Does the Number of Attempts of Endotracheal Intubation Influence the Incidence of Post-Extubation Dysphagia in Patients Undergoing Maxillofacial Surgical Procedures? - A Prospective Analysis
Rajesh P1, Prakyatha Brasanna Shetty2, Vaishali V2*
1 Professor and Head, Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, India.
2 Post Graduate, Department of Oral and Maxillofacial Surgery, Chettinad Dental College and Research Institute, India.
*Corresponding Author
Dr.Vaishali. V,
Department of Oral and Maxillofacial surgery, Chettinad Dental College and Research Institute, Kelambakkam, Chennai- 603103, India.
Tel: 8056379290, 8838017051
E-mail: vaish712.venkat@gmail.com
Received: August 16, 2020; Accepted: September 11, 2020; Published: October 22, 2020
Citation:Rajesh P, Prakyatha Brasanna Shetty, Vaishali V. Does the Number of Attempts of Endotracheal Intubation Influence the Incidence of Post-Extubation Dysphagia in Patients Undergoing Maxillofacial Surgical Procedures? - A Prospective Analysis. Int J Dentistry Oral Sci. 2020;7(10):860-863. doi: dx.doi.org/10.19070/2377-8075-20000170
Copyright: Vaishali V©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: To evaluate the incidence and association of post-extubation dysphagia (PED) with varying number of attempts of endotracheal
intubation in patients undergoing maxillofacial surgical procedures.
Settings: One of the unnoticed complications of endotracheal intubation, yet with tragic consequences is post-extubation dysphagia.
In a post maxillofacial surgical patient, this is masked by the extensiveness of the surgery and the immobilization protocols
and hence need to be attended with utmost care.
Materials and Methods: A two-year prospective analysis of patients undergoing maxillofacial surgical procedures for varied
cause was done. Data regarding age, gender, medical history, indication for surgery, pre-anaesthetic evaluation, intraoperative records
related to the number of intubation attempts and any complications associated and a water swallow test to test for PED 24
hours after surgery were recorded and subjected to statistical analysis.
Results: Mean age of the population was 35.1 years and was predominantly male. About 62.5% of them were intubated by fiberoptic
intubation, 35% by naso-endotracheal and 5% by oro-endotracheal intubation.65% of them were intubated more than once
and a maximum of 7 attempts was done to secure the airway. 19 patients had PED and it was significantly associated with the
number of attempts of intubation with p<0.001.
Conclusion: PED is the tip of the iceberg and could indicate a serious underlying complication that could result in fatal complications
if neglected and thus alarms the surgeon to watch out closely and address accordingly.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.Conclusion
7.Refereces
Keywords
Dysphagia; Maxillofacial Surgery; Endotracheal Intubation; Airway.
Introduction
Endotracheal intubation is the choice of securing the airway during
surgical procedures under general anaesthesia. Intubation in
patients indicated for oral and maxillofacial surgical procedures
are quite challenging and different from others. Often difficult intubation
is anticipated with increased extensiveness of the injuries
or pathology and failure of intubation in the first attempt is not
so uncommon. But the post extubation complications associated
as a result has to be attended with care to avoid flare-ups of unnecessary
consequences. One such complication is post extubation
dysphagia especially in maxillofacial surgical patients which in
combination with post-surgical immobilization of the jaw keeps
any serious complications like aspiration pneumonia latent. This
study aims to throw some light on the importance of addressing
the dysphagia in post-surgical patient and to evaluate its incidence
with difficulty in intubation.
Materials and Methods
A prospective analysis of 40 patients who reported to the outpatient
department, and emergency department of our institution
from November 2017 to November 2019 seeking surgical
management of maxillofacial injuries, pathologies and orthognathic
surgeries under general anaesthesia. Ethical clearance was
obtained from the Institutional Human Ethics Committee and
informed consent was obtained from the patients before the surgery.
Patients indicated for Open reduction and internal fixation of various maxillo-mandibular fractures, space infections, surgical
removal of pathologies like cyst enucleation, tumour resection,
cleft repair and removal of temporomandibular joint ankylosis
and those requiring jaw correction surgeries i.e. orthognathic surgeries
were included in the study. Those patients falling under the
categories ASA III and ASA IV, those with surgical airway and
known cases of obstructive and restrictive lung disorders were
excluded from the study. After obtaining informed consent, demographic
details, reason for the indication of surgery, complete
pre-anaesthetic evaluation, intraoperative records of the type of
intubation chosen and the number of attempts for successful intubation,
any other intraoperative complications associated and
incidence of post extubation dysphagia that was recorded with
water swallowing test 24 hours after the surgery. The endotracheal
intubation was performed by the experienced and skilled
anaesthesiologist of our institution. All the data were recorded
and subjected to statistical analysis.
The collected data were analysed with IBM.SPSS statistics software
21.0 Version. Frequency distribution was calculated for categorical.
Descriptive statistics were calculated for numerical data.
Independent t test was used to find the significance and correlation
between variables. In all the above statistical tools the probability
value .05 is considered as significant level.
Results
A total of 40 patients were enrolled in the study. About 82.5%
(n=33) of them were males and 17.5% (n=7) were females. Mean
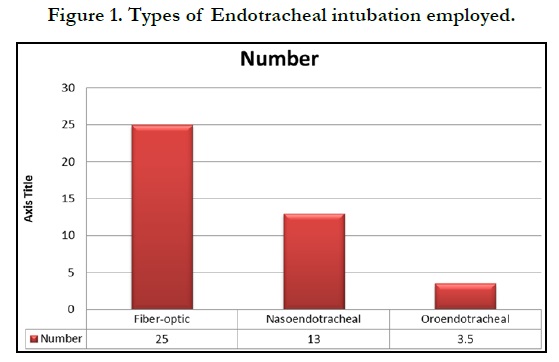
age of the population was 35.1 years. Figure 1 depicts the frequency
of the type of intubation chosen.
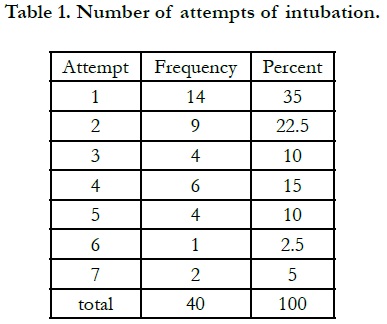
Fiber-optic intubation was the highest used with 62.5% (n= 25), followed by direct nasal intubation in 32.5% (n=13) and finally orotracheal intubation in 5% (n= 2). Table 1 shows the number of attempts used for successful intubation. About 35% (n=14) of the population was intubated successfully in the first attempt, 22.5% (n=9) in their second attempt, 15% (n= 6) in the fourth attempt and 10% (n=4) in the third attempts and rest of them had five attempts and more for successful intubation.
47.5% (n=19) of them were found to have post extubation dysphagia when screened 24 hours after surgery. When the number of intubation attempts and incidence of post-extubation dysphagia was correlated, there existed a positive correlation between both, and it was statistically significant with p<0.001.
Discussion
Securing the airway during maxillofacial procedures is peculiar
from others due to the shared regional anatomy of both. It is
because the maxillofacial injuries have direct impact on the respiratory
tract thereby injuring it as in case of trauma or indirectly
restricting the access due to limited mouth opening or obstructive
nature of the pathology or the tissue injury. This poses a challenge
to the anaesthesiologist to carry out detailed examination of
the upper respiratory tract to opt for the indicated method of securing
the airway. Also, they are not left with the freedom of manipulation
and mobilization of the maxillofacial structures during
examination or intubation due to the extensiveness of the injury
or pathology and due to immobilization protocols to be followed
based on the surgical plan. Prior to the surgical procedure, a thorough evaluation of the patient is mandatory that includes LEMON
assessment - external predictors of the difficult airway that
measures the length of the neck, thyromental distance, atlantoaxial
mobility, Mouth opening, Mallampati classification, and any
obstructed airway seen as stridor and neck mobility [1]. In cases
of maxillofacial trauma, the extent of the fracture, mobile bony
segments, the elevated floor of the mouth, soft tissue edema, and
loose teeth with the risk of aspiration, CSF leak, limited mobility
due to muscle spasm and, in case of any pathology, its extent,
swelling or ulceration, maximum mouth opening, obstructed airway
should be noted and based on the evaluation difficulty of
intubation should be anticipated. Thus the choice of intubation
in maxillofacial surgical procedures is always a team approach and
involves various factors that determine the success of intubation.
Every method of intubation has its indications and contraindications.
However endotracheal intubation either nasal or oral way,
remains the standard way of securing the airway [2]. But limited
mouth opening in maxillofacial surgical patient disables direct
visualization of vocal cords which is a pre-requisite for successful
endotracheal intubation. In such cases, awake fiber-optic intubation
is preferred that enables the anaesthesiologist to visualize the
vocal cords indirectly. The disadvantage that entails this method
is obscuring of vision by salivary secretions and blood but the
failure of intubation is minimal than the other direct techniques
and especially when the mouth opening is compromised. Method
of intubation and its success has important clinical implications.
Complications that results from the endotracheal intubation could
be major or minor [3]. Major complications include granulomas,
laryngeal ulceration or vocal cord injury including paralysis while
minor complications include sore throat, laryngeal edema, stridor
and dysphagia. The severity of complications depends on the
selection of the tube, proper instrumentation and placement of
the tube, number of attempts for successful intubation, duration
of intubation, pre-existing injuries to the airway and extubation
related. One important complication that often goes unnoticed
is the post extubation dysphagia that indicates more serious systemic
issues in a post-operative patient [4].
Post extubation dysphagia is defined as the inability or difficulty
to effectively and safely transfer food and liquid from the mouth
to the stomach after extubation. Clinically it is defined as the inability
to drink 50ml of water within 48 hours of extubation. Leder
et al reported a higher incidence of PED in trauma and critically
ill patients intubated endotracheally for mechanical ventilation
[5]. Multifactorial causation of PED has been described including
mechanical causes, cognitive disturbances and residual effects
of the drugs. Mechanical injury due to improper size of the tube
and prolonged intubation causes mucosal inflammation leading to
loss of architecture, atrophy of the muscles if prolonged, reduced
proprioception and reduced laryngeal circulation. Any dysregulation
in the swallowing reflexes due to neuromuscular disorders or
cognitive impairment due to traumatic brain injury significantly
contributes to PED. Those with neuromuscular disorders, low
Glasgow coma scores, severely injured, old age, prolonged ventilation,
forced supine position, head and neck pathologies, placement
of nasogastric tube adds risk to developing PED. Bordon
et al reported from his study in trauma patients that with every
added day of intubation of the patient, 14% rise in the risk of incidence
of PED and patients who were 55 years of age and above
had 37% increased risk. Macht et al., [6] proposed six mechanisms
to be etiological for PED in post-extubation patients:
1) Direct trauma to the anatomy of the throat (vocal cords, tongue
base, epiglottis, arytenoids by endotracheal or tracheostomy tubes
2) Muscular weakness due to nerve and muscle damage (disuse
atrophy; critical illness neuropathy and myopathy
3) Loss of normal sensation in the oropharynx and larynx
4) Impaired sensorium generally (delirium, sedation)
5) Gastroesophageal reflux
6) Out-of-sync breathing and swallowing in people with tachypnea
before and/or after extubation.
Undiagnosed dysphagia in post-extubation patients leads to bronchoaspiration
and related complications like pneumonia, malnutrition,
increased hospital stay and thereby interferes the recovery
period of the patient. Sassi et al reported that 50% of the patients
with difficult or prolonged intubation that presented with postextubation
dysphagia developed broncho-aspiration7. Such scenario
gets worse in a maxillofacial patient due to the overt influence
of other factors like static immobilized jaw, pain and swelling
with alternative route of nutrition that narrows the focus of the
patient and the surgeons during the first few days after surgery.
Meanwhile in rare occasions, if the respiratory and pharyngeal
complications are not treated results in catastrophic complications
leading to morbidities and mortalitites.
A number of methods are in use to diagnose PED [7]. Commonly
used method is the bedside evaluation (BSE) by a speech
pathologist. It is a multifaceted test comprising of an interview,
clinical assessment of respiratory tract and functional changes if
any. Another most often employed screening test for dysphagia is
the water swallow test [8]. When the severity of the condition has
to be graded, various other instrumental tests are preferred. Video
fluoroscopic swallow study (VFSS), Fiberoptic endoscopic evaluation
of swallowing, Ultrasonography, pH manometry and scintigraphy.
Of these VFSS and FEES are considered to be the gold
standard for diagnosis of PED as they portray a real time image
of various deglutition stages which aids in the accurate diagnosis
and prompt management of the condition [3]. In maxillofacial
surgical patients it is mandatory to check for the incidence of
PED post-surgically. In many instances PED is either unnoticed
due to the extensiveness of the surgery or masked by the jaw
immobilization protocols. The same reason calls for alternative
methods of nutrition to not interfere in the healing of the surgical
wound. By the time the patient reverts to oral intake, any minor
injuries to the pharynx would have healed and thus passes unseen.
This study intended to uncover the latent threat of the PED, even
if rare, and highlight the importance of thorough examination of
the patient during the post surgical period to watch out for any
signs and symptoms of PED though could be indicating an ongoing
aspiration pneumonia or related complications.
In our study, the mean age group of the population was 35.1 years
and the gender was predominantly male. This relieves the influence
of age on the incidence of dysphagia thereby eliminating
the confounding bias. Fiber-optic intubation was the frequently
chosen method of intubation (62.5%) followed by direct nasoendotracheal
intubation (35%) and finally by the oro-endotracheal
intubation. This differs from the results of the Sarasvat et al., and
Rashiuddin et al., where direct nasal intubation was the preferred
choice of intubation [9]. But this could be because those studies
involved only maxillofacial trauma while in our study patients
undergoing all types of maxillofacial surgical procedures were involved. Also the demographics, extensiveness of the etiology,
anticipated difficulty in airway and the anaesthesiologists’ preference
has a major role in the choice of airway. About 65% of
the patients were not intubated successfully in the first attempt.
22% had to be intubated twice, 15% four times and 10% three
times and the rest multiple times for a successful intubation. This
could be attributed again to the complexity of the injuries and
their obscurity to the evaluation. Significant proportion of the lot
developed PED (47.5%) and it had a strong positive correlation
with the number of failed attempts of intubation. Thus difficult
intubation could indicate potential complication of PED in the
post-surgical period.
Thus it is expected of every maxillofacial surgeon to express a
high index of suspicion during their evaluation for the symptoms
of PED to avoid unlikely complications. Knowledge of the attributes
of difficult airway, skills of managing the same, accurate
recognition of a failed airway is important while securing the airway
[10].
Conclusion
Post extubation dysphagia is not uncommon even in patients
without pre-existing pathologic states. Owing to the life threatening
consequences that could occur if PED is neglected, every
maxillofacial surgeon to monitor the patient closely. The risk of
dysphagia escalates with increased attempts of endotracheal intubation
and it should alarm the surgeon to anticipate PED and
watch out for the same to effectively manage the condition.
References
- Raval CB, Rashiduddin M. Airway management in patients with maxillofacial trauma - A retrospective study of 177 cases. Saudi J Anaesth. 2011; 5(1): 9-14. PMID: 21655009.
- Barak M, Bahouth H, Leiser Y, Abu El-Naaj I. Airway Management of the Patient with Maxillofacial Trauma: Review of the Literature and Suggested Clinical Approach. Biomed Res Int. 2015; 2015: 724032. PMID: 26161411.
- Tay JYY, Tan WKS, Chen FG, Koh KF, Ho V. Postoperative sore throat after routine oral surgery: influence of the presence of a pharyngeal pack. British Journal of Oral and Maxillofacial Surgery. 2002; 40(1): 60–63.
- Rassameehiran S, Klomjit S, Mankongpaisarnrung C, Rakvit A. Postextubation Dysphagia. Proc (Bayl Univ Med Cent). 2015 Jan; 28(1):18-20. PMID: 25552788.
- Leder SB, Cohn SM, Moller BA. Fiberoptic endoscopic documentation of the high incidence of aspiration following extubation in critically ill trauma patients. Dysphagia. 1998; 13(4): 208–212. PMID: 9716751.
- Macht M, Wimbish T, Clark BJ, Benson AB, Burnham EL, Williams A, et al. Postextubation dysphagia is persistent and associated with poor outcomes in survivors of critical illness. Crit Care. 2011; 15(5): R231. PMID: 21958475.
- Medeiros Gisele Chagas de, Sassi Fernanda Chiarion, Mangilli Laura Davison, Zilberstein Bruno, Andrade Claudia Regina Furquim de. Clinical dysphagia risk predictors after prolonged orotracheal intubation. Clinics (Sao Paulo). 2014; 69( 1 ): 8-14. PMID: 24473554.
- Tsai MH, Ku SC, Wang TG, Hsiao TY, Lee JJ, Chan DC, et al. Swallowing dysfunction following endotracheal intubation: Age matters. Medicine (Baltimore). 2016; 95(24): e3871. PMID: 27310972.
- Saraswat V. Airway management in Maxillofacial trauma: A Restrospective Review of 127 cases. Indian J Anaesth. 2008; 52: 311-6.
- Skoretz SA, Flowers HL, Martino R. The Incidence of Dysphagia Following Endotracheal Intubation. Chest. 2010; 137(3): 665–673. PMID: 20202948.