Effects of Probiotics on Clinical Appearance of Oral Mucositis in Children with Leukemia during Chemotherapy
Hans Christian1, Margaretha Suharsini2*, Eva Fauziah3
1 Postgraduate Program, Department of Pediatric Dentistry, Faculty of Dentistry, Universitas Indonesia, Jakarta 10430, Indonesia.
2 Professor, Lecturer, Department of Pediatric Dentistry, Faculty of Dentistry, Universitas Indonesia, Jakarta 10430, Indonesia.
3 Lecturer, Department of Pediatric Dentistry, Faculty of Dentistry, Universitas Indonesia, Jakarta 10430, Indonesia.
*Corresponding Author
Margaretha Suharsini D.D.S.,PhD.,
Professor, Lecturer, Department of Pediatric Dentistry, Faculty of Dentistry, Universitas Indonesia, Jakarta 10430, Indonesia.
Tel: +6281 314560000
E-mail: m_suharsini@ui.ac.id
Received: October 13, 2020; Accepted: November 18, 2020; Published: November 24, 2020
Citation:Hans Christian, Margaretha Suharsini, Eva Fauziah. Effects of Probiotics on Clinical Appearance of Oral Mucositis in Children with Leukemia during Chemotherapy. Int J Dentistry Oral Sci. 2020;7(11):1032-1036. doi: dx.doi.org/10.19070/2377-8075-20000204
Copyright: Margaretha Suharsini©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Mucositis is one of the side effects induced by chemotherapy. It results in pain, discomfort, difficulties in talking,
swallowing, eating, drinking, poor nutrition, systemic weakness and life-threatening infections. Probiotics contain nonpathogenic
live microorganisms that give benefit to our health and help in preventing inflammation in the oral cavity. Several studies have
reported the use of probiotics for oral health purposes.
Objectives: The aim of this study was to analyze the effect of probiotic to oral mucositis in children with hematology cancer that
underwent the chemotherapy process before gargling, 7 days after gargling, and 14 days after gargling with probiotic.
Materials and Methods: The study was held in National Cancer Hospital. Eleven patients were meet the criteria. One day after
the chemotherapy started, the researcher checked the patient’s oral health condition using Oral Assessment Guide (OAG). Then
the patient started to gargle the probiotic twice a day for 7 days and the researcher rechecked the score of oral mucositis after 7
days and 14 days.
Results: There was a significance decreasing OAG score between before gargling with 7 days and 14 days after gargling probiotics.
Conclusions: Probiotics gave effects in children with leukemia during chemotherapy and could be an alternative therapy for oral mucositis.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.Conclusion
7.Acknowledgement and Declarations
8.Refereces
Keywords
Chemotherapy; Children; Leukemia; Oral Assessment Guide; Oral Mucositis; Probiotic.
Introduction
Hematologic cancer is the most common types of cancer that
is found in children and the treatment option is chemotherapy.
One of the unexpected complication and mostly seen due to
chemotherapy is oral mucositis, start from the inflammation and
ulcerated in oral mucous then cause the pain, uncomfortable and
systemic weakness [1-4]. Eighty percent of children that have
chemotherapy will get various levels of mucositis, depends on the
types of cancer and medical treatment [5]. Children with hematologic
malignancies have the mucositis more often than children
with tumor, and they who have the chemotherapy are more frequently
to get mucositis than adults, mostly seen in 90% of children
below than 12 years [6, 7].
Oral mucous is easily broken because of chemotherapy. Inflammation
in oral mucous can cause pain, infected ulceration and
disability to eat, drink, even swallow. There are many assessment
scale that can be used to evaluate the oral mucositis. Each of
them use the same criteria but has different levels, so it is hard to
compare the accuracy of study result [5]. Oral Assessment Guide
(OAG) can be trusted and legal, it can be used and sensitive with
the changing condition [8]. OAG scores mucous in 8 different
area to see the extension of mucositis better than the other scoring
method, and according to some researchers, OAG is easily
used, especially for children [5]. Saliva is a complex media in the
oral cavity that contains various bactericidal, bacteriostatic and inhibitor
protein, which if they were combined, will destroy some
plankton species. Probiotics that are swallowed will expose with
the saliva protein and effect to adhesion, morphology, metabolism
activity and viability of probiotic microorganism. After the
adhesion with oral cavity, probiotic helps in preventing inflammation in the oral cavity and oral tissue destruction because of
the oral pathogen. Probiotics also activate and regulate immune
system [9].
Based on the study, oral mucositis is one of the most common
condition seen in children with cancer who take chemotherapy
and weakening them, it is found in 52-80% children that are being
treated [10, 11]. Oral mucositis causes inflammation and ulcer in
oral cavity, begin with tissue depletion in the oral, erythema then
become ulcer [6, 12]. Usually probiotics study is in digestive system
and there is a new study about the benefit of probiotic in oral
health, by manipulating oral microflora that significantly reduce
the inflammation in the oral [13]. Probiotics containing Lactobacillus
spp. are known as an effective new pharmacotherapy in
intervene mucositis [14]. Based on this information, researcher
interested to study about the effect of probiotics to oral mucositis
in children with cancer who are having chemotherapy. The aim of
this study was to analyze the effect of probiotic to oral mucositis
in children with hematology cancer who underwent the chemotherapy
process before gargling, 7 days after gargling, and 14 days
after gargling with probiotic.
Materials and Methods
The research project was approved by the Dental Research Ethics
Committee. Clinical experimental study was performed to evaluate
the clinical appearance of oral mucositis. The subjects were
children patients in National Cancer Hospital that were having
chemotherapy and agreed to take part in this study. The children
were diagnosed by the pediatrician and having chemotherapy in
induction and consolidation phase, also they had to be able to follow
instructions for gargling.
Measurement of oral mucositis had to be determined clinically in
children. The instrument that was used to assess oral mucositis
had a standard. In this study, the researcher used Oral Assessment
Guide to control the oral health patient that underwent chemotherapy
and scoring the level of oral mucositis. There were eight
components in OAG: voice, swallow, lips, saliva, tongue, mucous
membrane, gums, and teeth. The total of these eight components
would be calculated to see the oral health condition. A normal
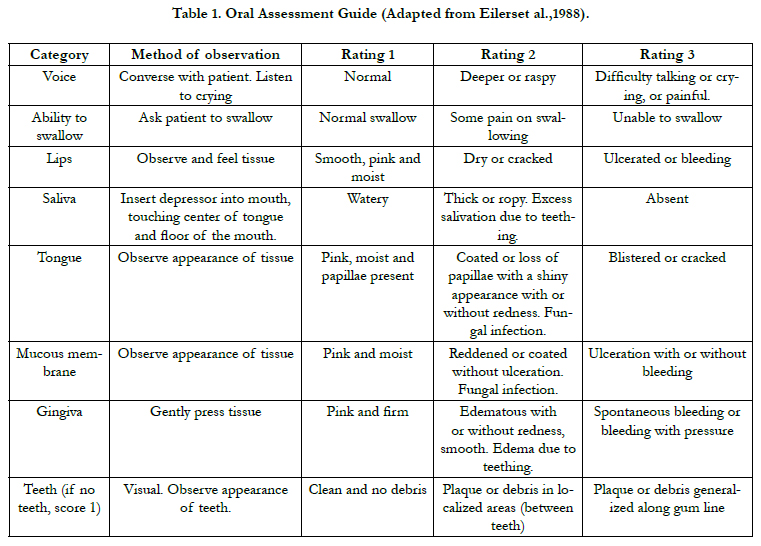
mouth would receive a score of 8 (Table 1).
Eleven children patients in National Cancer Hospital agreed to take part in this study. One day after the chemotherapy started, the researcher checked the patient’s oral health condition using Oral Assessment Guide (OAG). Then the patient started to gargle the probiotic twice a day for 7 days and the researcher rechecked the score of OAG. Patients continued gargling and researcher did the scoring of OAG 14 days later. OAG showed eight categories from oral cavity, those were voice, swallow, lips, saliva, tongue, mucous membrane, gums, and teeth.
The score were totaled; which increasing of the score indicated the severity of oral mucositis, whereas decreasing of the number meant improvement to the normal condition. Friedman test was performed to compare the score of Oral Assessment Guide before, after 7 days, and after 14 days gargling with probiotics since the data distribution was not normal.
Results
There were 11 patients that fulfilled the criteria and joined the program.
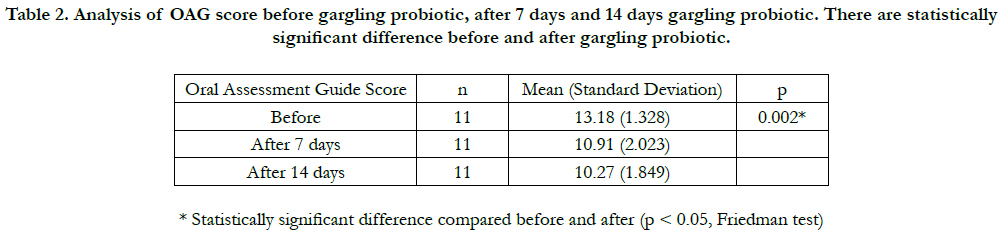
The OAG scores for each measurement were analyzed with
SPSS. The normality test with Shapiro-Wilk showed that the data
distribution was not normal with p-value< 0.05, therefore Friedman
test was used to see the difference between before, after 7
days and 14 days of the oral health condition by using OAG (Table
2).
Table 2. Analysis of OAG score before gargling probiotic, after 7 days and 14 days gargling probiotic. There are statistically significant difference before and after gargling probiotic.
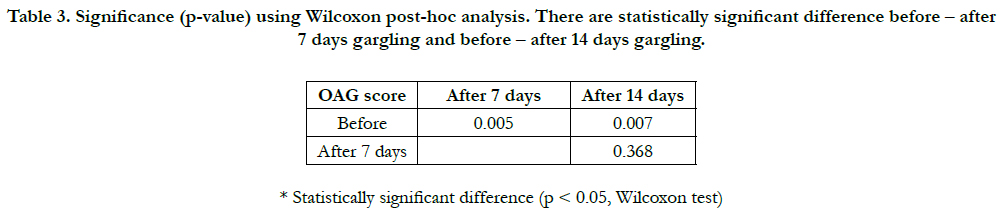
After the analysis had come out, the Wilcoxon post-hoc analysis was done to see the significance between each experimental time (Table 3).
Table 3. Significance (p-value) using Wilcoxon post-hoc analysis. There are statistically significant difference before – after 7 days gargling and before – after 14 days gargling.
Discussion
This study was undertaken to see the patients’ oral health condition
that were taking chemotherapy and their response in the oral
mucositis after short-term exposure to probiotic in ALL children
during the induction and consolidation phase of chemotherapy
treatment. The main finding showed that there was a decrease in
Oral Assessment Guide score after 7 days and 14 days gargling
with probiotic for 1 minute twice a day for 14 days.
One of the treatment option for children with leukemia is chemotherapy.
Methotrexate and cytarabine are used for leukemia which
have side effects in oral mucositis [15]. Chemotherapy destroys
the basal cell when drugs get into the cell through blood vessel
of submucous connective tissue. The progress of mucositis
is complex and dynamic, it can be described in five stages: initiation,
primary damage response, signal amplification, ulceration,
and healing [12, 16].
Oral status monitoring in patients with chemotherapy is important
in the treatment and prevention of inflammatory lesions or
ulcers [15]. This study showed a decrease in OAG score before
gargling with after gargling probiotics for 7 days and 14 days.
Probiotics contain mostly Lactobacillus species and Lactobacillus
casei is used in this study. Probiotic organisms can compete with
potential pathogens for nutrients and growth factors, disintegration
of toxins, local and systemic immunomodulation, develops
a mucosal barrier, and activates immune system [17]. Probiotic
can prevent mucositis not only in oral but also gastrointestinal,
with symptoms as nausea, vomiting, and abdominal pain [18]. A
previous study showed that oral and intestinal could be relevant
to mucositis development and treatment but no specific probiotic
formula has found to human clinical trial [4]. Other studies
reported that probiotic reduced oral and intestinal inflammation
in immunosuppressed experimental rats, also prevent mucositis
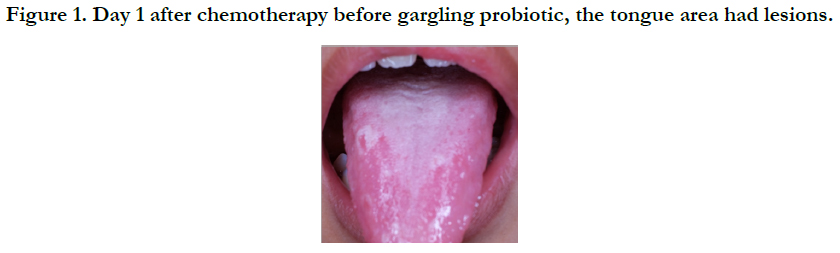
symptoms [18, 19]. Some patients showed improvement in mucous
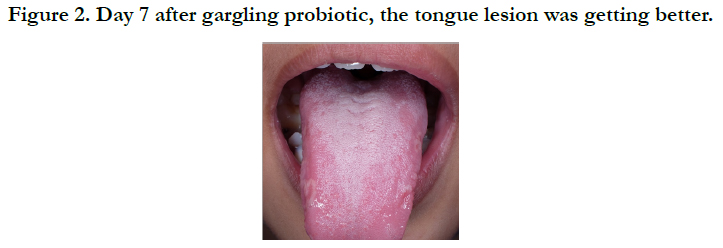
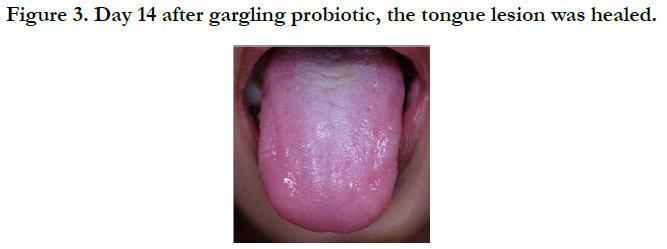
membrane, saliva, lips, and tongue area in this study. Figure
1 to figure 3 showed the improvement of tongue lesion in one of
the patients. The tongue had a lesion because of the chemotherapy
effect (figure 1) and the lesion healed after gargling probiotics
for 7 days (figure 2) and 14 days (figure 3).
A study showed that probiotic reduced oral mucositis by improving the immunity of patients and it reduced the incidence of oral mucositis induced by chemoradiotherapy in patients with nasopharyngeal carcinoma [20]. An initial treatment with chemotherapy cause damage and death of basal epithelial cells, whereas progressive mucosal destruction results in ulceration [4]. In this study, OAG score in leukemia patients showed nonparametric data (Table 2), and there was a statistically significant decrease of OAG score between before with 7 days and 14 days after gargling probiotic (Table 3). It meant that the probiotic gave effect in decreasing OAG score after gargling but no statistically significant changes was found between after 7 days with 14 days. It maybe because of the probiotics that had already taken for 7 days and after 14 days the OAG score was decreased but not significant. The result is similar to some research that showed probiotics can reduce inflammation in oral and intervene to mucositis [13, 14].
The obstacles in this study were in the sample size, limited time and patients that fulfilled the criteria. As we know that the chemotherapy caused systemic weakness, so not all leukemia patients could follow the method. We recommend that future studies with same approach consider to increase in sample size, provide more time and maybe can do it in another types of cancer.
Conclusion
This study showed that there was a statistical score difference of
OAG before and after gargling with probiotics in children patients with leukemia that are having chemotherapy. Mostly chemotherapy
drugs give same side effects and they act not only in
cancer cells but also in healthy cells. Therefore, probiotics could
be an alternative therapy and prevention for oral mucositis.
Acknowledgement and Declarations
The researcher would like to thank the patients and parents who
were willing to take part in this research, doctors from the hospital
and those who participated in this study. The authors confirmed
that there was no conflict of interest in this research.
References
- Ribeiro ILA, Limeira RRT, Dias de Castro R, Ferreti Bonan PR, Valença AMG. Oral Mucositis in Pediatric Patients in Treatment for Acute Lymphoblastic Leukemia. Int J Environ Res Public Health. 2017 Nov 28;14(12):1468. Pubmed PMID: 29182564.
- Herrstedt J. Prevention and management of mucositis in patients with cancer. Int J Antimicrob Agents. 2000 Oct;16(2):161-3. Pubmed PMID: 11053801.
- Naidu MU, Ramana GV, Rani PU, Mohan IK, Suman A, Roy P. Chemotherapy- induced and/or radiation therapy-induced oral mucositis--complicating the treatment of cancer. Neoplasia. 2004 Sep-Oct;6(5):423-31. Pubmed PMID: 15548350.
- Cereda E, Caraccia M, Caccialanza R. Probiotics and mucositis. Curr Opin Clin Nutr Metab Care. 2018;21(5):399–404. Pubmed PMID: 29916923.
- Miller MM, Donald D V., Hagemann TM. Prevention and Treatment of Oral Mucositis in Children with Cancer. J Pediatr Pharmacol Ther [Internet]. 2012;17(4):340–50.Pubmed PMID: 23413048.
- Al Jaouni SK, Al Muhayawi MS, Hussein A, Elfiki I, Al-Raddadi R, Al Muhayawi SM, et al. Effects of Honey on Oral Mucositis among Pediatric Cancer Patients Undergoing Chemo/Radiotherapy Treatment at King Abdulaziz University Hospital in Jeddah, Kingdom of Saudi Arabia. Evidence-based Complement Altern Med. 2017;2017:1–7.Pubmed PMID:28270852.
- Volpato LER, Silva TC, Oliveira TM, Sakai VT, Machado MAAM. Radiation therapy and chemotherapy-induced oral mucositis. Braz J Otorhinolaryngol. 2007;73(4):562–8. Pubmed PMID: 17923929.
- Farrington M, Cullen L, Dawson C. Assessment of Oral Mucositis in Adult and Pediatric Oncology Patients: an evidence-based approach. ORL Head Neck Nurs [Internet]. 2010;28(3):8–15. Pubmed PMID:20863028.
- Jain P, Sharma P. Probiotics and Their Efficacy in Improving Oral Health: A review. J Appl Pharm Sci. 2012;2(11):151–63.
- Cheng KKF, Ip WY, Lee V, Li CH, Yuen HL, Epstein JB. Measuring Oral Mucositis of Pediatric Patients with Cancer: A Psychometric Evaluation of Chinese Version of the Oral Mucositis Daily Questionnaire. Asia Pac J Oncol Nurs. 2017;4(4):330-5. Pubmed PMID:28966962.
- Cheng KK., Chang A., Yuen M. Prevention of oral mucositis in paediatric patients treated with chemotherapy: a randomised crossover trial comparing two protocols of oral care. Eur J Cancer [Internet]. 2004;40(8):1208–16. Pubmed PMID: 15110885.
- Redding SW. Cancer Therapy-Related Oral Mucositis. J Dent Educ. 2005;69(8):919–29.
- Sharma A, Tilak T, Bakhshi S, Raina V, Kumar L, Chaudhary SP, et al. Lactobacillus brevis CD2 lozenges prevent oral mucositis in patients undergoing high dose chemotherapy followed by haematopoietic stem cell transplantation. ESMO Open. 2016;1(6).
- Van Sebille YZA, Stansborough R, Wardill HR, Bateman E, Gibson RJ, Keefe DM. Management of Mucositis During Chemotherapy: From Pathophysiology to Pragmatic Therapeutics. Curr Oncol Rep. 2015;17(50).
- Garrocho-Rangel JA, Herrera-Moncada M, Márquez-Preciado R, Tejeda- Nava F, Ortiz-Zamudio JJ, Pozos-Guillén A. Oral mucositis in paediatric acute lymphoblastic leukemia patients receiving methotrexate-based chemotherapy: case series. Eur J Paediatr Dent. 2018;19(3):239–42.Pubmed PMID: 30063158.
- Kwon Y. Mechanism-based management for mucositis : option for treating side effects without compromising the efficacy of cancer therapy. Onco Targets Ther. 2016;9:2007–16. Pubmed PMID: 27103826.
- Murarka P, Thosar N, Baliga S, Rathi N. Probiotics - A Boon to Preventive Dentistry. Eur J Pharm Med Res. 2017;4(06):413–24.
- Picó-Monllor JA, Mingot-Ascencao JM. Search and Selection of Probiotics That Improve Mucositis Symptoms in Oncologic Patients. A Systematic Review. Nutrients. 2019;11(2322). Pubmed PMID: 31581434.
- Gerhard D, Sousa FJSS, Andraus RAC, Pardo PE, Nai GA, Neto HB, et al. Probiotic therapy reduces inflammation and improves intestinal morphology in rats with induced oral mucositis. Braz Oral Res. 2017Jul 3;31:e71. Pubmed PMID: 28678976.
- Jiang C, Wang H, Xia C, Dong Q, Chen E, Qiu Y, et al. A randomized, double-blind, placebo-controlled trial of probiotics to reduce the severity of oral mucositis induced by chemoradiotherapy for patients with nasopharyngeal carcinoma. Cancer. 2019;125(7):1081–90.Pubmed PMID: 30521105.