Alveoloplasty - Prevalence and Prerequisites: Prosthetic Point Of View
Kalyani P1, Jessy P2*, Subhabrata Maiti3, M. P. Santhosh Kumar4
1 Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai-600077, India.
2 Senior Lecturer, Department of Pedodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University 162, Poonamallee High Road, Chennai-600077, Tamil Nadu, India.
3 Senior Lecturer, Department of Prosthodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University 162, Poonamallee High Road, Chennai-600077, Tamil Nadu, India.
4 Reader, Department of Oral and Maxillofacial Surgery, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University 162, Poonamallee High Road, Chennai-600077, Tamil Nadu, India.
*Corresponding Author
Jessy P,
Senior Lecturer, Department of Pedodontics, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University 162, Poonamallee High Road,
Chennai-600077, Tamil Nadu, India.
Tel: +918861646189
E-mail: jessyp.sdc@saveetha.com
Received: September 06, 2020; Accepted: October 09, 2020; Published: October 243, 2020
Citation:Kalyani P, Jessy P, Subhabrata Maiti, M. P. Santhosh Kumar. Alveoloplasty - Prevalence and Prerequisites: Prosthetic Point Of View. Int J Dentistry Oral Sci. 2020;7(10):872-877. doi: dx.doi.org/10.19070/2377-8075-20000173
Copyright: Jessy P©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Complete denture construction is one of the most commonly performed procedures in a dental setting. Prior to complete dentures it is important to assess the ridge contour for the presence of any bony prominences, spicules or flabby tissues. Alveoloplasty is a procedure of pre-prosthetic mouth preparation that is aimed at the removal of such irregular ridge contours. The aim of the study was to determine the prevalence of cases requiring alveoloplasty and the timing of alveoplasty before complete denture construction. The retrospective study involved analysis of case records of patients who underwent alveoloplasty prior to complete denture construction and assessment based on following parameters: age, gender, timing and arch of alveoloplasty. Statistical analysis was done using SPSS Version 20.0. Categorical variables were expressed as frequency and percentage and associations were tested using Chi-square test. The sample size of the study was 100. Prevalence of Alveoloplasty procedures was 26.6% with a male predilection [53%]. Delayed alveoloplasty was the most prevalent [83%] and the association between gender and timing of alveoloplasty was statistically not significant [Chi-square test, p>0.05]. There is a high need for immediate alveoloplasty procedures post extraction to avoid multiple surgical visits.
2.Introduction
3.Materials and Methods
4.Results and Discussion
5.Conclusion
6.Authors Contributions
7.Acknowledgements
8.Refereces
Keywords
Alveoloplasty; Complete Denture; Delayed; Immediate; Prevalence.
Introduction
Edentulism can be defined as a condition that can be either complete
with loss of entire dentition or partial with loss of one or
more teeth and retaining the others. Edentulism is one of the
most commonly encountered problems in a dental office [1]. The
reasons for edentulism can be decay, periodontal disease, fracture
of crown or root, failure of endodontic treatment. In particular,
complete edentulism differs from partial edentulism in that it affects
the physical, mental and social well being of a person.
According to the World Health Organisation, 'Edentulism is a
poor public health outcome that substantially affects oral and
general health status' [2]. Hence, complete denture construction
plays a pivotal role in restoring not just the oral health but also the
psychological well-being of a person [3]. The complete denture
rests on the oral soft tissues and the underlying residual alveolar
ridge, which is subjected to constant remodelling under different
forces of oral complex. These soft tissues are not uniform in
all patients. Post extraction they tend to become either flabby or
tense. Similarly, the underlying residual ridge can also pose bony
prominences and undercuts. The form of the ridge can also vary
from being a flat ridge to a thin knife edged contour. The bony
prominences pose a major hindrance to denture construction and
denture stability. Such bony prominences and knife edged ridges,
when compressed by a denture can lead to irritation and ulceration
causing discomfort for the patient. This also increases the
chance of residual ridge resorption [RRR]. Moreover, the pattern
of ridge resorption that differs in maxilla and mandible adds up
further to the problems faced during denture construction [4].
Preprosthetic surgical procedures are aimed at creating a good
hard and soft tissue environment, in order to facilitate a retentive
and stable denture construction [4, 5]. The preprosthetic surgical
procedures include the following: alveoloplasty, frenectomy,
frenotomy, removal of tori, vestibuloplasty and ridge augmentation
procedures for increasing the ridge height and width. Alveoloplasty
is commonly performed in patients post extraction to
smoothen the ridge contour by elimination of bony spicules or
prominences [6]. The timing of alveoloplasty can be immediate
post extraction or delayed, which is done as a surgical appointment
after healing of extraction sites. A few studies have reported
on the effects of alveoloplasty on denture construction [7]. Bhuskute
et al. [8], presents a case report of an 81-year old male, who
underwent delayed alveoloplasty 3 weeks post extraction for correction
of bony prominences, that resulted in a well fitting and
comfortable prosthesis for the patient. But according to Neumeier
et al. [9], there is a 2.39% increase in the incidence of secondary
alveoloplasty procedures over the span of two years, which they
report to be alarming. However, there is very little literature evidence
reporting on the timing of alveoloplasty and associated advantages
and disadvantages. The aim of the study was to measure
the prevalence of Alveoloplasty among complete denture patients
and the timing (immediate/delayed) of alveoloplasty.
The study was conducted with the approval of the Institutional
Ethics Committee [SDC/SIHEC/2020/DIASDATA/
0619-0320]. The study consisted of one reviewer, one assessor
and one guide.
The study was designed to include all dental patients above 30
years of age who have undergone alveoloplasty for the purpose
of complete denture construction. The patients who did not fall
under this inclusion criteria were excluded.
The study was based on a Non probability convenience sampling.
To minimise the sampling bias, all the case sheets of patients who
underwent alveoloplasty prior to complete denture construction
were reviewed and included.
Data collection was done using the patient database with the timeframe
work of 1st June 2019 to 30th April 2020. About 41,438
case sheets were reviewed and those fitting under the inclusion
criteria were included. Cross verification of data was done by a reviewer. The collected data was tabulated based on the following
parameters:
● Patient’s demographic details
● Arch of alveoloplasty
● Timing of alveoloplasty
The variables were coded and the data was imported to SPSS.
Using SPSS Version 20.0, categorical variables were expressed in
terms of frequency and percentage, and bar graphs were plotted.
The statistical significance of associations was tested using the
Chi-square test.
Results and Discussion
The valid sample size of the study is N=100. The prevalence of
alveoloplasty procedures among complete denture patients was
found to be 26.6%.
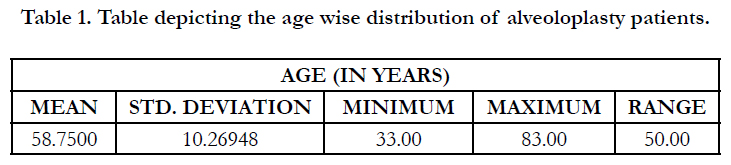
The age wise distribution of Alveoloplasty patients shows a minimum
age of 33 years, maximum age of 83 years and a mean age
of 58.75 ± 10.3 years [Table 1].
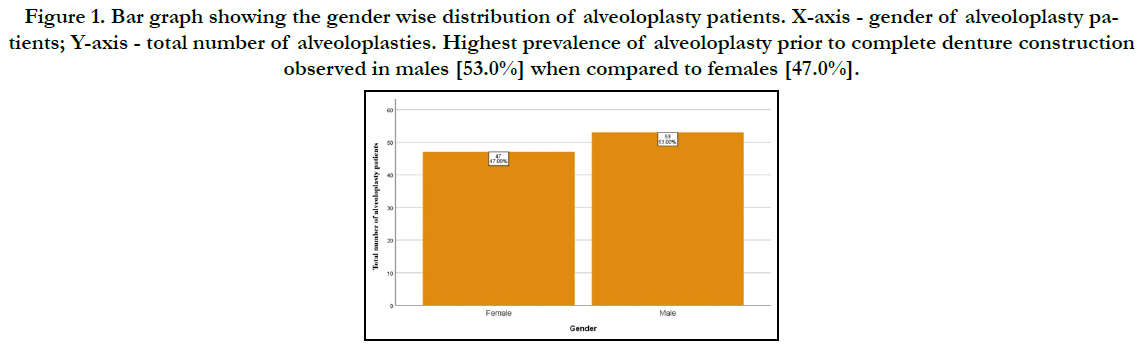
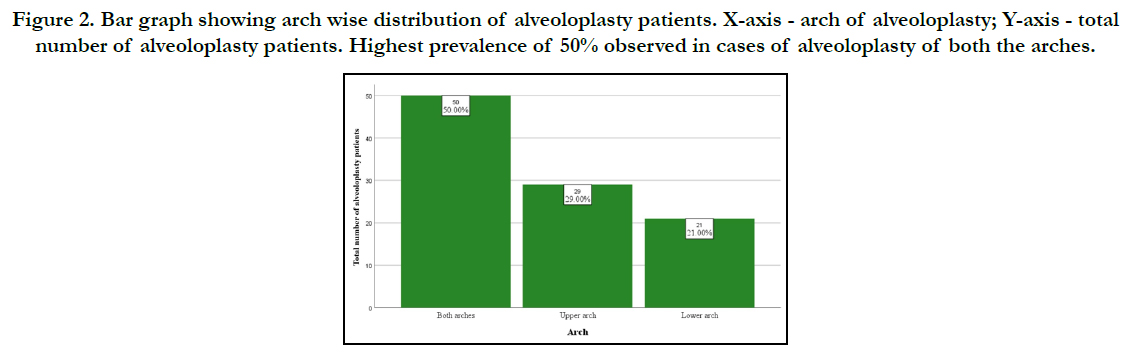
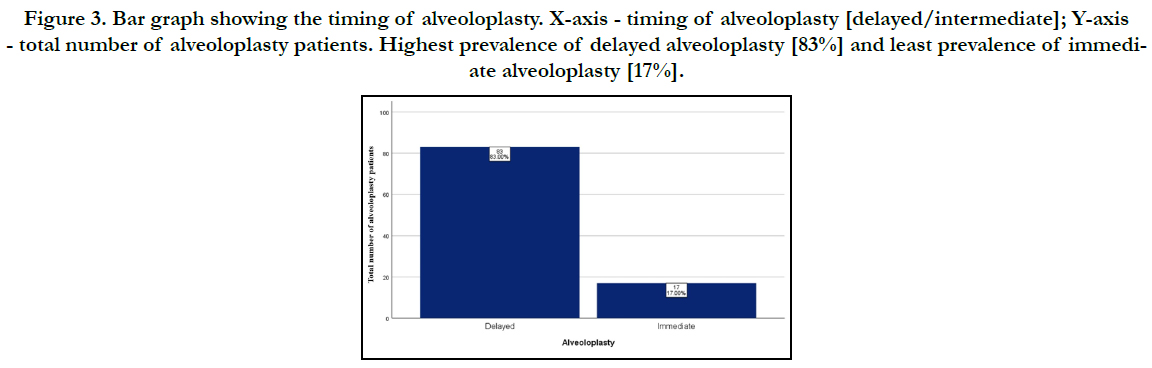
The gender wise distribution shows a male predilection, 53% (n=53) and 47% (n=47) in females. [Figure 1]. The arch wise distribution of alveoloplasty is as follows: 50% (n=50) involve both the arches, while 29% (n=29) is in the upper arch and 21% (n=21) involve the lower arch only. [Figure 2]. The timing of alveoloplasty as revealed by [Figure 3] is that most cases undergo delayed alveoloplasty 83% (n=83), while only 17% (n=17) undergo immediate alveoloplasty.
Figure 1. Bar graph showing the gender wise distribution of alveoloplasty patients. X-axis - gender of alveoloplasty patients; Y-axis - total number of alveoloplasties. Highest prevalence of alveoloplasty prior to complete denture construction observed in males [53.0%] when compared to females [47.0%].
Figure 2. Bar graph showing arch wise distribution of alveoloplasty patients. X-axis - arch of alveoloplasty; Y-axis - total number of alveoloplasty patients. Highest prevalence of 50% observed in cases of alveoloplasty of both the arches.
Figure 3. Bar graph showing the timing of alveoloplasty. X-axis - timing of alveoloplasty [delayed/intermediate]; Y-axis - total number of alveoloplasty patients. Highest prevalence of delayed alveoloplasty [83%] and least prevalence of immediate alveoloplasty [17%].
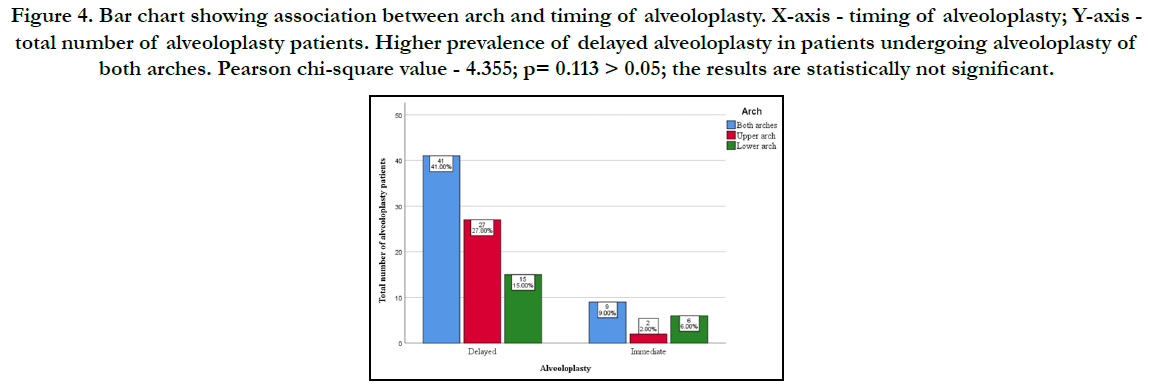
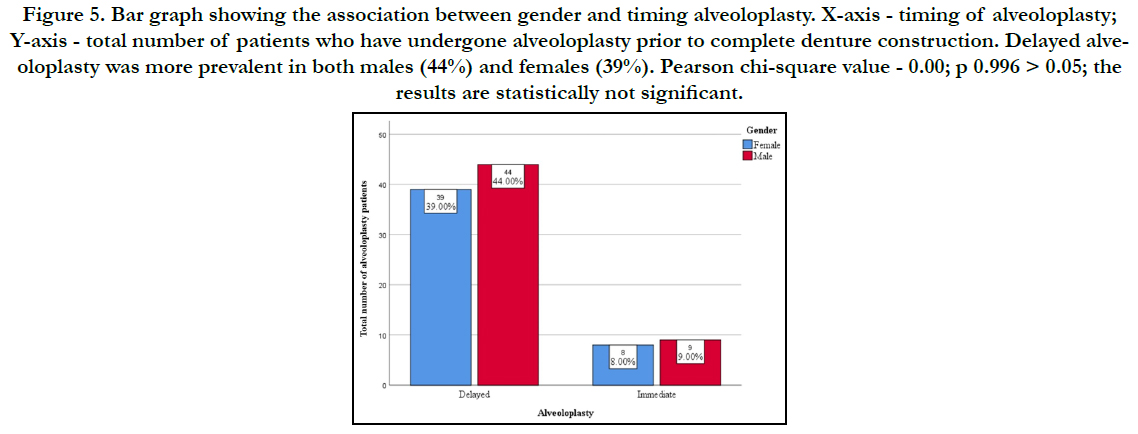
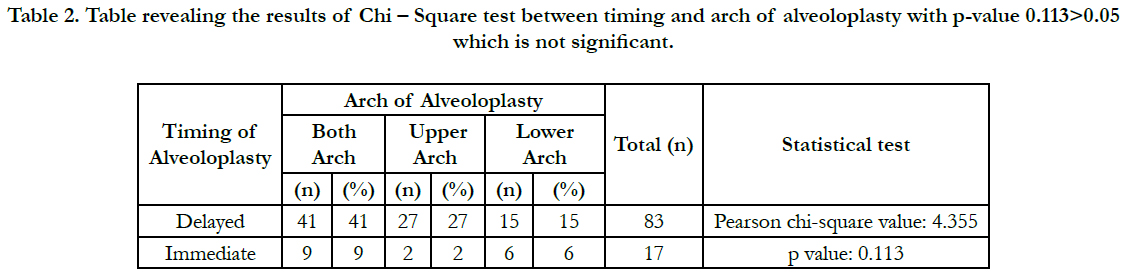
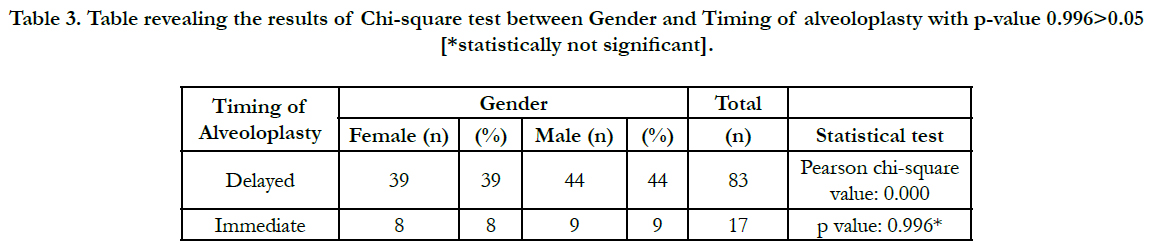
The association between arch of alveoloplasty and timing of alveoloplasty reveals that delayed alveoloplasty shows greater prevalence in patients undergoing alveoloplasty of both arches, 41% (n=41). Immediate alveoloplasty is commonly in cases involving both arches, 9% (n=9), closely followed by patients with lower arch alveoloplasty only, 6% (n=6) [Figure 4]. However, this association was found to be statistically not significant after a Chisquare test yielded a p-value of 0.113>0.05 [Table 2]. Evaluating the association between gender and timing of alveoloplasty, Delayed alveoloplasty was most prevalent in both males, 44% (n=44) and females, 39% (n=39) [Figure 5]. This association was also statistically not significant after a Chi-square test yielding a p-value of 0.996>0.05 [Table 3].
Figure 4. Bar chart showing association between arch and timing of alveoloplasty. X-axis - timing of alveoloplasty; Y-axis - total number of alveoloplasty patients. Higher prevalence of delayed alveoloplasty in patients undergoing alveoloplasty of both arches. Pearson chi-square value - 4.355; p= 0.113 > 0.05; the results are statistically not significant.
Figure 5. Bar graph showing the association between gender and timing alveoloplasty. X-axis - timing of alveoloplasty; Y-axis - total number of patients who have undergone alveoloplasty prior to complete denture construction. Delayed alveoloplasty was more prevalent in both males (44%) and females (39%). Pearson chi-square value - 0.00; p 0.996 > 0.05; the results are statistically not significant.
Table 2. Table revealing the results of Chi – Square test between timing and arch of alveoloplasty with p-value 0.113>0.05 which is not significant.
Table 3. Table revealing the results of Chi-square test between Gender and Timing of alveoloplasty with p-value 0.996>0.05 [*statistically not significant].
The state of complete edentulism is influenced by a lot of etiological factors like diet, age, lifestyle, systemic illness, etc, [10]. Complete edentulism puts the patient into many discomforts be it physical, physiological or psychological and some patients consider it to be disfiguring [11]. The incidence and prevalence of edentulism has been reported to be decreasing over the last 20 years in western countries according to Polzer et al. [12],. However, he also points out that in developing countries like India, its prevalence is about 19% at the age of 65-74 years.
This phenomenon of complete edentulism is treated with the help of complete dentures, which can be overdentures (Tooth supported / Tissue supported) or tissue supported complete dentures. In Spite of the advent of implants, a conventional tissue supported complete denture remains a common clinical procedure [11, 13]. The complete denture delivered to a patient must be retentive, stable, aesthetic and also in harmony with supporting hard and soft tissues [14]. Under some conditions, due to errors in denture construction, this harmony is not achieved leading to discomfort and complaints upon wearing dentures. According to Bilhanet al., [15], loose fitting dentures, instability and food accumulation were the most reported problems among denture wearers (p<0.001).
The pre prosthetic evaluation and mouth preparation plays a significant role in avoiding such problems. The etiological factors leading to unstable dentures, denture sores, etc. [16], can be related to hard tissues or soft tissues [17]. Those associated with soft tissues are: Flabby tissue, redundant tissue, frenal attachments and inadequate vestibular depth, while those related to hard tissues are bony prominences, irregular ridge contour, knife edge ridges and tori [18, 19]. The most important factor leading to hard tissue changes is the Residual Ridge Resorption, whose pattern is upward & inward in maxilla and downward & outward in mandible [20]. This RRR is also influenced by factors like systemic illness such as osteoporosis, where greater RRR and decreased masticatory performance post denture insertion has been observed by Singhal et al.,[21]. The presence of knife edged ridges and bony spicules also contributes to increased chances of discomfort, pain & ulceration and increases the rate of Residual Ridge Resorption.
Inorder to halt the process of residual ridge resorption, a complete denture is important with adequate pre prosthetic mouth preparation [22]. Johnston defines mouth preparation as a process that includes all operations to re-establish and maintain the harmony of supporting structures & ridge tissues and which make possible a simpler design of the prosthesis [23]. Among the pre prosthetic surgical procedures, alveoloplasty is the most common. It is a surgical procedure that offers to smooth or re-shape a patient's edentulous jaw bone. According to Ramkumar et al. [24], this procedure can have two fold significance: 1. When done along with extraction i.e. Immediate alveoloplasty, it allows establishment of a desired ridge contour during the healing of the extraction site itself. 2. If performed two days or week after extraction i.e. Delayed alveoloplasty, it optimizes the existing ridge contour to avoid complications during denture insertion. The prevalence of alveoloplasty in complete denture wearers in the current study was 26.6%, which matches with the results of a similar study by Jones et al. [25], where approximately one third of complete denture patients (33.3%) underwent alveoloplasty followed by immediate dentures.
No literature evidence exists about the timing of alveoloplasty - delayed/immediate. This timing is of significant importance because of the following reasons: in case of immediate alveoloplasty, the bony spicules are removed immediately following extraction using bone rongeurs and the extraction socket is compressed using finger pressure, facilitating a smooth healing with desirable ridge contour. In case of delayed alveoloplasty, after healing of the extraction site, an incision along the crest of the alveolus is given and a full flap is elevated. The bone is recontoured using a rongeur or bone file or a handpiece with bur [26]. The major disadvantage of this technique is the need for multiple surgical appointments.
However, in the current study, delayed alveoloplasty has a higher prevalence percentage, 83% (n=83), which is of critical concern. A school of thought that exists in association with the increased number of delayed alveoloplasty is that, with the advent of implant supported prosthesis, clinicians don't prefer compression of extraction sockets in order to preserve the ridge width. In a study by Michael and Barosum [26, 27], a simple tooth extraction preserved much of the residual ridge than a labial plate by intraseptal alveoloplasty. A newer technique of alveoloplasty (delayed) has been devised by Klein, who suggests creation of grooves in the ridge in the molar region, enhancing denture retention, as pointed out by Behrman [28].
The current study couldn't establish a significant association between gender and the timing of alveoloplasty (p-value > 0.05). However, a male predilection, 53% (n=53), exists for alveoloplasty procedures which can be attributed to the difference in bone pattern and bone density in males compared to females.The entire significance and purpose of the study is to bring out the prevalence of alveoloplasty procedures in complete denture patients, in order to avoid post insertion problems like decreased masticatory ability and associated problems being most common in ill-fitting dentures as pointed by Bosman et al. [29], and L. Laurina et al., [30]. A proper fitting denture not only contributes to patient satisfaction but also improves their quality of life [31].
In the current study, large numbers of alveoloplasties were of the delayed type and required a second surgical procedure. This can be avoided in the future and focus should be directed towards performing alveoloplasties immediately post extraction, so that healing can take place harmoniously along with that of the extraction socket.
Conclusion
Within the limits of the study, it can be concluded that there was
a higher prevalence of male population undergoing alveoloplasty
procedure prior to complete denture construction, which can be
attributed to the difference in the bone pattern and bone density
in males when compared to females. Considering the timing of
alveoplasty,there is a high need for early alveoloplasty carried out
on the same day of extraction to avoid multiple surgical appointments.
Authors Contributions
First author (Kalyani. P) performed the analysis, and interpretation
and wrote the manuscript. Second author (Dr. Jessy P) and
Third author (Dr. Subhabrata Maiti) contributed to conception,
data design, analysis, interpretation and critically revised the manuscript.
Fourth author (Dr. M. P. Santhosh Kumar) participated in the study and revised the manuscript. All the four authors have
discussed the results and contributed to the final manuscript.
Acknowledgement
This study was supported by Saveetha Dental College and Hospitals,
Saveetha Institute of Medical and Technical Sciences,
Saveetha University.
References
- Jain AR, Nallaswamy D, Ariga P, Ganapathy DM. Determination of correlation of width of maxillary anterior teeth using extraoral and intraoral factors in Indian population: A systematic review. World J Dent. 2018 Jan; 9: 68-75.
- Papadaki E, Anastassiadou V. Elderly complete denture wearers: a social approach to tooth loss. Gerodontology. 2012 Jun; 29(2): e721-7. PMID: 21916954.
- Jyothi S, Robin PK, Ganapathy D. Periodontal health status of three different groups wearing temporary partial denture. Research Journal of Pharmacy and Technology. 2017; 10(12): 4339-42.
- Duraisamy R, Krishnan CS, Ramasubramanian H, Sampathkumar J, Mariappan S, Navarasampatti Sivaprakasam A. Compatibility of Nonoriginal Abutments With Implants: Evaluation of Microgap at the Implant-Abutment Interface, With Original and Nonoriginal Abutments. Implant Dent. 2019 Jun; 28(3): 289-295. PMID: 31124826.
- Selvan SR, Ganapathy D. Efficacy of fifth generation cephalosporins against methicillin-resistant Staphylococcus aureus-A review. Research Journal of Pharmacy and Technology. 2016; 9(10): 1815-8.
- Ganapathy D, Sathyamoorthy A, Ranganathan H, Murthykumar K. Effect of Resin Bonded Luting Agents Influencing Marginal Discrepancy in All Ceramic Complete Veneer Crowns. J Clin Diagn Res. 2016 Dec; 10(12): ZC67-ZC70. PMID: 28209008.
- Subasree S, Murthykumar K. Effect of Aloe Vera in Oral Health-A Review. Research Journal of Pharmacy and Technology. 2016; 9(5): 609-12.
- Bhuskute MV, Shet RG. Preprosthetic surgery: An adjunct to complete denture therapy. Journal of the International Clinical Dental Research Organization. 2019 Jan 1; 11(1): 49.
- Neumeier TT, Neumeier H. Digital immediate dentures treatment: A clinical report of two patients. J Prosthet Dent. 2016 Sep; 116(3): 314-9. PMID: 27061629.
- Ranganathan H, Ganapathy DM, Jain AR. Cervical and Incisal Marginal Discrepancy in Ceramic Laminate Veneering Materials: A SEM Analysis. Contemp Clin Dent. 2017 Apr-Jun; 8(2): 272-278. PMID: 28839415.
- Vijayalakshmi B, Ganapathy D. Medical management of cellulitis. Research Journal of Pharmacy and Technology. 2016; 9(11): 2067-70.
- Polzer I, Schimmel M, Müller F, Biffar R. Edentulism as part of the general health problems of elderly adults. Int Dent J. 2010 Jun; 60(3): 143-55. PMID: 20684439.
- Kannan A. Effect of Coated Surfaces influencing Screw Loosening in Implants: A Systematic Review and Meta-analysis. World. 2017 Nov; 8(6): 496-502.
- Ashok V, Suvitha S. Awareness of all ceramic restoration in rural population. Research Journal of Pharmacy and Technology. 2016; 9(10):1691-3.
- Bilhan H, Geckili O, Ergin S, Erdogan O, Ates G. Evaluation of satisfaction and complications in patients with existing complete dentures. J Oral Sci. 2013 Mar; 55(1): 29-37. PMID: 23485598.
- Ashok V, Nallaswamy D, Benazir Begum S, Nesappan T. Lip Bumper Prosthesis for an Acromegaly Patient: A Clinical Report. J Indian Prosthodont Soc. 2014 Dec; 14(Suppl 1): 279-82. PMID: 26199531.
- Venugopalan S, Ariga P, Aggarwal P, Viswanath A. Magnetically retained silicone facial prosthesis. Niger J Clin Pract. 2014 Mar-Apr; 17(2): 260-4. PMID: 24553044.
- Kannan A, Venugopalan S. A systematic review on the effect of use of impregnated retraction cords on gingiva. Research Journal of Pharmacy and Technology. 2018; 11(5): 2121-6.
- Basha FY, Ganapathy D, Venugopalan S. Oral Hygiene Status among Pregnant Women. Research Journal of Pharmacy and Technology. 2018; 11(7): 3099-102.
- Devaki VN, Balu K, Ramesh SB, Arvind RJ, Venkatesan. Pre-prosthetic surgery: Mandible. J Pharm Bioallied Sci. 2012 Aug; 4(Suppl 2): S414-6. PMID: 23066301.
- . Singhal S, Chand P, Singh BP, Singh SV, Rao J, Shankar R, et al. The effect of osteoporosis on residual ridge resorption and masticatory performance in denture wearers. Gerodontology. 2012 Jun; 29(2): e1059-66. PMID: 22229790.
- Ajay R, Suma K, Ali SA, Kumar Sivakumar JS, Rakshagan V, Devaki V, et al. Effect of Surface Modifications on the Retention of Cement-retained Implant Crowns under Fatigue Loads: An In vitro Study. J Pharm Bioallied Sci. 2017 Nov; 9(Suppl 1): S154-S160. PMID: 29284956.
- Bilhan H. Preparation of the mouth for removable partial dentures. In Removable partial dentures 2016; 53-61. .
- Ramkumar V. Preprosthetic Surgery [Internet]. Viva in Oral Surgery for Dental Students. 2012; 122–122.
- Jones PM, Nakayama LK. Surgical experiences of complete denture patients. J Prosthet Dent. 1967 Jul; 18(1): 12-8. PMID: 5229664.
- Ephros H, Klein R, Sallustio A. Preprosthetic Surgery. Oral Maxillofac Surg Clin North Am. 2015 Aug; 27(3): 459–72.
- Michael CG, Barsoum WM. Comparing ridge resorption with various surgical techniques in immediate dentures. J Prosthet Dent. 1976 Feb; 35(2): 142-55. PMID: 1061808.
- Behrman SJ. Surgical preparation of edentulous ridges for complete dentures. Journal of Prosthetic Dentistry. 1961 May 1; 11(3): 404-13.
- Slagter AP, Olthoff LW, Bosman F, Steen WH. Masticatory ability, denture quality, and oral conditions in edentulous subjects. J Prosthet Dent. 1992 Aug; 68(2): 299-307. PMID: 1501179.
- Laurina L, Soboleva U. Construction faults associated with complete denture wearers' complaints. Stomatologija. 2006; 8(2): 61-4. PMID: 16861852.
- Mayun IG, Indrasari M, Soetanto MF. Relationship between patient’s satisfaction of removable denture wearers and oral health-related quality of life. International Journal of Applied Pharmaceutics. 2017 Dec 1; 9(Special Issue 2): 150-4.