The Efficacy of Xenograft Polymerized with Platelet Rich Fibrin Versus Autogenous Graft During the Secondary Alveolar Bone Grafting Of Alveolar Clefts: A Randomized Controlled Clinical Trial
Alaa Alnajjar1, Isam Alkhoury2, Ahmad S Burhan3, Muaaz Alkhouli4*
1 Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Damascus University, Syrian Arab Republic.
2 Professor at Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Damascus University, Syrian Arab Republic.
3 Professor at Department of Orthodontics, Faculty of Dentistry, Damascus University, Syrian Arab Republic.
4 Department of Pediatric Dentistry, Faculty of Dentistry, Damascus University, Syrian Arab Republic.
*Corresponding Author
Muaaz Alkhouli,
MSc, DDS, Department of Pediatric Dentistry, Faculty of Dentistry, Damascus University, Syrian Arab Republic.
Tel: 00963966133383
Fax: 00963966334555
E-mail: muaaz.alkhouli@outlook.com
Received: October 03, 2020; Accepted: October 22, 2020; Published: November 09, 2020
Citation:Alaa Alnajjar, Isam Alkhoury, Ahmad S Burhan, Muaaz Alkhouli. The Efficacy of Xenograft Polymerized with Platelet Rich Fibrin Versus Autogenous Graft During the Secondary Alveolar Bone Grafting Of Alveolar Clefts: A Randomized Controlled Clinical Trial. Int J Dentistry Oral Sci. 2020;7(11):985-990. doi: dx.doi.org/10.19070/2377-8075-20000196
Copyright: Muaaz Alkhouli©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objectives: The aim of this study was to clinically and radiographically compare the effect of two types of secondary alveolar
grafting, xenografts with injectable platelet rich fibrin (I-PRF) and autogenous grafts in patients with alveolar clefts.
Materials and Methods: Twenty patients with unilateral alveolar cleft were divided equally into two groups: Autogenous grafts
group (iliac graft) (6 males, 4 females) with a mean age of 10.5 yrs, and Xenografts polymerized with (I-PRF) group (5 males, 5
females) with a mean age of 9.8 yrs.After six months of grafting, gingival and periodontal clinical examination have been achieved
at the adjacent teeth of the alveolar cleft area for all patients, while bone density was compared radiographically between alveolar
cleft region and intact corresponding region within and between groups using (Cone Beam Computed Tomography) CBCT.
Results: The results showed no statistical differences between both groups either clinically by measuring pocket depth, periodontal
index and gingival index, or radiographically by measuring bonedensity. There was significant difference amongst bone density
means in the grafted alveolar cleft region (425±120 HU) and intact corresponding region (545±125 HU) in the autogenous graft
group. Conversely, there was no statistical significant difference when bone density was compared between both regions in the
second group.
Conclusions: The clinical and radiological success rate of the xenografts polymerized with injectable platelet-rich fibrin (I-PRF)
was similar to that of the autogenous grafts when secondary grafting of the alveolar bone was done.
2.Introduction
3.Material and Methods
4.Results
5.Discussion
6.Conclusion
7.Refereces
Keywords
Autogenous Grafts; Alveolar Clefts; Xenografts; Platelet-Rich Fibrin (Prf).
Introduction
Secondary alveolar bone grafting (SABG) is considered to be an
important comprehensive treatment for cleft lip and palate patientsduring
the mixed dentition stage [1]. SABG has many advantages
likethe stabilization of maxillary dental arch, reaching to
a continuous alveolar process, closing theoronasal fistula, facilitating
the normal eruption of the impacted teeth into the grafted
area, supporting the upper lip, and improving the esthetic appearance
[2, 3].
In 1972, SABG technique was introduced by Boyns and Sends.
Several types of bone grafting have been used in the medical literature
such as: Autogenous bone graft, Allogenic bone graft, and
Xenogeneic bone graft.
The autogenous bone graft is considered thegold standard way of
bone grafting in which the preferred site of donation is iliac crest
bone dueto the sufficient osteoinductive properties and rapid
healing [4, 5]. In fact, the cancellous bone has always seen as one
of the best materials used in the alveolar clefts management [6].
However, there are many shortcomings associated with this type
of bone grafting such as, donor site deterioration, infection, significant
pain, high bone resorption rate, and increased hospitality
time with the possibility of hematoma [7, 8]. These disadvantages
led to search for alternative substances that are biocompatible, resorbable and readily available with bone induction properties [9].
Xenograft refers to a tissue transplanted from one species to another
species, usually derived from bovine or porcine dermis [10].
Bovine grafts are similar in structure to the cancellous bone of
human origin [11]. Furthermore, it is safe and biocompatible with
aboneosteoconductive property [12]. Recently, Choukroun et al
in 2006 mentioned the platelet rich fibrin (PRF) as an effective
method for bone formation in the alveolar cleft patients [13]. The
liquid form of platelet rich fibrin (PRF) is called injectable platelet
rich fibrin (I-PRF). I-PRFincrease the healing properties since it
is richwithleukocytes and platelets. I-PRF can be mixed with bone
graft grains to obtain a sticky bone graft, this sticky bone then
is condensed in the alveolar cleft region where it coagulates and
formed cohesive crystals within few minutes [14].
Several studies reported that I-PRF able to enhance graft stability,
consistency, and integration into thecleft site. as well as it provokes
immune response and reduce the graft rejection possibility
[15]. There are a limited number of studies in the medical literature
compared the autogenous bone graft with the xenogenous
bone graft during secondary alveolar bone grafting. Therefore,
the aim ofthe current study was to evaluate the clinical and radiological
results of secondary alveolar bone grafting using xenograft
polymerized with I-PRF comparing with autologous bone graft in
patients who have alveolar clefts.
This prospective study was a two-arm parallel-group randomized
controlled clinical trial. This study was carried out at the oral and
maxillofacial surgery hospital in Damascus University between
March 2017 and September 2019. Ethical approval was obtained
from the Local Ethics Research Committee at Damascus University
Dental School.
The sample size was estimated using G-power software version
3.1.9.2 (Franz Faul, Universitat Kiel, Germany) as following: the
effect size of bone density was 1.37 [17], study power was 80 %,
the level of significance was 0.05 and the allocation ratio was 1:1.
The required sample size was 10 patients for each group.
Twenty patients who have a unilateral alveolar cleft according to
LAHS classification [16] aged between 9-13 years were recruited
to this study.
Patients with a systemic disease, a contraindication for general
anesthesia, a history of failed alveolar bone grafting, a history of
chemo-therapy or jaw irradiation or poor oral hygiene were excluded.
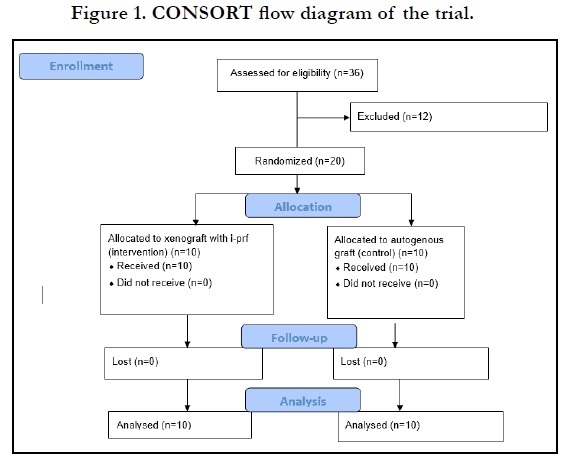
Figure 1 shows the CONSORT flow diagram of the trial.
A pre-surgical orthodontic expansion for the upper dental arch
was occured if needed to prepare the cleft area for bone grafting.
A removable appliance with expansion screw was applied for 3-4
months to obtain 6 to 8 mm of adequate expansion for maxillary
arch which lead to increase in the alveolar cleft width and access
to the surgical field more conveniently [18].
36 patients who have cleft lip and palate were diagnosed and
screened for eligibility primarily, 24 of them met the study inclusion
criteria. The parents of four patients refused to participate in
the current study. Informed consent was obtained for 20 patients.
They were allocated randomly into two parallel groups using software-
generated list of random numbers from the website:www.
randomalists.com. Patients in the first group receivedanautogenous
bone graft from iliac bone. On the other hand,patients in
the second received abovine Xenograft (Bionnovation, Brasil) in
the form of granules polymerized with I-PRF.
The surgical technique for secondary alveolar bone grafting was
performed similarly in both groups by one surgeon under general
anesthesia according to a previous study [19]. In the autogenous
bone graft group, the surgical intervention on the iliac crest was
achieved by a different surgical team to obtain the autologous
bone graft.
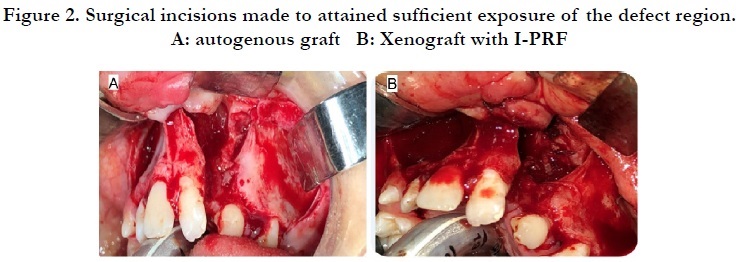
Graft bed or basement preparation was achieved by splitting oral mucosa from nasal mucosa and suturing the nasal layer. Therefore, surgical incisions have been done at the alveolar cleft margins to attained sufficient exposure of the defect region (Fig 2). Vestibular incisions have been completed along gingival margin until first molars region followed by vertical released incision by an obtuse angle toward mucosal vestibule. It is critical to reach periosteum at the bottom of the surgical flap to acquired easy mobilization and coverage of bone graft without tension, and then the flap was elevated from buccal and palatal sides along alveolar cleft edges.
Figure 2. Surgical incisions made to attained sufficient exposure of the defect region. A: autogenous graft B: Xenograft with I-PRF
Bleeding is an important factor to the bone grafted area. Therefore, alveolar bone reshaping by small rounded surgical bur has been used to induce bleeding and allow for the resulting mixture ofthe bone graft and blood to be occurred.
The granular tissues were removed from the cleft area, followed by suturing with released flaps without tension. The graft bed was covered by intact mucoperiosteal flaps on both sides in order to prevent infection or ischemic injury. Suturing began in the nasopalatal mucosal area by Vicryl absorbable sutures – 4/0, followed by labial vestibular mucosa over the grafted areausing the same type of sutures.
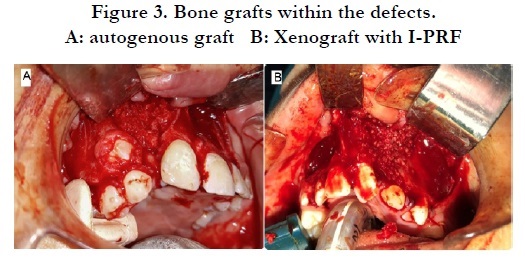
The autogenous bone grafts were placed in the form of chips in the first group (Fig 3), while bovine graft particles were mixed with I-PRF in the second group (Fig 3).
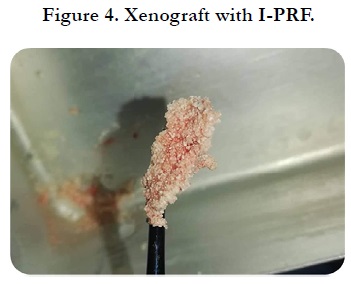
I-PRF was prepared by collecting venous blood by the researchers themselves in 9 ml special-duty tube, followed by centrifuging at 3300 rpm speed for two minutes in a horizontal centrifuge. Blood tubes were placed with water tubes during centrifuging to maintain balance according to previous study [14]. At the end of this process blood materials were observed at the bottom of tube and I-PRF orange material above. Then 5 ml of I-PRF were collected by using 20 ml syringe and mixed with Xenograft in a metal tank for 5 minutes by adding graft particles gradually. Polymerization start within 15 minutes then the material was ready to applied as a bone graft within 20 minutes [14] (Fig 4). Patients were instructed to follow postoperative care guidance, and adhere to liquids based diet for one week.
Concerning patient’s turnaround time (TAT), patients who underwent bovine graft stayed for one day only, while those with iliac crest bone grafts continued their stay in hospital for full three days.
Clinical Evaluation: clinical evaluation was performed by measuring
pocket depth, gingival bleeding, and plaque indices at the
adjacent teeth to the alveolar cleft area [12]. This was done after
six months of the secondary alveolar bone grafting by two
blinded investigators.
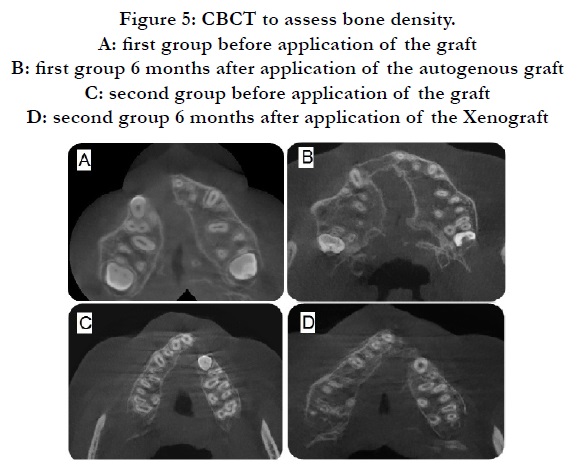
Osseo-density Evaluation: Cone Beam Computed Tomography
CBCT (Vatech, South Korea) was implemented to get the
measure of bone density values in the alveolar cleft region and intact
corresponding region at 99 Kv and 16 mA after 6 months of
secondary bone grafting. bone density was determined by the two
blinded experienced examiners throughout gray values, which
are quantitatively converted into Hounsfield (HU) units [20]. The
axial view was chosen to measure the bone density (Fig 5).
Figure 5: CBCT to assess bone density.
A: first group before application of the graft
B: first group 6 months after application of the autogenous graft
C: second group before application of the graft
D: second group 6 months after application of the Xenograft
Clinical and bone density measurements were repeated three times at different intervals, the average of these measurements was adopted as the final value of the measured variable.
Descriptive statistics were analyzed by measuring means and
standard deviations for bone density values and clinical variables
in both groups. An Independent sample t-Test was used to compare
the mean of bone density and pocket depth in both groups.
While the difference in plaque index and gingival bleeding index
between studied groups was examined by using Chi square test.
Data analysis were performed by using SPSS 20.0 (SPSS, Inc, Chicago,
IL). And set the value of p at (≤0.05) to obtain a statistically
significant test.
Results
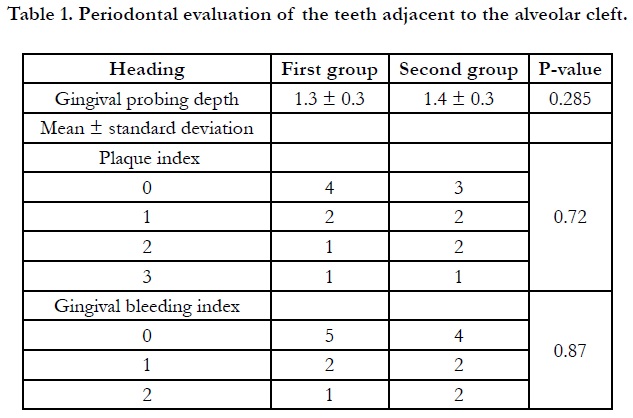
As shown in table 1 the mean value for gingival pockets depth of
the first and second group were 1.3 ± 0.3 and 1.4 ± 0.3 respectively.
By comparing the two groups there was no statistical significant
difference regarding gingival pocket depth, plaque index,
and gingival bleeding index after 6 months of secondary alveolar
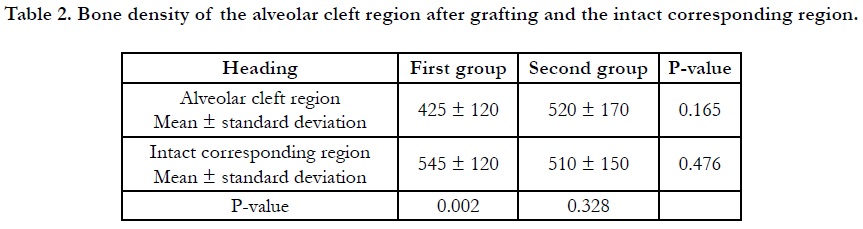
bone grafting. In contrast, table 2 shows the statistical significant
difference regarding bone density values in the first group between
the grafted alveolar cleft region (425 ± 120 HU) and the
intact corresponding area (545 ± 120 HU) with p = 0.002.
Table 2. Bone density of the alveolar cleft region after grafting and the intact corresponding region.
Whilethe second group showed no significant difference in the bone density values when comparing between the grafted alveolar cleft region (520 ± 170HU) and the intact corresponding area (510 ± 150HU). Moreover, no statistically significant differences were depicted in the bone density values in the grafted alveolar cleft regions(p= 0.165) and intact corresponding regions (p=0.476) when comparing between the two groups.
Discussion
Skeletal deformities in the cleft lip and palate patients represented
major challenge for maxillofacial surgeons, because of the various
procedures required to restore normal shape and function of
the oral cavity components. Therefore, secondary alveolar bone
grafting has become a wide popular procedure for restoring occlusal
function in the cleft lip and palate patients. Although, many
articles explored different grafting materials and their application,
there is still a lack of knowledge concerning possible alternatives
to classic grafting materials, hence the importance of this study
as it is the first clinical control study comparing xenografts polymerized
with I-PRF with autologous graft in the alveolar cleft
patients.
Patients were divided into two separate groups autogenous and
xenograft polymerized with I-PRF groups, the use of split mouth
technique was avoided due to heterogenity of right and left sides
in the cleft area for bilateral alveolar cleft patients [21].
Orthodontic expansion were applied for all patients before grafting
in a similar manner to some authors [21]. Orthodontic expansion
provide enough space for graft application and increase graft
absorption rate [23].
Vicryl absorbable sutures were used for closure of the grafting
site as this type of sutures is characterized by low tissue reactivity,
and continuity of the tensile strength for two weeks after surgery
[24].
Cohen's kappa test was used to calculate intra-examiner reproducibility
and inter-examiner reliability for the assessment of test
variables. The kappa for intra-examiner agreement and inter-examiner
reliability was 0.90.
Gingival and periodontal status assessment of the teeth adjacent
to the cleft side is an important factor to confirm oral health
status. Poor oral hygiene promotes infection in the grafting site,
which in turn lead to the bone graft resorption. Thus, clinical
evaluation of the periodontal tissues of the adjacent teeth is studied by measuring amount of pocket depth, gingival bleeding, and
plaque index [25].
Tiny voxel size could be obtained in cone beam computed tomography
(CBCT) which are close to the size of voxel in the computed
tomography (CT) [26], Therefore, it is feasible to obtain an
accuracy in measuring bone density with less radiation exposure.
In addition to that using CBCT is less expansive, more convenient,
and ethically justified [27].
Due, et al. in 2018 concluded that en bloc grafts application in 17
years patients yields satisfactory results as enough bone is provided
to apply dental implants and orthodontic procedures [5]. In
contrast to many studies agreed that using bone grafts in the form
of chips is superior to en bloc corticocancellous grafts. Indeed,
bone chips are easier to osseo-integrate and remodel with the adjacent
bone [28], as indicated in the current study.
Autograft group showed statistically significant difference between
grafted alveolar cleft regionand intact corresponding region.
This is most probably attributed to the autograft’s high absorption
rate, which is in consistent with a previous study [20].
There was no statistically significant difference between alveolar
cleft area and the intact corresponding area in the xenografts polymerized
with I-PRF group; this may be related to the period of
radiographic evaluation. Mich indicated that Xenograft remodeling
in large defects requires 6-9 months [29]. The variance in
this period is related to the size of grafted area; the results of the
present investigation are different with others [12]. Nonetheless,
the outcomes of the current study are in consistent with Zhang’s
study, which evaluated secondary alveolar bone grafting by using
xenografts after six months [30].
Although the bone density value in the xenograft polymerized
with injectable I-PRF group (520 ± 170 HU) was higher than
that in the autogenous group (425 ± 120 HU) in the cleft area,
statistical analysis showed no significance differences between
both groups (P=0.190), which is in agreement with others [12].
Many components such as: bone graft form, dimension, quality,
and fixation affect remodeling process during secondary alveolar
bone grafting. Therefore, the result of this study may related to
the amount of bone loss occurs after autogenous bone grafting.
The limitations of our study are the short period of follow-up
and the small sample size.
Conclusions
Within the limitations of this study, it can be concluded that injectable
I-PRF with Xenograft may show favor in bone formation
than autogenous bone graft. In addition, there are no negative
clinical results when comparing between two types of grafting.
Hence, I-PRF material is preferred for cleft lip and palate correction
during secondary alveolar bone grafting because of its ease
of application and low cost.
References
- Berkowitz S, editor. Cleft lip and palate: diagnosis and management. Springer Science & Business Media; 2006 May 20.
- Cho-Lee GY, García-Díez EM, Nunes RA, Martí-Pagès C, Sieira-Gil R, Rivera-Baró A. Review of secondary alveolar cleft repair. Ann. Maxillofac. Surg. 2013 Jan;3(1):46.
- Nagasao T, Ogata H, Miyamoto J, Jiang H, Kaneko T, Isshiki Y, et al. Alveolar bone grafting for patients with unilateral complete alveolar and palatal clefts improves the bony structure of the nose. Cleft Palate Craniofac J. 2009 Jan;46(1):9-18. Pubmed PMID: 19115796.
- Cobb AR, McCarthy E, Van Zyl M, Ayliffe PR. Alveolar bone grafting: use of the Jacob's chuck with trephine to harvest iliac crest cancellous bone. Br J Oral Maxillofac Surg. 2011 Apr;49(3):239-40. Pubmed PMID: 20546982.
- Du Y, Zhou W, Pan Y, Tang Y, Wan L, Jiang H. Block iliac bone grafting enhances osseous healing of alveolar reconstruction in older cleft patients: A radiological and histological evaluation. Med Oral Patol Oral Cir Bucal. 2018 Mar 1;23(2):e216-e224. Pubmed PMID: 29476672.
- Vandeputte T, Bigorre M, Tramini P, Captier G. Comparison between combined cortical and cancellous bone graft and cancellous bone graft in alveolar cleft: Retrospective study of complications during the first six months postsurgery. J Craniomaxillofac Surg. 2020 Jan;48(1):38-42.Pubmed PMID: 31874807.
- Rawashdeh MA, Telfah H. Secondary alveolar bone grafting: the dilemma of donor site selection and morbidity. Br J Oral Maxillofac Surg. 2008 Dec;46(8):665-70.Pubmed PMID: 18760515.
- Cricchio G, Lundgren S. Donor site morbidity in two different approaches to anterior iliac crest bone harvesting. Clin Implant Dent Relat Res. 2003;5(3):161-9.Pubmed PMID: 14575632.
- da Silva Filho OG, Ozawa TO, Bachega C, Bachega MA. Reconstruction of alveolar cleft with allogenous bone graft: Clinical considerations. Dental Press J Orthod. 2013 Nov-Dec;18(6):138-47.Pubmed PMID: 24351162.
- Sohn HS, Oh JK. Review of bone graft and bone substitutes with an emphasis on fracture surgeries. Biomater Res. 2019 Mar 14;23(1):9.Pubmed PMID: 30915231.
- Temmerman A, Cortellini S, Van Dessel J, De Greef A, Jacobs R, Dhondt R, et al. Bovine-derived xenograft in combination with autogenous bone chips versus xenograft alone for the augmentation of bony dehiscences around oral implants: A randomized, controlled, split-mouth clinical trial. J Clin Periodontol. 2020 Jan;47(1):110-119.Pubmed PMID: 31602699.
- Benlidayi ME, Tatli U, Kurkcu M, Uzel A, Oztunc H. Comparison of bovine-derived hydroxyapatite and autogenous bone for secondary alveolar bone grafting in patients with alveolar clefts. J Oral Maxillofac Surg. 2012 Jan;70(1):e95-e102.Pubmed PMID: 22182665.
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Mar;101(3):e37-44. Pubmed PMID: 16504849.
- Mourão CF, Valiense H, Melo ER, Mourão NB, Maia MD. Obtention of injectable platelets rich-fibrin (i-PRF) and its polymerization with bone graft: technical note. Rev Col Bras Cir. 2015 Nov-Dec;42(6):421-3.Pubmed PMID: 26814997.
- Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, et al. Advanced platelet-rich fibrin: a new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implantol. 2014 Dec;40(6):679-89. Pubmed PMID: 24945603.
- Koch Koch J, Koch H, Grzonka M, Gundlach KK. Facial clefts and their coding with LAHS nomenclature.MKG. 2003 Oct 14;7(6):339-44.
- Canan Jr LW, da Silva Freitas R, Alonso N, Tanikawa DY, Rocha DL, Coelho JC. Human bone morphogenetic protein-2 use for maxillary reconstruction in cleft lip and palate patients. J. Craniofac. Surg. 2012 Nov 1;23(6):1627- 33.
- Uzel A, Benlidayı ME, Kürkçü M, Kesiktaş E. The Effects of Maxillary Expansion on Late Alveolar Bone Grafting in Patients With Unilateral Cleft Lip and Palate. J Oral Maxillofac Surg. 2019 Mar;77(3):607-614.Pubmed PMID: 30138625.
- Mossaad A, El Badry T, Abdelrahaman M, Abdelazim A, Ghanem W, Hassan S, et al. Alveolar cleft reconstruction using different grafting techniques. Open Access Maced. J. Med. Sci. 2019 Apr 30;7(8):1369.
- De Mulder D, Cadenas de Llano-Pérula M, Jacobs R, Verdonck A, Willems G. Three-dimensional radiological evaluation of secondary alveolar bone grafting in cleft lip and palate patients: a systematic review. Dentomaxillofac Radiol. 2018 Jul 20;48(1):20180047. Pubmed PMID: 29947253.
- Zheng W, Li B, Zou Y, Lou F. The prenatal diagnosis and classification of cleft palate: the role and value of magnetic resonance imaging. Eur Radiol. 2019 Oct;29(10):5600-5606.Pubmed PMID: 30887208.
- de Ruiter A, van der Bilt A, Gert M, Ronald K. Orthodontie Treatment Results following Grafting Autologous Mandibular Bone to the Alveolar Cleft in Patients with a Complete Unilateral Cleft. Cleft Palate Craniofac. J. 2010 Jan;47(1):35-42. h
- Khalifa ME, Gomaa NE. Dental arch expansion after alveolar cleft repair using autogenous bone marrow derived mesenchymal stem cells versus autogenous chin bone graft. Egypt Dent J. 2018;64:107-18.
- Yaltirik M, Dedeoglu K, Bilgic B, Koray M, Ersev H, Issever H, et al. Comparison of four different suture materials in soft tissues of rats. Oral Dis. 2003 Nov;9(6):284-6.Pubmed PMID: 14629327.
- Teja Teja Z, Persson R, Omnell ML. Periodontal status of teeth adjacent to nongrafted unilateral alveolar clefts. Cleft Palate Craniofac J. 1992 Jul;29(4):357-62.Pubmed PMID: 1643067.
- Lee S, Gantes B, Riggs M, Crigger M. Bone density assessments of dental implant sites: 3. Bone quality evaluation during osteotomy and implant placement. Int J Oral Maxillofac Implants. 2007 Mar-Apr;22(2):208-12. Pubmed PMID: 17465345.
- Krishnan V. Cone beam computed tomography–A risk-benefit analysis!. J. World Fed. Orthod. 2019 Dec 1;8(4):129-30.
- Alonso N, da Silva Freitas R, Amundson J, Raposo-Amaral CE. Bone Graft in Alveolar Cleft Lip and Palate. Cleft Lip and Palate Treatment: Springer. 2018. 247-61.
- Misch CE, Misch-Dietsh F. Keys to bone grafting and bone grafting materials. Contemporary implant dentistry. St. Louis: Mosby Elsevier. 2008:839- 68.
- Zhang W, Shen G, Wang X, Yu H, Fan L. Evaluation of alveolar bone grafting using limited cone beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012 Apr 1;113(4):542-8.