Assessment Of Periodontal Status among Post Menopausal Women: A Retrospective Study
Trishala Rajan1, Arvina Rajasekar2*, Arvina Rajasekar3
1 Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India.
2 Senior Lecturer, Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
3 Senior Lecturer, Department of Public Health Dentistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
*Corresponding Author
Arvina Rajasekar,
Senior Lecturer, Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077,
India.
Tel: +919486442309
E-mail: arvinar.sdc@saveetha.com
Received: October 07, 2020; Accepted: November 22, 2020; Published: November 25, 2020
Citation:Trishala Rajan, Arvina Rajasekar, Arvina Rajasekar. Assessment Of Periodontal Status among Post Menopausal Women: A Retrospective Study. Int J Dentistry Oral Sci. 2020;7(11):1063-1066. doi: dx.doi.org/10.19070/2377-8075-20000210
Copyright: Arvina Rajasekar© 2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Periodontitis is defined as an inflammatory disease of the supporting tissues of the teeth. Menopause has been associated with
destructive periodontal disease in older women. The aim of this study was to assess the periodontal status among post menopausal
women. A retrospective study was conducted among patients in a private institution in Chennai from June 2019 - March 2020. A
total of 4341 postmenopausal patients were recruited. Data regarding the periodontal status of the patients were collected from
their case records. Descriptive statistics and inferential statistics were done using SPSS software. The present study showed that
among the study population, 20.3% had periodontitis, 71.61% had gingivitis and 8.04% had clinically healthy gingiva. There was a
higher prevalence of periodontitis among post menopausal women between 45 to 60 years of age (15.8%), followed by patients
between 60 to 75 years of age (3.92%) and the least among patients between 75 to 90 years of age (0.58%). Also there was a statistically
significant association between different age groups of post menopausal women and the periodontal status.
2.Introduction
3.Materials and Method
4.Results and Discussion
5.Conclusion
6.Acknowledgement
7.References
Keywords
Age; Menopause; Oral health; Periodontitis.
Introduction
The health of the oral cavity can have wide reaching effects on
overall health. Poor oral health may occur concomitantly with a
more serious underlying disease process or may predispose an individual
to other health conditions [1]. Protecting oral health is
therefore critical in maintaining overall health [2].
Periodontitis is defined as an inflammatory disease of supporting
tissues of the teeth caused by specific microorganisms, resulting
in progressive destruction of the periodontal ligament and alveolar
bone with periodontal pocket formation, gingival recession or
both [3]. Almost all forms of periodontal disease occur as a result
of mixed microbial infections within which specific groups of
pathogenic bacteria coexist [4]. Various risk factors are associated
with periodontal disease which can be either modifiable and non
modifiable [5]. These include microorganisms, tobacco smoking,
diabetes mellitus, cardiovascular disease, drug-induced disorders,
stress, obesity, hematological disorders, host response, pregnancy,
female hormonal alterations and osteoporosis [6]. Among these,
sex hormones have been suggested as important modifying factors
that may influence the pathogenesis of periodontal diseases
[7]. Hormones are specific regulatory molecules that modulate
reproduction, growth and development, maintenance of the internal
environment, as well as energy production, utilization and
storage [8]. The variation in the level of female sex hormones
estrogen and progesterone are responsible for various physiological
changes in females at specific phases of their life [9]. These
changes not only affect other parts of the body, but also have
significant influence on oral tissues as the receptors for estrogen
and progesterone have been demonstrated in the gingiva, on the
periosteal fibers, scattered fibroblasts of the lamina propria and
also on periodontal ligament fibroblasts and osteoblasts proving
the direct action of sex hormones on periodontal tissues [10].
Peak ovarian function occurs before age 30 and then declines gradually. The initial sign of the transition, which may begin in
the forties, is a reduction in menstrual flow which is followed by
missed periods [11]. Menopause is defined as the permanent cessation
of menstruation due to the loss of ovarian follicular function,
and usually takes place between 45 and 55 years of age, and
has also been associated with destructive periodontal disease in
older women [12].
Changes in progesterone level may change vascular permeability
and then result in gingival swelling and inflammation and reduced
resistance to dental plaque (i.e. bacteria). While changes in estrogen
hormone level can cause alteration in immune function and
and changes in microflora of the mouth.Women's oral health has
become an international focus, as it is an integral part of general
health [8].
Previously our team had conducted various studies on treatment
modalities for periodontal diseases and periodontal procedures
[13-22], studies correlating various diseases and factors related to
periodontal diseases [23-25] and in-vitro & radiological studies [26,
27] over the past five years. Now we are focussing on epidemiological
studies. Therefore, the aim of this study was to assess the
periodontal status among postmenopausal women.
Materials and Methods
A retrospective study was conducted to find out the prevalence
of periodontitis among post menopausal women visiting a private
institution between June 2019 to March 2020. Prior permission to
utilize the data for the study and analysis was obtained from the
Institutional Research Committee of the University under ethical
approval number SDC/SIHEC/2020/DIASDATA/0619-0320.
A total of 4341 post menopausal patients were recruited. Patients
with systemic diseases, patients under long term medications were
excluded from the study. Data regarding the periodontal status of
the patients were collected from their case records. Descriptive
(frequency distribution and percentage) and inferential statistics
(chi-square test) were done using SPSS software.
Results and Discussion
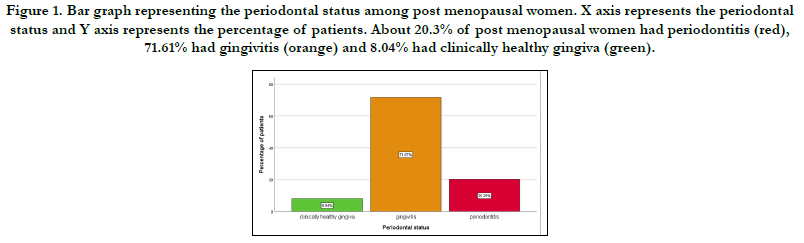
A total of 4341 post menopausal patients were recruited in the
present study. Among the study population, 20.3% had periodontitis,
71.61% had gingivitis and 8.04% had clinically healthy gingiva
(Figure 1).
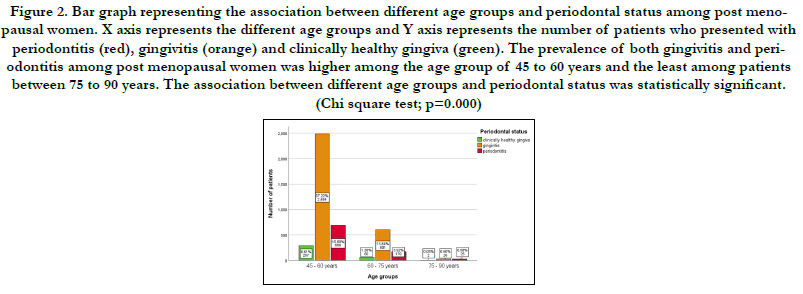
The mean age of the patients was 54.31 ± 7.77 years. The study
participants were divided based on their age as follows: 45 to 60
years, 60 to 75 years, 75 to 90 years. About 15.8% of patients
between 45 to 60 years, 3.92% of patients between 60 to 75 years
and 0.58% of patients between 75 to 90 years presented with
periodontitis. The prevalence of both gingivitis and periodontitis
among post menopausal women was higher among the age group
of 45 to 60 years and the least among patients between 75 to
90 years. The association between different age groups and periodontal
status of post menopausal women was assessed by chisquare
test and was found to be statistically significant with the p
value of 0.000 [Figure 2].
Figure 1. Bar graph representing the periodontal status among post menopausal women. X axis represents the periodontal status and Y axis represents the percentage of patients. About 20.3% of post menopausal women had periodontitis (red), 71.61% had gingivitis (orange) and 8.04% had clinically healthy gingiva (green).
Figure 2. Bar graph representing the association between different age groups and periodontal status among post menopausal women. X axis represents the different age groups and Y axis represents the number of patients who presented with periodontitis (red), gingivitis (orange) and clinically healthy gingiva (green). The prevalence of both gingivitis and periodontitis among post menopausal women was higher among the age group of 45 to 60 years and the least among patients between 75 to 90 years. The association between different age groups and periodontal status was statistically significant. (Chi square test; p=0.000)
This study aims to create an awareness about the severity of periodontitis especially in post menopausal women and to elucidate the importance of proper oral hygiene practices so as to prevent further progression of periodontal disease.
In the present study, the overall prevalence of periodontitis among post menopausal women was 20.3%, which is relatively low, the prevalence of gingivitis was 71.67% and the prevalence of patients with clinically healthy gingiva was 8.04%. This is in accordance with a study by Hossain et al, where in Saudi Arabian population, 71.9% postmenopausal patients were found suffering from gingivitis and 29.1% had periodontitis [28]. Alves C et al compared the periodontal status of premenopausal women with postmenopausal women and concluded that menopause does not significantly influence the severity of periodontal diseases or tooth loss. Factors other than menopause may exert a greater influence on periodontal disease severity [29]. In another study by Alves C et al, it was concluded that there is no relationship between tooth loss and periodontal disease in post menopausal women [30]. Contrastingly in a study by Sharath K.S et al, 67.8% of post menopausal women had periodontitis in the Dakshina Kannada population [31].
There was a higher prevalence of periodontitis among post menopausal women between 45 to 60 years of age in this study. This is comparable to a study by Suresh et al, where in Indian women, there is an increased incidence of periodontitis between the ages of 45 and 55 [32]. Wulandari et al, stated that there was a higher prevalence of periodontitis in post menopausal women above 45 years of age [33]. Understanding age-related factors at menopause is important because early menopause can increase risk factors for diseases associated with estrogen deficiency, such as periodontitis and osteoporosis.
There are several restrictions to the present study which includes the sample size and geographic limitation of study population. Thus, these results cannot be generalised to other populations of geographic and cultural variation.
Conclusion
Within the limitations of the present study, it can be concluded
that among the study population, 20.3% had periodontitis,
71.61% had gingivitis and 8.04% had clinically healthy gingiva.
Also, the prevalence of both gingivitis and periodontitis among
post menopausal women was higher among the age group of 45
to 60 years.
Acknowledgements
The authors of this study would like to express their gratitude
towards everyone who facilitated and enabled us to carry out this
study successfully. We would also thank the institute for helping
us to have access to all the case records for collecting the required
cases for conducting this study.
Authors Contribution
Trishala Rajan performed the analysis, interpretation and drafted
the manuscript. Arvina Rajasekar contributed to conception, data
design, analysis, interpretation and critically revised the manuscript.
Arthi Balasubramaniam participated in the study and revised
the manuscript. All the three authors equally contributed to
the manuscript.
References
- Page RC, Kornman KS. The pathogenesis of human periodontitis: an introduction. Periodontol. 2000. 1997 Jun;14(1):9-11.
- Flemmig TF. Periodontitis. Annals of Periodontology. 1999 Dec;4(1):32-8.
- Van Dyke TE, Dave S. Risk factors for periodontitis. J Int Acad Periodontol. 2005 Jan;7(1):3-7.
- Li Y, Lee S, Hujoel P, Su M, Zhang W, Kim J, et al. Prevalence and severity of gingivitis in American adults. Am J Dent. 2010 Feb;23(1):9-13.Pubmed PMID: 20437720.
- Ostberg AL, Halling A, Lindblad U. Gender differences in knowledge, attitude, behavior and perceived oral health among adolescents. Acta Odontol Scand. 1999 Aug;57(4):231-6.Pubmed PMID: 10540935.
- AlJehani YA. Risk factors of periodontal disease: review of the literature. Int. J. Dent. 2014 May 20;2014:1-9.
- Salvi GE, Lawrence HP, Offenbacher S, Beck JD. Influence of risk factors on the pathogenesis of periodontitis. Periodontology 2000. 1997 Jun;14(1):173-201.
- Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol. 1999 Dec;4(1):1-6.
- Deepa D. Influences of estrogen and progesterone on periodontium - A review [Internet]. CODS Journal of Dentistry. 2014;6: 26–9. Available from: http://dx.doi.org/10.5005/cods-6-1-26
- Güncü NG, Tözüm TF. The effects of estrogen, progesterone and testosterone on periodontal tissues. J Gazi University Faculty of Dentistry. 2005;22:121-7.
- Dutt P, Chaudhary S, Kumar P. Oral health and menopause: a comprehensive review on current knowledge and associated dental management. Ann Med Health Sci Res. 2013 Jul;3(3):320-3.Pubmed PMID: 24116306.
- Hariri R, Alzoubi EE. Oral manifestations of menopause. J Dent Health Oral Disord Ther. 2017;7(4):1-4.
- Panda S, Jayakumar ND, Sankari M, Varghese SS, Kumar DS. Platelet rich fibrin and xenograft in treatment of intrabony defect. Contemp Clin Dent. 2014 Oct;5(4):550-4.Pubmed PMID: 25395778.
- Thamaraiselvan M, Elavarasu S, Thangakumaran S, Gadagi JS, Arthie T. Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian Soc Periodontol. 2015 Jan;19(1):66-71.
- Varghese SS, Thomas H, Jayakumar ND, Sankari M, Lakshmanan R. Estimation of salivary tumor necrosis factor-alpha in chronic and aggressive periodontitis patients. Contemp Clin Dent. 2015 Sep;6(Suppl 1):S152-6. Pubmed PMID: 26604566.
- Mootha A, Malaiappan S, Jayakumar ND, Varghese SS, Toby Thomas J. The Effect of Periodontitis on Expression of Interleukin-21: A Systematic Review. Int J Inflam. 2016;2016:3507503.Pubmed PMID: 26998377.
- Ramesh A, Varghese SS, Doraiswamy JN, Malaiappan S. Herbs as an antioxidant arsenal for periodontal diseases. J Intercult Ethnopharmacol. 2016 Jan 27;5(1):92-6.Pubmed PMID: 27069730.
- Kavarthapu A, Thamaraiselvan M. Assessing the variation in course and position of inferior alveolar nerve among south Indian population: A cone beam computed tomographic study. Indian J Dent Res. 2018 Jul- Aug;29(4):405-409.Pubmed PMID: 30127186.
- Ramesh A, Ravi S, Kaarthikeyan G. Comprehensive rehabilitation using dental implants in generalized aggressive periodontitis. J Indian Soc Periodontol. 2017 Mar-Apr;21(2):160-163.Pubmed PMID: 29398863.
- Ravi S, Malaiappan S, Varghese S, Jayakumar ND, Prakasam G. Additive Effect of Plasma Rich in Growth Factors With Guided Tissue Regeneration in Treatment of Intrabony Defects in Patients With Chronic Periodontitis: A Split-Mouth Randomized Controlled Clinical Trial. J Periodontol. 2017 Sep;88(9):839-845.Pubmed PMID: 28474968.
- RAMAMURTHY J. COMPARISON OF EFFECT OF HIORA MOUTHWASH VERSUS CHLORHEXIDINE MOUTHWASH IN GINGIVITIS PATIENTS: A CLINICAL TRIAL. Asian J Pharm Clin Res. 2018;11(7):84- 8.
- Ramesh A, Vellayappan R, Ravi S, Gurumoorthy K. Esthetic lip repositioning: A cosmetic approach for correction of gummy smile - A case series. J Indian Soc Periodontol. 2019 May-Jun;23(3):290-294.Pubmed PMID: 31143013.
- Khalid W, Vargheese SS, Lakshmanan R, Sankari M, Jayakumar ND. Role of endothelin-1 in periodontal diseases: A structured review. Indian J Dent Res. 2016 May-Jun;27(3):323-33.Pubmed PMID: 27411664.
- Ramesh A, Varghese SS, Jayakumar ND, Malaiappan S. Chronic obstructive pulmonary disease and periodontitis–unwinding their linking mechanisms. J. Oral Biosci. 2016 Feb 1;58(1):23-6.
- Avinash K, Malaippan S, Dooraiswamy JN. Methods of Isolation and Characterization of Stem Cells from Different Regions of Oral Cavity Using Markers: A Systematic Review. Int J Stem Cells. 2017 May 30;10(1):12-20. Pubmed PMID: 28531913.
- Khalid W, Varghese SS, Sankari M, Jayakumar ND. Comparison of Serum Levels of Endothelin-1 in Chronic Periodontitis Patients Before and After Treatment. J Clin Diagn Res. 2017 Apr;11(4):ZC78-ZC81.Pubmed PMID: 28571268.
- Priyanka S, Kaarthikeyan G, Nadathur JD, Mohanraj A, Kavarthapu A. Detection of cytomegalovirus, Epstein-Barr virus, and Torque Teno virus in subgingival and atheromatous plaques of cardiac patients with chronic periodontitis. J Indian Soc Periodontol. 2017 Nov-Dec;21(6):456-460.Pubmed PMID: 29551863.
- Hossain MZ, Fageeh HN, Elagib MF. Prevalence of periodontal diseases among patients attending the outpatient department at the college of dentistry, King Khalid University, Abha, Saudi Arabia. City Dent. Coll. j. 2018;10(1):9-12.
- Alves RC, Félix SA, Rodriguez-Archilla A, Oliveira P, Brito J, Dos Santos JM. Relationship between menopause and periodontal disease: a crosssectional study in a Portuguese population. Int J Clin Exp Med. 2015 Jul 15;8(7):11412-9.Pubmed PMID: 26379957.
- Alves RC, Castro Alves R, Félix SA, Archilla AR. Is menopause associated with an increased risk of tooth loss in patients with periodontitis? [Internet]. Revista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial. 2013;54: 210–6.
- Sharath KS, Singhal R, Thomas B. Prevalence of Periodontitis in Post-Menopausal Women in Rural Dakshina Kannada. PUBLIC HEALTH. 2011 Jul 1;2011(17 SUPPL II).
- Suresh S, Kumar TS, Saraswathy PK, Pani Shankar KH. Periodontitis and bone mineral density among pre and post menopausal women: A comparative study. J Indian Soc Periodontol. 2010 Jan;14(1):30-4.Pubmed PMID: 20922076.
- Wulandari P, Masulili SL, Tadjoedin FM, Kemal Y, Kusdhany LS. The Relationship Between Estrogen Levels and Periodontal Status in Postmenopausal Women. J. Int. Dent. Medical Res. 2017;10:657-62.