Knowledge, Attitude and Practice on Management of Oral Submucous Fibrosis among General Dentists - Survey
Sindhu Priya Kuppusamy Sundara Murthy1, Maragathavalli2*, Suresh3
1 Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India.
2 Professor, Department of Oral Medicine, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
3 Reader, Department of Prosthodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha
University, Chennai, 600077, India.
*Corresponding Author
Dr. Maragathavalli,
Professor, Department of Oral Medicine, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
Tel: +91 94451 71146
E-mail: drgopalvalli@gmail.com
Received: July 08, 2019; Accepted: August 03, 2019; Published: August 08, 2019
Citation:Sindhu Priya Kuppusamy Sundara Murthy, Maragathavalli, Suresh. Knowledge, Attitude and Practice on Management of Oral Submucous Fibrosis among General
Dentists - Survey. Int J Dentistry Oral Sci. 2020;7(10):931-936. doi: dx.doi.org/10.19070/2377-8075-20000184
Copyright: Maragathavalli©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
It is a precancerous condition, progressive fibrosis leads to rigidity and causing inability to open the mouth. There are various
treatments involved, dexamethasone hyaluronidase, mouth opening exercises, etc. To evaluate the awareness, knowledge on Oral
Submucous Fibrosis management among general dentists for betterment of treatment. In this cross-sectional study 112 dentists
filled out self-administered questionnaires assessing dentist’s awareness on the management of OSMF. More than 50% of the
patients understand the basic treatment for OSMF, and less than 50% of patients had lack of knowledge in the combination treatment
involved for OSMF and advanced treatment options of OSMF. In this study, 84% of the population had the knowledge on
the basic treatment modalities to cure and prevent further spread for OSMF, among which 73% answered discontinuation of the
habit. 92% of the dentists had general knowledge on the basic diagnosis of OSMF, such as; mouth opening. When asked about
the combination therapy and more advanced treatment options, such as; biogenic stimulators, only 50% of the dentists answered
correctly. Overall, most of the dentists had good knowledge on the basic treatment administered to treat and cure OSMF but
had lack of knowledge in the combination and more advanced treatments necessary to cure the more advanced stage of OSMF.
2.Introduction
3.Materials and Method
4.Results and Discussion
5.Conclusion
6.Acknowledgement
7.References
Keywords
OSMF; Combination Treatment; Betel Nuts.
Introduction
Oral submucous fibrosis is a chronic progressive and irreversible
condition affecting the oral, oropharyngeal, and sometimes esophageal
mucosa. The characteristic features of OSMF are loss
of pigmentation of oral mucosa, blanching and leathery texture
of oral mucosa, depapillation and reduced movement of tongue,
progressive reduction of mouth opening and sunken cheeks [1].
The disease is seen in those from Indian subcontinent and southeast
Asia such as Taiwan in 1952.
Initially in 1952, shwartz discovered a disease in 5 Indian patients.
He called the disease ‘atrophia idiopathica mucosae orris’. The
same disease was described by Pindborg as an insidious, chronic
disease affecting any part of mouth and pharynx. In 1953, Joshi
described this condition as ‘submucous fibrosis’ [2, 3].
It causes significant morbidity (loss of mouth function as tissues
become rigid and mouth opening becomes difficult) and mortality
(transformation into squamous cell carcinoma occurs). The introduction
of chewing tobacco containing areca nuts into the market
has been associated with a sharp increase in frequency of OSMF.
The various treatments are initially cessation of the habit of
chewing betel quid, areca nut. Various steroid forms used as injections
are trypsin, collagenous, hyaluronidase, oral zinc and pentoxifylline
[4-6].
Previously our team had conducted numerous clinical trials [7-11]
and lab animal studies [12-18] and in-vitro students [19-21] over
the past 5 years. Now we are focussing on epidemiological surveys.
The idea for this survey stemmed from the current interest
in our community. The aim of this study is to evaluate the awareness, knowledge on Oral Submucous Fibrosis management
among general dentists for betterment of treatment.
Materials and Methods
A cross sectional survey was conducted among the dentists of
Saveetha Dental college and hospitals and other dentists based in
Chennai. A self-administered questionnaire was prepared to assess
the awareness on management of OSMF. The nature of this
study was explained to the subjects and informed consent was
obtained. The questionnaire was administered through an online
survey planet link. The survey had 10 questions on the management
of OSMF. All the collected data were cross verified and
compiled together in an excel sheet. Compiled data were statistically
analysed with help of SPSS software.
Results and Discussion
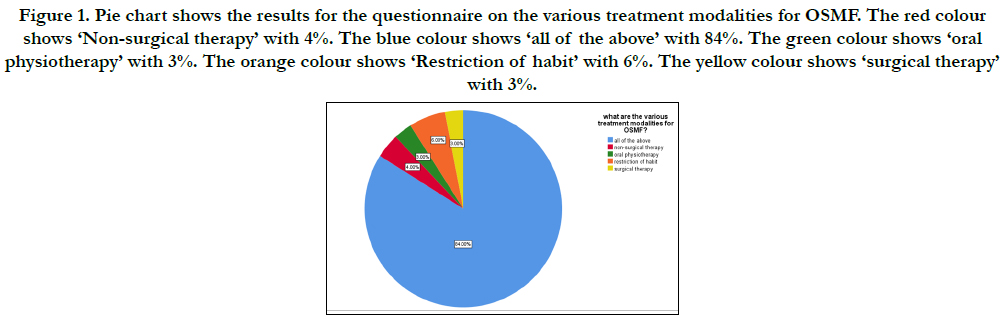
In the present study, when questioned about the various modalities
of treatment in fig.1 of OSMF, 84% of the population said all
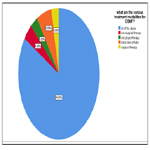
of the above. For the question ‘what is the normal mouth opening?’
92% gave the correct answer of 35-70mm from fig.2. 64%
of the population answered fiberotomy for the typical surgery of
OSMF from fig.3. The first step to treat OSMF is discontinuation
of the habit was given by 73% of the patients in fig.4. ‘all of the
above’ was mentioned by 52% of the population for nutritional
support for OSMF in fig.5.
When questioned about what acts as a biogenic stimulation to
help increase blood circulation, physiological action and absorption,
‘placental extract’ was answered by 50% in fig.6 of dentists.
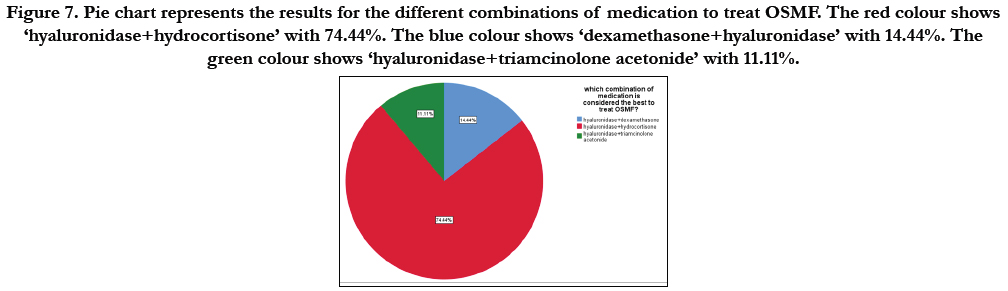
The best combination of medication is hyaluronidase and hydrocortisone
acetate, given correctly by 67% of dentists in fig.7. The
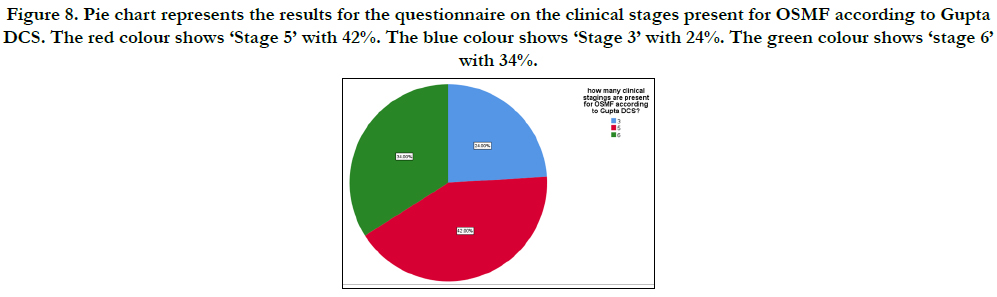
total number of clinical stages was correctly answered by 42% as
5 stages in fig.8. From grade IV the surgery is done for OSMF,
82% have answered this correctly in fig.9.
The 3 basic treatment modalities are surgery, iron supplement,
injection of hyaluronidase was answered by 59% in fig.10.
Figure 1. Pie chart shows the results for the questionnaire on the various treatment modalities for OSMF. The red colour shows ‘Non-surgical therapy’ with 4%. The blue colour shows ‘all of the above’ with 84%. The green colour shows ‘oral physiotherapy’ with 3%. The orange colour shows ‘Restriction of habit’ with 6%. The yellow colour shows ‘surgical therapy’ with 3%.
Figure 2. Pie chart shows the results for the questionnaire on the normal mouth opening. The red colour shows ‘35-70mm’ with 92%. The blue colour shows ‘20-40mm’ with 5%. The green colour shows ‘45-90mm’ with 3%.
Figure 3. Pie chart represents the results for the questionnaire on the typical name for surgery treatment for OSMF. The red colour shows ‘Laser’ with 19%. The blue colour shows ‘Fibrotomy’ with 64%. The green colour shows ‘vestibulectomy’ with 17%.
Figure 4. Pie chart represents the results for the questionnaire on the first step to treat OSMF. The red colour shows ‘Restriction of habit’ with 73%. The blue colour shows ‘physiotherapy’ with 11%. The green colour shows ‘surgery’ with 16%.
Figure 5. Pie chart represents the results for the questionnaire on the different Nutritional supports for OSMF. The red colour shows ‘iron’ with 32%. The blue colour shows ‘all of the above’ with 52%. The green colour shows ‘vitamin A,B’ with 16%.
Figure 6. Pie chart represents the results for the questionnaire on the different products that acts as a biogenic stimulator to help increase blood circulation, physiological action and absorption of exudates. The red colour shows ‘heat wave’ with 23%. The blue colour shows ‘alpha lipoic acid’ with 50%. The green colour shows ‘placental extract’ with 27%.
Figure 7. Pie chart represents the results for the different combinations of medication to treat OSMF. The red colour shows ‘hyaluronidase+hydrocortisone’ with 74.44%. The blue colour shows ‘dexamethasone+hyaluronidase’ with 14.44%. The green colour shows ‘hyaluronidase+triamcinolone acetonide’ with 11.11%.
Figure 8. Pie chart represents the results for the questionnaire on the clinical stages present for OSMF according to Gupta DCS. The red colour shows ‘Stage 5’ with 42%. The blue colour shows ‘Stage 3’ with 24%. The green colour shows ‘stage 6’ with 34%.
Figure 9. Pie chart represents the results for the questionnaire to identify the correct clinical stage of OSMF to undergo surgery as a treatment. The red colour shows ‘Grade IV’ with 82%. The blue colour shows ‘Grade III’ with 5%. The green colour shows ‘Grade V’ with 13%.
Figure 10. Pie chart represents the results for the questionnaire on the basic treatment modalities done for any clinical staging in OSMF. The red colour shows ‘Iron, inj. dexamethasone, lycopene’ with 65.56%. The blue colour shows ‘antioxidants, vitamins, iron, lycopene’ with 7.78%. The green colour shows ‘surgery, iron, hyaluronidase’ with 28.67%.
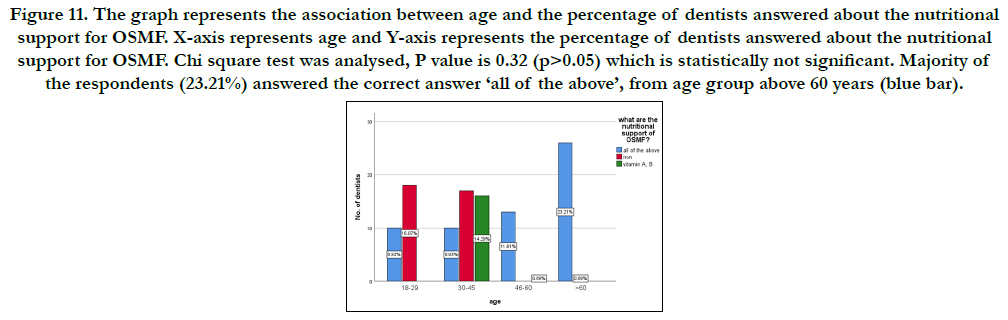
Figure 11. The graph represents the association between age and the percentage of dentists answered about the nutritional support for OSMF. X-axis represents age and Y-axis represents the percentage of dentists answered about the nutritional support for OSMF. Chi square test was analysed, P value is 0.32 (p>0.05) which is statistically not significant. Majority of the respondents (23.21%) answered the correct answer ‘all of the above’, from age group above 60 years (blue bar).
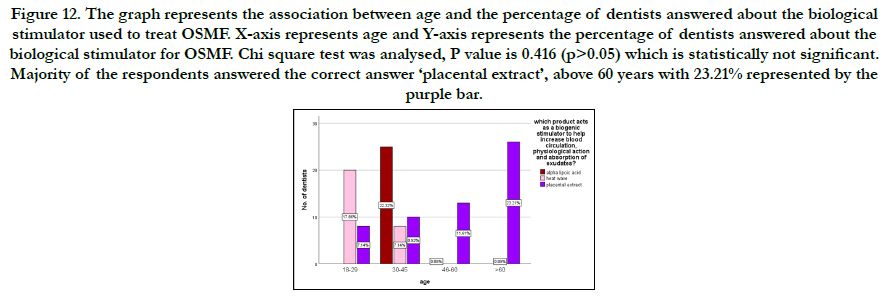
Figure 12. The graph represents the association between age and the percentage of dentists answered about the biological stimulator used to treat OSMF. X-axis represents age and Y-axis represents the percentage of dentists answered about the biological stimulator for OSMF. Chi square test was analysed, P value is 0.416 (p>0.05) which is statistically not significant. Majority of the respondents answered the correct answer ‘placental extract’, above 60 years with 23.21% represented by the purple bar.
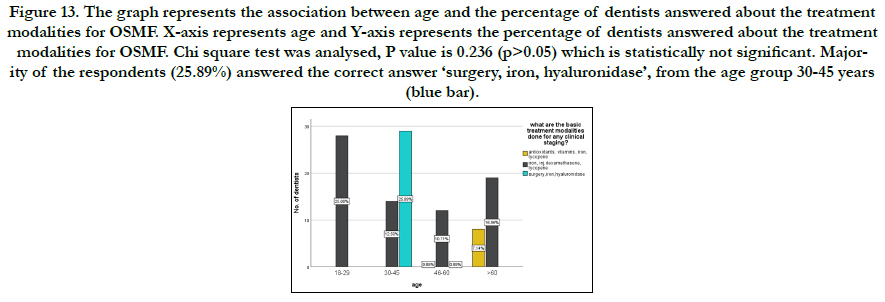
Figure 13. The graph represents the association between age and the percentage of dentists answered about the treatment modalities for OSMF. X-axis represents age and Y-axis represents the percentage of dentists answered about the treatment modalities for OSMF. Chi square test was analysed, P value is 0.236 (p>0.05) which is statistically not significant. Majority of the respondents (25.89%) answered the correct answer ‘surgery, iron, hyaluronidase’, from the age group 30-45 years (blue bar).
In the present study, more than 50% of dentists knew about the treatment for OSMF. Less than 50% of dentists knew about the clinical staging and combination treatment for OSMF. Various classifications have been proposed depending on the clinical features by Wahi et Al. who classified OSMF based on clinical features, severity, and extent of involvement by Pindborg classified the histology into 4 stages [22-24].
Stomatitis is the first symptom and significant feature in the initial stage of OSMF. Stomatitis includes erythematous mucosa, vesicles, mucosal ulcers and mucosal petechiae. The epithelial atrophy of oral mucosa can easily be irritated. The patient complains of burning sensation on eating hot and spicy food. Burning sensation is the initial symptom, followed by either hyper salivation or dryness of mouth. The fibrous bands gradually become palpable in the buccal mucosa [25, 26]. Involvement of the soft palate is marked by fibrotic change and a clear delineation of the soft palate from the hard palate as if a ‘heavy curtain’ is hanging from the hard palate. Uvula may be shrunken, and in extreme cases it becomes ‘bud like’ or ‘hockey stick like’.
OSMF is considered among the high risk PMD that progress into cancer. An atrophic mucosa is more likely to undergo malignant transformation and the rate of OSMF converting into malignancy is 4.5–7.6% [27]. Kakar et Al reported that patients treated with hyaluronidase showed quicker improvement in symptoms, but a combination of corticosteroids gave better long-term results.
Hyaluronidase degrades fibrous matrix promoting the lysis of fibrin coagulum. Relieving the symptoms and softening the fibrous tissue. Other methods include injection of placental extract, use of trypsin, collagenase, hyaluronidase, and elastase.
A study from India used the general health questionnaire -28 to assess the psychological morbidity in OSMF. Assessing the quality of life of OSMF patients is complex, considering the large number of variables which impact the patient’s self-perception [28, 29].
Conclusion
OSMF is a widely occurring condition with significant morbidity
and mortality associated with it. This study showed that dentists
are aware of the various basic treatment modalities to cure and
prevent OSMF, but there was lack of knowledge on the more
advanced treatment options. The advanced options such as combination
therapy and biogenic stimulators need to be more familiarised
among the dentists, as it is proved to provide better
prognosis and quality of life for patients.
Acknowledgment
This research was supported by Saveetha Dental College and
Hospital. We thank the department of Oral Medicine,Saveetha
Dental College for providing insight and expertise that greatly assisted
this research.
References
- McCullough MJ, Prasad G, Farah CS. Oral mucosal malignancy and potentially malignant lesions: an update on the epidemiology, risk factors, diagnosis and management. Aust Dent J. 2010 Jun;55 Suppl 1:61-5.Pubmed PMID: 20553246.
- Afroz N, Hasan SA, Naseem S. Oral submucous fibrosis a distressing disease with malignant potential. Indian J Community Med. 2006 Oct 1;31(4):270-77.
- Auluck A, Rosin MP, Zhang L, Sumanth KN. Oral submucous fibrosis, a clinically benign but potentially malignant disease: report of 3 cases and review of the literature. J Can Dent Assoc. 2008 Oct;74(8):735-40.Pubmed PMID: 18845065.
- Jayanthi V, Probert CS, Sher KS, Mayberry JF. Oral submucosal fibrosis--a preventable disease. Gut. 1992 Jan;33(1):4-6.
- Mehrotra R, Singh M, Kumar D, Pandey AN, Gupta RK, Sinha US. Age specific incidence rate and pathological spectrum of oral cancer in Allahabad. Indian J Med Sci. 2003 Sep;57(9):400-4.Pubmed PMID: 14515030.
- Gupta L, Gupta N, Punn K, Chandel S. Oral submucous fibrosis: A clinical note. Asian J Oral Health Allied Sci. 2011 Jul;1(3):229.
- Venugopal A, Uma Maheswari TN. Expression of matrix metalloproteinase-9 in oral potentially malignant disorders: A systematic review. J Oral Maxillofac Pathol. 2016 Sep-Dec;20(3):474-479.Pubmed PMID: 27721614.
- Chaitanya NC, Muthukrishnan A, Babu DBG, Kumari CS, Lakshmi MA, Palat G, et al. Role of Vitamin E and Vitamin A in Oral Mucositis Induced by Cancer Chemo/Radiotherapy- A Meta-analysis. J Clin Diagn Res. 2017 May;11(5):ZE06-ZE09.Pubmed PMID: 28658926.
- Subashri A, Maheshwari TN. Knowledge and attitude of oral hygiene practice among dental students. Res J Pharm Technol. 2016;9(11):1840-2. =
- Maheswari TNU, Venugopal A, Sureshbabu NM, Ramani P. Salivary micro RNA as a potential biomarker in oral potentially malignant disorders: A systematic review. Ci Ji Yi Xue Za Zhi. 2018 Apr-Jun;30(2):55-60.Pubmed PMID: 29875583.
- Misra SR, Shankar YU, Rastogi V, Maragathavalli G. Metastatic hepatocellular carcinoma in the maxilla and mandible, an extremely rare presentation. Contemp Clin Dent. 2015 Mar;6(Suppl 1):S117-21. doi: 10.4103/0976- 237X.152966. PMID: 25821363.
- Steele JC, Clark HJ, Hong CH, Jurge S, Muthukrishnan A, Kerr AR, et al. World Workshop on Oral Medicine VI: an international validation study of clinical competencies for advanced training in oral medicine. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015 Aug;120(2):143-51.Pubmed PMID: 25861956.
- Muthukrishnan A, Warnakulasuriya S. Oral health consequences of smokeless tobacco use. Indian J. Med. Res. 2018 Jul;148(1):35.
- Patil SR, Maragathavalli G, Araki K, Al-Zoubi IA, Sghaireen MG, Gudipaneni RK, et al. Three-rooted mandibular first molars in a Saudi Arabian population: a CBCT study. Pesqui. Bras. Odontopediatria Clín. Integr. 2018 Aug 27;18(1):4133.
- Chaitanya NC, Muthukrishnan A, Krishnaprasad CMS, Sanjuprasanna G, Pillay P, Mounika B. An Insight and Update on the Analgesic Properties of Vitamin C. J Pharm Bioallied Sci. 2018 Jul-Sep;10(3):119-125.Pubmed PMID: 30237682.
- Rohini S, Kumar VJ. Incidence of dental caries and pericoronitis associated with impacted mandibular third molar-A radiographic study. Res J Pharm Technol. 2017;10(4):1081-4.
- Dharman S, Muthukrishnan A. Oral mucous membrane pemphigoid - Two case reports with varied clinical presentation. J Indian Soc Periodontol. 2016 Nov-Dec;20(6):630-634.Pubmed PMID: 29238145.
- Muthukrishnan A, Bijai Kumar L, Ramalingam G. Medication-related osteonecrosis of the jaw: a dentist's nightmare. BMJ Case Rep. 2016 Apr 6;2016:bcr2016214626.Pubmed PMID: 27053542.
- Subha M, Arvind M. Role of magnetic resonance imaging in evaluation of trigeminal neuralgia with its anatomical correlation. Biomed. Pharmacol. J. 2019 Mar 25;12(1):289-96.
- Muthukrishnan A, Bijai Kumar L. Actinic cheilosis: early intervention prevents malignant transformation. BMJ Case Rep. 2017 Mar 20;2017:bcr2016218654.Pubmed PMID: 28320702.
- Choudhury P, Panigrahi RG, Maragathavalli, Panigrahi A, Patra PC. Vanishing roots: first case report of idiopathic multiple cervico-apical external root resorption. J Clin Diagn Res. 2015 Mar;9(3):ZD17-9.Pubmed PMID: 25954713.
- Wahi PN, Kapur VL, Luthra UK, Srivastava MC. Submucous fibrosis of the oral cavity. 2. Studies on epidemiology. Bull. World Health Organ. 1966;35(5):793-9.
- Pindborg JJ, Sirsat SM. Oral submucous fibrosis. Oral Surg Oral Med Oral Pathol Oral Radiol. 1966 Dec 1;22(6):764-79.
- Lai DR, Chen HR, Lin LM, Huang YL, Tsai CC. Clinical evaluation of different treatment methods for oral submucous fibrosis. A 10-year experience with 150 cases. J Oral Pathol Med. 1995 Oct;24(9):402-6.Pubmed PMID: 8537913.
- More C, Thakkar K. Oral submucous fibrosis-an insight. J Dent. 2010;1(3).
- Reddy V, Wanjari PV, Banda NR, Reddy P. Oral submucous fibrosis: Correlation of clinical grading to various habit factors. Int. j. dent. clin. 2011 Mar 31;3(1).
- Daftary DK. Oral precancerous lesions and conditions of tropical interest. Oral diseases in the tropics. 1993:402-28.
- Rawson K, Prasad R, Nair A, Josephine J. Oral submucous fibrosis-The Indian scenario: Review and report of three treated cases. J Indian Acad Oral Med Radiol. 2017 Oct 1;29(4).
- DeSa JV. LXXXVII Submucous Fibrosis of the Palate and Cheek. Ann Otol Rhinol Laryngol. 1957 Dec;66(4):1143-59.