orthodontic treatment are at greater risk for gingivitis if oral hygiene is compromised during the course of treatment.
Table 2. Describes the age wise distribution of gingivitis among patients undergoing orthodontic treatment.
Conclusion
Within the limits of the present study, it can be concluded that
there was a high prevalence of gingivitis in patients undergoing
orthodontic treatment. We were able to see that gingivitis was
very common in patients undergoing Orthodontic treatment specifically
in the age group of 22-25 years. Considering the relationship
between orthodontic treatment and gingival health, patients
and orthodontists must cooperate and consult with periodontists
during the treatment for a favourable outcome.
Acknowledgement
I would like to thank Saveetha Dental College for the constant
encouragement with my work during all stages.
References
- Thamaraiselvan M, Elavarasu S, Thangakumaran S, Gadagi JS, Arthie T. Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian SocPeriodontol. 2015 Jan-Feb;19(1):66-71. PubmedPMID: 25810596.
- Ramesh A, Varghese SS, Doraiswamy JN, Malaiappan S. Herbs as an antioxidant arsenal for periodontal diseases. J IntercultEthnopharmacol. 2016 Jan 27;5(1):92-6. PubmedPMID: 27069730.
- Varghese SS, Thomas H, Jayakumar ND, Sankari M, Lakshmanan R. Estimation of salivary tumor necrosis factor-alpha in chronic and aggressive periodontitis patients. ContempClin Dent. 2015 Sep;6(Suppl 1):S152-6. PubmedPMID: 26604566.
- Shivakumar K, Chandu G, Shafiulla M. Severity of Malocclusion and Orthodontic Treatment Needs among 12- to 15-Year-Old School Children of Davangere District, Karnataka, India. Eur J Dent. 2010 Jul;4(3):298-307. Pubmed PMID: 20613919.
- Avinash K, Malaippan S, Dooraiswamy JN. Methods of Isolation and Characterization of Stem Cells from Different Regions of Oral Cavity Using Markers: A Systematic Review. Int J Stem Cells. 2017 May 30;10(1):12-20. PubmedPMID: 28531913.
- Panda S, Jayakumar ND, Sankari M, Varghese SS, Kumar DS. Platelet rich fibrin and xenograft in treatment of intrabony defect. ContempClin Dent. 2014 Oct;5(4):550-4. PubmedPMID: 25395778.
- Mootha A, Malaiappan S, Jayakumar ND, Varghese SS, Toby Thomas J. The Effect of Periodontitis on Expression of Interleukin-21: A Systematic Review. Int J Inflam. 2016;2016:3507503. PubmedPMID: 26998377.
- Ravi S, Malaiappan S, Varghese S, Jayakumar ND, Prakasam G. Additive Effect of Plasma Rich in Growth Factors With Guided Tissue Regeneration in Treatment of Intrabony Defects in Patients With Chronic Periodontitis: A Split-Mouth Randomized Controlled Clinical Trial. J Periodontol. 2017 Sep;88(9):839-845. PubmedPMID: 28474968.
- Khalid W, Varghese SS, Sankari M, Jayakumar ND. Comparison of serum levels of endothelin-1 in chronic periodontitis patients before and after treatment. Journal of Clinical and Diagnostic Research: Jcdr. 2017 Apr;11(4):ZC78.
- Khalid W, Vargheese SS, Lakshmanan R, Sankari M, Jayakumar ND. Role of endothelin-1 in periodontal diseases: A structured review. Indian J Dent Res. 2016 May-Jun;27(3):323-33. PubmedPMID: 27411664.
- Boke F, Gazioglu C, Akkaya S, Akkaya M. Relationship between orthodontic treatment and gingival health: A retrospective study. Eur J Dent. 2014 Jul;8(3):373-380. doi: 10.4103/1305-7456.137651. PubmedPMID: 25202219.
- Bollen AM, Cunha-Cruz J, Bakko DW, Huang GJ, Hujoel PP. The effects of orthodontic therapy on periodontal health: a systematic review of controlled evidence. The Journal of the American Dental Association. 2008 Apr 1;139(4):413-22.
- Antoniazzi RP, Miranda LA, Zanatta FB, Islabão AG, Gustafsson A, Chiapinotto GA, Oppermann RV. Periodontal conditions of individuals with Sjögren's syndrome. J Periodontol. 2009 Mar;80(3):429-35. PubmedPMID: 19254127.
- Reali L, Zuliani E, Gabutti L, Schönholzer C, Marone C. Poor oral hygiene enhances gingival overgrowth caused by calcineurin inhibitors. J Clin Pharm Ther. 2009 Jun;34(3):255-60. PubmedPMID: 19646074.
- Somacarrera ML, Lucas M, Scully C, Barrios C. Effectiveness of periodontal treatments on cyclosporine-induced gingival overgrowth in transplant patients. Br Dent J. 1997 Aug 9;183(3):89-94. PubmedPMID: 9282449.
- Ramesh A, Varghese SS, Jayakumar ND, Malaiappan S. Chronic obstructive pulmonary disease and periodontitis–unwinding their linking mechanisms. journal of oral biosciences. 2016 Feb 1;58(1):23-6.
- Kavarthapu A, Thamaraiselvan M. Assessing the variation in course and position of inferior alveolar nerve among south Indian population: A cone beam computed tomographic study. Indian Journal of Dental Research. 2018 Jul 1;29(4):405.
- Ramesh A, Ravi S, Kaarthikeyan G. Comprehensive rehabilitation using dental implants in generalized aggressive periodontitis. J Indian SocPeriodontol. 2017 Mar-Apr;21(2):160-163. PubmedPMID: 29398863.
- Ramesh A, Vellayappan R, Ravi S, Gurumoorthy K. Esthetic lip repositioning: A cosmetic approach for correction of gummy smile - A case series. J Indian SocPeriodontol. 2019 May-Jun;23(3):290g-294. PubmedPMID: 31143013.
- Gomes SC, Varela CC, da Veiga SL, Rösing CK, Oppermann RV. Periodontal conditions in subjects following orthodontic therapy. A preliminary study. Eur J Orthod. 2007 Oct;29(5):477-81. PubmedPMID: 17693428.
- Sadowsky C, BeGole EA. Long-term effects of orthodontic treatment on periodontal health. Am J Orthod. 1981 Aug;80(2):156-72. PubmedPMID: 6943936.
- Diamanti-Kipioti A, Gusberti FA, Lang NP. Clinical and microbiological effects of fixed orthodontic appliances. J ClinPeriodontol. 1987 Jul;14(6):326- 33. J ClinPeriodontol. 1990 Jan;17(1):66.Pubmed PMID: 3509967.
- Paolantonio M, Festa F, di Placido G, D'Attilio M, Catamo G, Piccolomini R. Site-specific subgingival colonization by Actinobacillusactinomycetemcomitans in orthodontic patients. Am J OrthodDentofacialOrthop. 1999 Apr;115(4):423-8. PubmedPMID: 10194288.
- Ristic M, VlahovicSvabic M, Sasic M, Zelic O. Clinical and microbiological effects of fixed orthodontic appliances on periodontal tissues in adolescents. OrthodCraniofac Res. 2007 Nov;10(4):187-95. PubmedPMID: 17973685.
- . Yoo SY, Kim M, Kim S, Kim SH, Ko SJ, Beom JW, et al. Relationship between obesity indices and cardiovascular risk score in Korean type 2 diabetes patients. The Korean Journal of Obesity. 2013 Sep 30;22(3):148-54.
- Marsh P, Martin M. Oral microbiology. Background and introduction. Oral Microbiology 1992; 1–5.
- . Gorelick L, Geiger AM, Gwinnett AJ. Incidence of white spot formation after bonding and banding. American journal of orthodontics. 1982 Feb 1;81(2):93-8.
- Löe H, Theilade E, Börglum Jensen S. Experimental Gingivitis in Man. Journal of Periodontology 1965; 36: 177–187.PubmedPMID: 14296927.
- Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999 Dec;4(1):1-6. PubmedPMID: 10863370.
- Boyd RL. Longitudinal evaluation of a system for self-monitoring plaque control effectiveness in orthodontic patients. J ClinPeriodontol. 1983 Jul;10(4):380-8. PubmedPMID: 6577031.
- Willmot D. Orthodontic treatment and the compromised periodontal patient. Eur J Dent. 2008 Jan;2(1):1-2. PubmedPMID: 19212501.
- Dorfman HS. Mucogingival changes resulting from mandibular incisor tooth movement. Am J Orthod. 1978 Sep;74(3):286-97. PubmedPMID: 281132.
- Hollender L, Rönnerman A, Thilander B. Root resorption, marginal bone support and clinical crown length in orthodontically treated patients. Eur J Orthod. 1980;2(4):197-205. PubmedPMID: 6961039.
- Zanatta FB, Ardenghi TM, Antoniazzi RP, Pinto TM, Rösing CK. Association between gingival bleeding and gingival enlargement and oral healthrelated quality of life (OHRQoL) of subjects under fixed orthodontic treatment: a cross-sectional study. BMC Oral Health. 2012 Nov 27;12:53. PubmedPMID: 23186371.
- Kurol J, Rönnerman A, Heyden G. Long-term gingival conditions after orthodontic closure of extraction sites. Histological and histochemical studies. Eur J Orthod. 1982 May;4(2):87-92. PubmedPMID: 6955180.
- Ramamurthy J. COMPARISON OF EFFECT OF HIORA MOUTHWASH VERSUS CHLORHEXIDINE MOUTHWASH IN GINGIVITIS PATIENTS: A CLINICAL TRIAL. Asian J Pharm Clin Res 2018; 11: 84–88.
- Guilford HJ, Grubb TA, Pence DL. Vertical extrusion: a standardized technique. CompendContinEduc Dent. 1984 Jul-Aug;5(7):562-7.Pubmed PMID: 6590201.
- Melsen B. Tissue reaction following application of extrusive and intrusive forces to teeth in adult monkeys. Am J Orthod. 1986 Jun;89(6):469-75. PubmedPMID: 3459360.
- Zachrisson BU, Zachrisson S. Gingival condition associated with partial orthodontic treatment. ActaOdontol Scand. 1972 Mar;30(1):127-36. PubmedPMID: 4504433.
- Priyanka S, Kaarthikeyan G, Nadathur JD, Mohanraj A, Kavarthapu A. Detection of cytomegalovirus, Epstein-Barr virus, and Torque Teno virus in subgingival and atheromatous plaques of cardiac patients with chronic periodontitis. J Indian SocPeriodontol. 2017 Nov-Dec;21(6):456-460. PubmedPMID: 29551863.
- Liu H, Sun J, Dong Y, Lu H, Zhou H, Hansen BF, et al. Periodontal health and relative quantity of subgingivalPorphyromonasgingivalis during orthodontic treatment. Angle Orthod. 2011 Jul;81(4):609-15. PubmedPMID: 21306224.
- Davies TM, Shaw WC, Worthington HV, Addy M, Dummer P, Kingdon A. The effect of orthodontic treatment on plaque and gingivitis. Am J Orthod- DentofacialOrthop. 1991 Feb;99(2):155-61. Pubmed PMID: 1990825.
- Wennström JL, Lindhe J, Sinclair F, Thilander B. Some periodontal tissue reactions to orthodontic tooth movement in monkeys. J ClinPeriodontol. 1987 Mar;14(3):121-9. PubmedPMID: 3470318.
- Melsen B, Allais D. Factors of importance for the development of dehiscences during labial movement of mandibular incisors: a retrospective study of adult orthodontic patients. Am J OrthodDentofacialOrthop. 2005 May;127(5):552-61. PubmedPMID: 15877035.
- Yared KF, Zenobio EG, Pacheco W. Periodontal status of mandibular central incisors after orthodontic proclination in adults. Am J OrthodDentofacial- Orthop. 2006 Jul;130(1):6.e1-8. PubmedPMID: 16849063.
- Joss-Vassalli I, Grebenstein C, Topouzelis N, Sculean A, Katsaros C. Orthodontic therapy and gingival recession: a systematic review. OrthodCraniofac Res. 2010 Aug;13(3):127-41.Pubmed PMID: 20618715.
- Mahindra RK, Suryawanshi GR, Doshi UH. Effects of fixed orthodontic treatment on gingival health: An observational study.
- Sallum EJ, Nouer DF, Klein MI, Gonçalves RB, Machion L, Wilson Sallum A, et al. Clinical and microbiologic changes after removal of orthodontic appliances. Am J OrthodDentofacialOrthop. 2004 Sep;126(3):363-6. PubmedPMID: 15356501.