Oral Status Of Pregnant Women - A Hospital Based Study
Fathima Bareera Rezvi1, Revathi Duraisamy2*, Manjari Chaudhary3
1 Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, India.
2 Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
3 Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
*Corresponding Author
Revathi Duraisamy,
Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, 600077, India.
Tel: 7598267022
E-mail: revathid.sdc@saveetha.com
Received: September 06, 2020; Accepted: October 09, 2020; Published: October 24, 2020
Citation:Fathima Bareera Rezvi, Revathi Duraisamy, Manjari Chaudhary. Oral Status Of Pregnant Women - A Hospital Based Study Int J Dentistry Oral Sci. 2020;7(10):881-887. doi: dx.doi.org/10.19070/2377-8075-20000175
Copyright: Revathi Duraisamy© 2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Oral health of women during pregnancy is important. Not only can it compromise the outcomes of pregnancy, it may also affect
the overall health of the newborn. Proper dental care during pregnancy is very important, since pregnancy causes various
hormonal changes in the body that can actually increase the risk of developing gum diseases. The aim of the study was to assess
the oral status of pregnant women who visited Saveetha Dental College. A survey was conducted among pregnant females who
had reported to Saveetha Dental College, from the time period of June 2019 to March 2020. A questionnaire consisting of questions
on oral health was asked. Patient records were reviewed and 60 pregnant females were selected. Descriptive statistics, cross
tabulation and chi-square test were done by SPSS IBM software 20.0. Bleeding gums were reported by 68%, dental caries by 61%,
halitosis by 70% while mobility and sensitivity was reported by 35% and 33% respectively. No association was found between the
diet of pregnant women and their oral status. Pearson’s Chi Square value: 3.389, p value: 0.06 (>0.05). No association was found
between the diet of pregnant women and their oral status.. Within the limits of the present study oral status of pregnant women
was assessed. Most patients experienced gingival bleeding, dental caries and halitosis while few patients experience mobility and
sensitivity. No association was found between the diet of pregnant women and their oral status.
2.Introduction
3.Materials and Method
4.Results and Discussion
5.Conclusion
6.Acknowledgement
7.References
Keywords
Oral Status; Pregnancy; Gingival Bleeding; Dental Caries; Halitosis.
Introduction
From the perspective of oral health, pregnancy is considered a
unique, sensitive and crucial period. This is due to the physical,
hormonal and emotional changes that take place during this period
[1]. Proper dental care during pregnancy is very important,
since pregnancy causes various hormonal changes in the body that
can actually increase the risk of developing gum diseases causing
pregnant women to be more susceptible to gingival inflammation
[2]. During pregnancy women are said to be vulnerable to certain
oral diseases such as dental caries and periodontal diseases.
Due to inadequate maintenance of oral health during this period
there are implications for oral health in the woman's subsequent
life [3, 4]. Furthermore, during the first trimester, regular self-oral
hygiene care, such as tooth brushing and flossing is important. It
is nearly impossible in some women especially in the premolar
and molar area because of pregnancy related nausea and vomiting
symptoms [3]. This situation may impact the quality of the
mother’s life [4]. Although the changes in clinical parameters for
gingival inflammation like bleeding on probing, was said to be
reversible at the end of pregnancy or after delivery [5-7]. A previous
study has shown that periodontal treatment during pregnancy
improves quality of life [4].
Hormonal changes during pregnancy along with gastric acid secretion
causes recurrent morning sickness, leading to erosion of
dental enamel [5]. Furthermore progesterone decreases plasma
bicarbonate levels contributing to reduced pH [8]. This along with
increased sugar consumption due to cravings, increases the risk
of candida colonisation [6] and dental caries [7, 9-11] which left
untreated leads to tooth mobility [12]. Changes in oral hygiene
practices and dietary habits can increase the risk of tooth decay
during pregnancy [13]. This is supported by a study conducted in
Iraq that showed a significant difference in decayed teeth among
pregnant women and non pregnant women [14]. It has also been
suggested that children born to mothers who have high caries levels are more likely to develop early caries [15, 16].
Hormonal variations during pregnancy, estrogen and progesterone
could exacerbate the inflammatory response in dental plaque,
resulting in severe forms of gingivitis [17-20]. Due to increased
production of oestrogen and progesterone during pregnancy,
there is an increased development of gingivitis and periodontitis.
This is attributed to increased vascular permeability and tissue
oedema [17, 21]. Studies show the association between periodontal
disease with gestational diabetes mellitus, which contributes to
maternal and infant morbidity as well as the risk of the mother
developing type 2 diabetes mellitus subsequently [22, 23]. Moreover,
maternal periodontal disease may increase the risk of adverse
pregnancy outcomes such as pre-eclampsia, pre-term births, retarded
fetal growth and low birth weight [24, 25]. The above relationships
could be explained by the poor awareness of the importance
of oral hygiene and inaccessibility to dental clinics [26, 27].
Periodontitis, gingivitis and poor oral health are common causes
of halitosis, which occurs due to volatile sulfur compounds by
oral bacteria [28, 29].
Previously our team had conducted numerous clinical trials [30-
36] systematic reviews [37-42] and survey [43] over the past five
years. Maintaining oral health during pregnancy may be achieved
by early screening and referring pregnant mothers to oral treatment
to complete overall well-being of the mother and fetus.This
survey aims to assess the oral status of pregnant women who
visited Saveetha Dental College.
Materials and Methods
Our study population consisted of 50 pregnant patients who visited
Saveetha Dental College in the past one year. A questionnaire
with oral health related questions was developed. Ethical
clearance was obtained from the institutional ethics board - SDC/
SIHEC/2020/DIASDATA/0619-0320
The data was retrieved from 86,000 patients’ records among
which 60 pregnant patients were selected. Phone calls were made
to the patient and the patient was asked about their oral health.
This study involved 3 reviewers. Data included the study were
from the time period of June 2019 to March 2020. Certain measurements
were taken in order to minimize bias, such as simple random sampling, collecting more data sources and including the
data from the institute.
The data was then entered in Microsoft Excel and was analysed
using SPSS IBM software version 20.0. Descriptive statistics were
calculated to explore the demographic data. A cross tabulation
analysis was conducted to examine the categorical variables. Chisquare
test was used to identify the presence of significance between
the variables.
1. Are you experiencing bleeding gums during pregnancy?
2. Are you experiencing mobility of your teeth?
3. Do you have any dental caries?
4. Do you experience bad breath during pregnancy?
5. Do you experience teeth sensitivity during pregnancy?
Results and Discussion
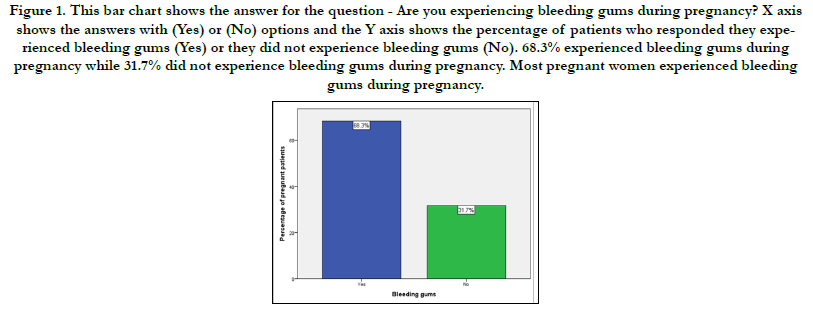
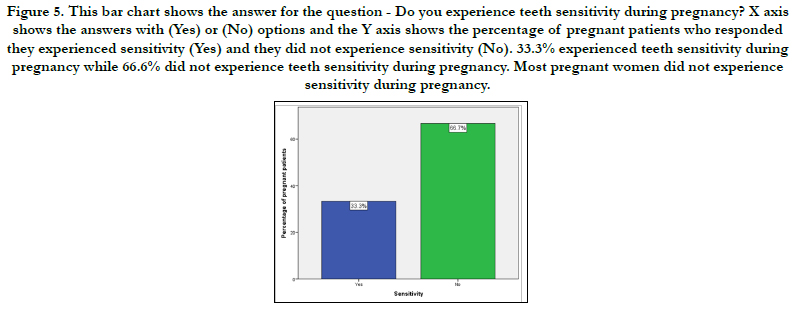
The following results were obtained from our study. 68.3% of
the participants reported they experienced bleeding gums during
pregnancy and 31.7% of the participants reported they did not
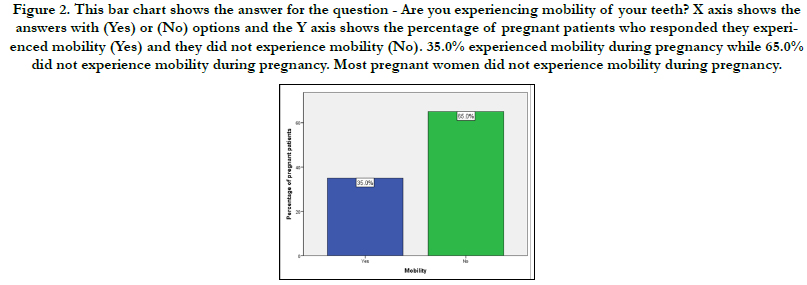
experience bleeding gums during pregnancy (Figure 1). Mobility
was experienced by 35% of the participants and was not experienced
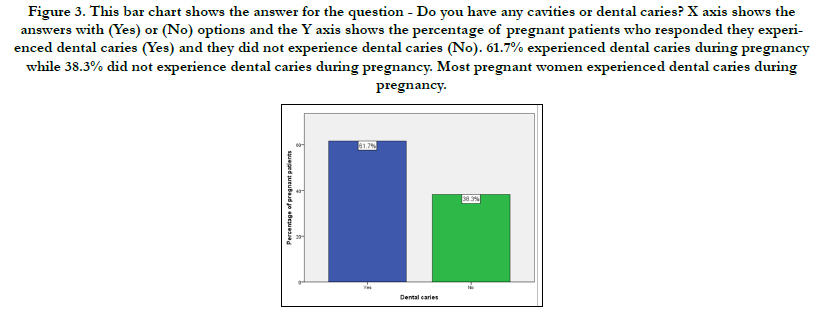
by 65% of the participants (Figure 2). 61.7% of participants
reported they experienced dental caries during pregnancy
and 38.3% of participants reported they did not experience dental
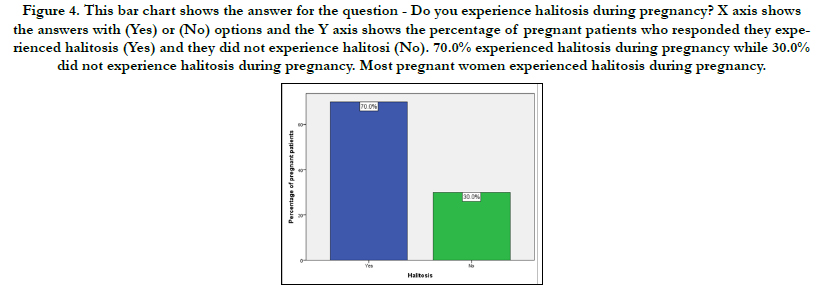
caries during pregnancy (Figure 3). Halitosis was experienced by
70% of the participants and was not experienced by 30% of
the participants (Figure 4). 33.3% of the participants reported
they experienced sensitivity during pregnancy and 66.7% of participants
reported they did not experience sensitivity during pregnancy
(Figure 5).
Figure 1. This bar chart shows the answer for the question - Are you experiencing bleeding gums during pregnancy? X axis shows the answers with (Yes) or (No) options and the Y axis shows the percentage of patients who responded they experienced bleeding gums (Yes) or they did not experience bleeding gums (No). 68.3% experienced bleeding gums during pregnancy while 31.7% did not experience bleeding gums during pregnancy. Most pregnant women experienced bleeding gums during pregnancy.
Figure 2. This bar chart shows the answer for the question - Are you experiencing mobility of your teeth? X axis shows the answers with (Yes) or (No) options and the Y axis shows the percentage of pregnant patients who responded they experienced mobility (Yes) and they did not experience mobility (No). 35.0% experienced mobility during pregnancy while 65.0% did not experience mobility during pregnancy. Most pregnant women did not experience mobility during pregnancy.
Figure 3. This bar chart shows the answer for the question - Do you have any cavities or dental caries? X axis shows the answers with (Yes) or (No) options and the Y axis shows the percentage of pregnant patients who responded they experienced dental caries (Yes) and they did not experience dental caries (No). 61.7% experienced dental caries during pregnancy while 38.3% did not experience dental caries during pregnancy. Most pregnant women experienced dental caries during pregnancy.
Figure 4. This bar chart shows the answer for the question - Do you experience halitosis during pregnancy? X axis shows the answers with (Yes) or (No) options and the Y axis shows the percentage of pregnant patients who responded they experienced halitosis (Yes) and they did not experience halitosi (No). 70.0% experienced halitosis during pregnancy while 30.0% did not experience halitosis during pregnancy. Most pregnant women experienced halitosis during pregnancy.
Figure 5. This bar chart shows the answer for the question - Do you experience teeth sensitivity during pregnancy? X axis shows the answers with (Yes) or (No) options and the Y axis shows the percentage of pregnant patients who responded they experienced sensitivity (Yes) and they did not experience sensitivity (No). 33.3% experienced teeth sensitivity during pregnancy while 66.6% did not experience teeth sensitivity during pregnancy. Most pregnant women did not experience sensitivity during pregnancy.
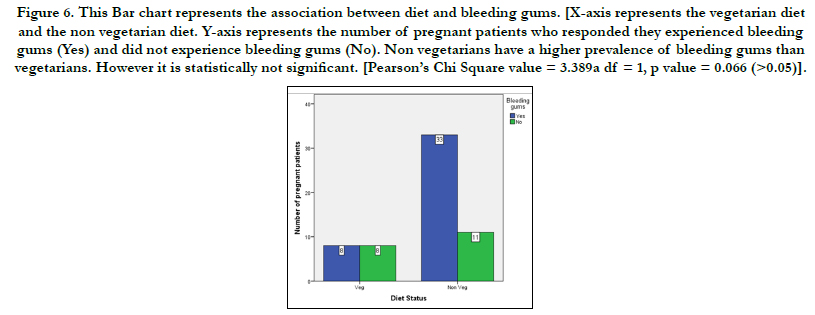
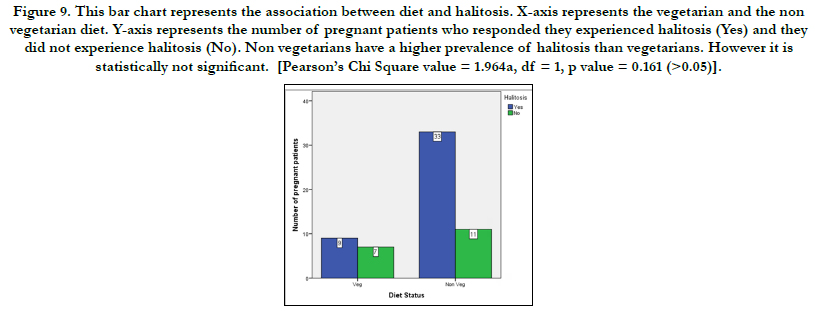
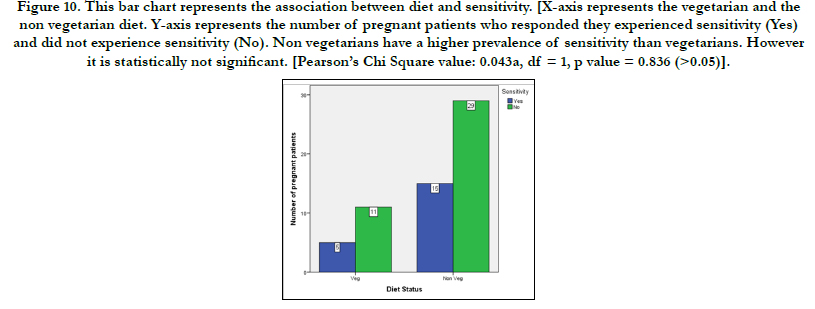
When comparing the diet status and the oral status of the patients, following results were obtained in or study. Non vegetarians have a higher prevalence of bleeding gums than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value = 3.389a , df = 1, p value = 0.066 (>0.05)] (Figure 6). Non vegetarians have a higher prevalence of mobility than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value = 0.959a , df = 1, p value = 0.327 (>0.05)] (Figure 7). Non vegetarians have a higher prevalence of dental caries than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value: 1.641a, df = 1, p value = 0.200 (>0.05)] (Figure 8). Non vegetarians have a higher prevalence of halitosis than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value = 1.964a , df = 1, p value = 0.161 (>0.05)] (Figure 9). Non vegetarians have a higher prevalence of sensitivity than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value: 0.043a , df = 1, p value = 0.836 (>0.05)] (Figure 10).
Figure 6. This Bar chart represents the association between diet and bleeding gums. [X-axis represents the vegetarian diet and the non vegetarian diet. Y-axis represents the number of pregnant patients who responded they experienced bleeding gums (Yes) and did not experience bleeding gums (No). Non vegetarians have a higher prevalence of bleeding gums than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value = 3.389a df = 1, p value = 0.066 (>0.05)].
Figure 7. This bar chart represents the association between diet and mobility. [X-axis represents the vegetarian and the non vegetarian diet. Y-axis represents the number of pregnant patients who responded they experienced mobility (Yes) and they did not experience mobility (No). Non vegetarians have a higher prevalence of mobility than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value = 0.959a df = 1, p value = 0.327 (>0.05)].
Figure 8. This Bar chart represents the association between diet and dental caries. [X-axis represents the vegetarian and the non vegetarian diet. Y-axis represents the number of pregnant patients who responded they experienced dental caries (Yes) and did not experience dental caries (No). Non vegetarians have a higher prevalence of dental caries than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value: 1.641a df = 1, p value = 0.200 (>0.05)].
Figure 9. This bar chart represents the association between diet and halitosis. X-axis represents the vegetarian and the non vegetarian diet. Y-axis represents the number of pregnant patients who responded they experienced halitosis (Yes) and they did not experience halitosis (No). Non vegetarians have a higher prevalence of halitosis than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value = 1.964a, df = 1, p value = 0.161 (>0.05)].
Figure 10. This bar chart represents the association between diet and sensitivity. [X-axis represents the vegetarian and the non vegetarian diet. Y-axis represents the number of pregnant patients who responded they experienced sensitivity (Yes) and did not experience sensitivity (No). Non vegetarians have a higher prevalence of sensitivity than vegetarians. However it is statistically not significant. [Pearson’s Chi Square value: 0.043a, df = 1, p value = 0.836 (>0.05)].
From the results of our study we can see that 68.3% of women experienced bleeding gums during pregnancy. Nata Fonseca Silva et al [44], states that gingivitis can be considered the main oral disease affecting women in the gestational period, due to an increase in the concentration of female sex hormones. According to our study 35% of pregnant women experienced mobility during pregnancy. This result is in line with A.George et al [45], where mobility was present in few patients in his study. This could because the periodontal status of each patient differs, which could eventually lead the difference in mobility.
61.7% of our patients experienced dental caries which is similar to the studies by George et al [45], Africa et al [46], Kamate et al [47]. The mean DMFT score was 7.18 in [46] which was higher than the score of 4.08 reported in a rural hospital in India. Increased caries activity may be seen due to increased candida levels in the oral cavity. In [45] 41.5% reported cavities as a dental problem.
Bad breath (halitosis) was reported by 70% of patients as their major concern. This result is similar to the study conducted by Naorungroj et al [48] in which 61% of pregnant women reported bad breath experience. This could be due to poor oral hygiene status, higher plaque deposits along with increased nausea and vomiting during pregnancy. 33.3% of pregnant women experienced sensitivity during pregnancy. A review by VT Hemalatha et al [49] stated that sensitivity was not seen in most patients during pregnancy. Tooth erosion can result from nausea and vomiting of pregnancy [50], because of the hydrochloric acid content of regurgitated gastric juice [51]. There is possibility for the buffering capacity of saliva to change during pregnancy leading to a more acidic environment [52]. Effects of tooth erosion such as tooth sensitivity may last beyond the duration of pregnancy [53]. All pregnant women do not experience vomiting and this could be one of the reasons for lower prevalence of sensitivity.
Limitations of the study include smaller sample size, education level of the patient and other pregnancy complications. Hence for future scope a larger sample size could be used with better knowledge and treatment modalities along with providing adequate education on oral health care of pregnant women.
Conclusion
Within the limits of the present study oral status of pregnant
women was assessed. Most patients experienced gingival bleeding,
dental caries and halitosis while few patients experienced mobility
and sensitivity. No association was found between the diet of
pregnant women and their oral status.
Acknowledgement
Thanks to Saveetha Dental college for allowing me to review the
case sheets.
Authors Contribution
First author (Fathima Bareera Rezvi) performed the analysis, and
interpretation and wrote the manuscript. Second author (Dr. Revathi
Duraisamy) contributed to conception, data design, analysis,
interpretation and critically revised the manuscript. Third
author(Dr.Manjari Chaudhary) participated in the study and revised
the manuscript. All the three authors have discussed the
results and contributed to the final manuscript.
References
- Nicolau B, Thomson WM, Steele JG, Allison PJ. Life-course epidemiology: concepts and theoretical models and its relevance to chronic oral conditions. Community Dent Oral Epidemiol. 2007 Aug; 35(4): 241-9. PMID: 17615010.
- Basha FYS, Ganapathy D. Oral Hygiene Status among Pregnant Women. Research Journal of [Internet]. 2018.
- Taani DQ, Habashneh R, Hammad MM, Batieha A. The periodontal status of pregnant women and its relationship with socio-demographic and clinical variables. J Oral Rehabil. 2003 Apr; 30(4): 440-5. PMID: 12631171.
- Musskopf ML, Milanesi FC, Rocha JMD, Fiorini T, Moreira CHC, Susin C, et al. Oral health related quality of life among pregnant women: a randomized controlled trial. Braz Oral Res. 2018; 32: e002. PMID: 29364329.
- Annan B, Nuamah K. Oral pathologies seen in pregnant and non-pregnant women. Ghana Med J. 2005 Mar; 39(1): 24-7. PMID: 17299537.
- Rio R, Simões-Silva L, Garro S, Silva MJ, Azevedo Á, Sampaio-Maia B. Oral yeast colonization throughout pregnancy. Med Oral Patol Oral Cir Bucal. 2017 Mar 1; 22(2): e144-e148. PMID: 28160578.
- Vasiliauskiene I, Milciuviene S, Bendoraitiene E, Narbutaite J, Slabsinskiene E, Andruskeviciene V. Dynamics of pregnant women's oral health status during preventive programme. Stomatologija. 2007; 9(4): 129-36. PMID: 18303278.
- Naveen S, Asha ML, Shubha G, Bajoria AA, Jose AA. Salivary Flow rate, pH and buffering capacity in pregnant and non pregnant women-A comparative study. JMED research. 2014; 2014: 1-8.
- Kidd E. Essentials of Dental Caries: The Disease and Its Management (3rd Edtn). OUP Oxford. 2005; 180.
- Silk H, Douglass AB, Douglass JM, Silk L. Oral health during pregnancy. American family physician. 2008 Apr 15; 77(8): 1139-44.
- Rakchanok N, Amporn D, Yoshida Y, Harun-Or-Rashid M, Sakamoto J. Dental caries and gingivitis among pregnant and non-pregnant women in Chiang Mai, Thailand. Nagoya J Med Sci. 2010 Feb; 72(1-2): 43-50. PMID: 20229702.
- Giglio JA, Lanni SM, Laskin DM. Oral health care for the pregnant patient. Dental Assistant. 2013 Nov 1; 82(6): 38.
- Evans RD, Briggs PF. Tooth-surface loss related to pregnancy-induced vomiting. Prim Dent Care. 1994 Sep; 1(1): 24-6. PMID: 8941784.
- Khamrco TY, Saleh KM. A comparative study in dental caries prevalence and treatment needs of pregnant women and single females in Mosul city, Iraq. Al-Rafidain Dental Journal. 2003; 1(1): 57–64.
- Berkowitz RJ. Acquisition and transmission of mutans streptococci. J Calif Dent Assoc. 2003 Feb; 31(2): 135-8. PMID: 12636317.
- Weintraub JA, Prakash P, Shain SG, Laccabue M, Gansky SA. Mothers' caries increases odds of children's caries. J Dent Res. 2010 Sep; 89(9): 954-8. PMID: 20505046.
- Gürsoy M, Pajukanta R, Sorsa T, Könönen E. Clinical changes in periodontium during pregnancy and post-partum. J Clin Periodontol. 2008 Jul; 35(7): 576-83. PMID: 18430046.
- Tilakaratne A, Soory M, Ranasinghe AW, Corea SM, Ekanayake SL, de Silva M. Periodontal disease status during pregnancy and 3 months post-partum, in a rural population of Sri-Lankan women. J Clin Periodontol. 2000 Oct; 27(10): 787-92. PMID: 11034128.
- Carrillo-de-Albornoz A, Figuero E, Herrera D, Bascones-Martínez A. Gingival changes during pregnancy: II. Influence of hormonal variations on the subgingival biofilm. J Clin Periodontol. 2010 Mar; 37(3): 230-40. PMID: 20088983.
- Morelli EL, Broadbent JM, Leichter JW, Thomson WM. Pregnancy, parity and periodontal disease. Aust Dent J. 2018 May 16. PMID: 29770451.
- Straka M. Pregnancy and periodontal tissues. Neuro Endocrinol Lett. 2011; 32(1): 34-8. PMID: 21407157.
- Xiong X, Elkind-Hirsch KE, Vastardis S, Delarosa RL, Pridjian G, Buekens P. Periodontal disease is associated with gestational diabetes mellitus: a casecontrol study. J Periodontol. 2009 Nov; 80(11): 1742-9. PMID: 19905944.
- Xiong X, Buekens P, Vastardis S, Pridjian G. Periodontal disease and gestational diabetes mellitus. Am J Obstet Gynecol. 2006 Oct; 195(4): 1086–9.
- Saddki N, Bachok N, Hussain NH, Zainudin SL, Sosroseno W. The association between maternal periodontitis and low birth weight infants among Malay women. Community Dent Oral Epidemiol. 2008 Aug; 36(4): 296- 304. PMID: 19145718.
- Cruz SS, Costa Mda C, Gomes-Filho IS, Rezende EJ, Barreto ML, Dos Santos CA, et al. Contribution of periodontal disease in pregnant women as a risk factor for low birth weight. Community Dent Oral Epidemiol. 2009 Dec; 37(6): 527-33. PMID: 19694773.
- Vamos CA, Thompson EL, Avendano M, Daley EM, Quinonez RB, Boggess K. Oral health promotion interventions during pregnancy: a systematic review. Community Dent Oral Epidemiol. 2015 Oct; 43(5): 385-96. PMID: 25959402.
- Amin M, ElSalhy M. Factors affecting utilization of dental services during pregnancy. J Periodontol. 2014 Dec; 85(12): 1712-21. PMID: 25119559.
- van den Broek AM, Feenstra L, de Baat C. A review of the current literature on management of halitosis. Oral Dis. 2008 Jan; 14(1): 30-9. PMID: 18173446.
- Mumghamba EG, Manji KP, Michael J. Oral hygiene practices, periodontal conditions, dentition status and self-reported bad mouth breath among young mothers, Tanzania. Int J Dent Hyg. 2006 Nov; 4(4): 166-73. PMID: 17038053.
- Jyothi S, Robin PK, Ganapathy D. Periodontal health status of three different groups wearing temporary partial denture. Research Journal of Pharmacy and Technology. 2017; 10(12): 4339-42.
- Duraisamy R, Krishnan CS, Ramasubramanian H, Sampathkumar J, Mariappan S, Navarasampatti Sivaprakasam A. Compatibility of Nonoriginal Abutments With Implants: Evaluation of Microgap at the Implant-Abutment Interface, With Original and Nonoriginal Abutments. Implant Dent. 2019 Jun; 28(3): 289-295. PMID: 31124826.
- Ganapathy D, Sathyamoorthy A, Ranganathan H, Murthykumar K. Effect of Resin Bonded Luting Agents Influencing Marginal Discrepancy in All Ceramic Complete Veneer Crowns. J Clin Diagn Res. 2016 Dec; 10(12): ZC67-ZC70. PMID: 28209008.
- Vijayalakshmi B, Ganapathy D. Medical management of cellulitis. Research Journal of Pharmacy and Technology. 2016; 9(11): 2067-70.
- Ashok V, Nallaswamy D, Benazir Begum S, Nesappan T. Lip Bumper Prosthesis for an Acromegaly Patient: A Clinical Report. J Indian Prosthodont Soc. 2014 Dec; 14(Suppl 1): 279-82. PMID: 26199531.
- Venugopalan S, Ariga P, Aggarwal P, Viswanath A. Case Report: Magnetically retained silicone facial prosthesis. Nigerian Journal of Clinical Practice. 2014 Mar 27; 17(2): 260-4.
- Ajay R, Suma K, Ali SA, Kumar Sivakumar JS, Rakshagan V, Devaki V, et al. Effect of Surface Modifications on the Retention of Cement-retained Implant Crowns under Fatigue Loads: An In vitro Study. J Pharm Bioallied Sci. 2017 Nov; 9(Suppl 1):S154-S160. PMID: 29284956.
- Kannan A, Venugopalan S. A systematic review on the effect of use of impregnated retraction cords on gingiva. Research Journal of Pharmacy and Technology. 2018; 11(5): 2121-6.
- Kannan A. Effect of Coated Surfaces influencing Screw Loosening in Implants: A Systematic Review and Meta-analysis. World. 2017 Nov; 8(6): 496-502.
- Ranganathan H, Ganapathy DM, Jain AR. Cervical and Incisal Marginal Discrepancy in Ceramic Laminate Veneering Materials: A SEM Analysis. Contemp Clin Dent. 2017 Apr-Jun; 8(2): 272-278. PMID: 28839415.
- Subasree S, Murthykumar K. Effect of Aloe Vera in Oral Health-A Review. Research Journal of Pharmacy and Technology. 2016; 9(5): 609-12.
- Selvan SR, Ganapathy D. Efficacy of fifth generation cephalosporins against methicillin-resistant Staphylococcus aureus-A review. Research Journal of Pharmacy and Technology. 2016; 9(10): 1815-8.
- Jain AR, Nallaswamy D, Ariga P, Ganapathy DM. Determination of correlation of width of maxillary anterior teeth using extraoral and intraoral factors in Indian population: A systematic review. World J Dent. 2018 Jan; 9: 68-75.
- Ashok V, Suvitha S. Awareness of all ceramic restoration in rural population. Research Journal of Pharmacy and Technology. 2016;9(10):1691–3.
- Natã Fonseca Silva R, Rodrigues Monteiro M, Verly Grodzikwoski B, Alves deCastro FL, Moreira Roriz V. Periodontal profile and oral hygiene status in pregnants at maternity hospital in the state of Goias, Brazil. Revista clínica de periodoncia, implantología y rehabilitación oral. 2018 Dec; 11(3): 140-2.
- George A, Johnson M, Blinkhorn A, Ajwani S, Bhole S, Yeo AE, et al. The oral health status, practices and knowledge of pregnant women in southwestern Sydney. Aust Dent J. 2013 Mar; 58(1): 26-33. PMID: 23441789.
- Africa CW, Turton M. Oral health status and treatment needs of pregnant women attending antenatal clinics in KwaZulu-Natal, South Africa. International journal of dentistry. 2019 Mar 4; 2019.
- Kamate WI, Vibhute N, Baad R, Belgaumi U, Kadashetti V, Bommanavar S. Effect of socioeconomic status on dental caries during pregnancy. J Family Med Prim Care. 2019 Jun; 8(6): 1976-1980. PMID: 31334165.
- Naorungroj S, Hunsrisakhun J, Talungchit S. Oral hygiene status, self-reported oral malodor, oral hygiene practices, and oral health knowledge: A cross-sectional study in a group of Muslim Thai pregnant women. Journal of International Oral Health. 2018 Sep 1; 10(5): 229.
- Vt H, Nisha A. Dental considerations in pregnancy-a critical review on the oral care. J Clin Diagn Res. 2013 May; 7(5): 948-53. PMID: 23814753.
- Kumar J, Samelson R. Oral health care during pregnancy recommendations for oral health professionals. N Y State Dent J. 2009 Nov; 75(6): 29-33. PMID: 20069785.
- Johansson AK, Omar R, Carlsson GE, Johansson A. Dental erosion and its growing importance in clinical practice: from past to present. International journal of dentistry. 2012 Jan 1; 2012.
- Laine MA. Effect of pregnancy on periodontal and dental health. Acta Odontol Scand. 2002 Oct; 60(5): 257-64. PMID: 12418714.
- Enabulele J, Ibhawoh L. Resident obstetricians' awareness of the oral health component in management of nausea and vomiting in pregnancy. BMC Pregnancy Childbirth. 2014 Nov 25; 14:388. PMID: 25421787.