Obstructive Sleep Apnea - A Review
Melvin George1, Madhulaxmi Marimuthu2*
1 Fellow in Orthognathic Surgery, Department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospitals, Saveetha Institute of Medical
and Technical Sciences, Saveetha University, Poonamallee High Road, Vellappanchavadi, Chennai, Tamil Nadu, India.
2 Professor, Department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences,
Saveetha University, Poonamallee High Road, Vellappanchavadi, Chennai, Tamil Nadu, India.
*Corresponding Author
Madhulaxmi Marimuthu MDS,
Professor, Department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, No 162, Poonamallee High Road, Vellappanchavadi, Chennai-600077, Tamil Nadu, India.
Tel: +91-73738-14000
E-mail: madhulaxmi@saveetha.com
Received: July 25, 2020; Accepted: September 11, 2020; Published: October 08, 2020
Citation:Melvin George, Madhulaxmi Marimuthu. Obstructive Sleep Apnea - A Review. Int J Dentistry Oral Sci. 2020;7(10):849-851. doi: dx.doi.org/10.19070/2377-8075-20000167
Copyright: Madhulaxmi Marimuthu©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Obstructive sleep apnea (OSA) is a common sleeping disorder. As the name suggests, it is associated with apneic and hypopneic breathing due to some kind of obstruction in the respiratory passage and thereby interferes with sleep. This review aims to give a concise overview on the disease, its pathophysiology, clinical presentation, diagnosis and various methods of management.
2.Introduction
3.Pathophysiology
4.Clinical Manifestation
5.Diagnosis of OSA
6.Polysomnography
7.Portable monitoring
8.Treatment
9.Positional Therapy
10.Oral Appliances
11.Surgical management
12.Weight control
13.Educational and behavioural intervention
14.References
Keywords
Obstructive Sleep Apnea; Airway; Polysomnography; Medical; Surgical; Management
Introduction
Obstructive sleep apnea (OSA) is an increasingly common,
chronic sleep-related breathing disorder which is characterized by
periodic narrowing and obstruction of the pharyngeal airway during
sleep [1, 2]. Untreated OSA can be associated with metabolic
disorders, cardiovascular disease, cognitive impairement, depression,
loss of productivity in workplace and motor vehicle accidents
[3]. The causes and consequences of OSA vary between
patients. Most patients with OSA are undiagnosed and untreated
which might be related to lack of awareness about the disorder [4,
5]. Early detection of OSA can result in greatly improved quality
of life along with reduction of systemic morbidities.
Pathophysiology
OSA is characterized by recurrent collapse of pharyngeal airway
during sleep, resulting in substantially reduced or complete cessation
of airflow despite ongoing breathing efforts These disturbances
lead to intermittent hypercapnia and hypoxia and surges
in sympathetic activation. The culmination of a respiratory event
leads to brief awakening from sleep. These events result in a cyclical
breathing pattern and fragmented sleep as the patient oscillates
between wakefulness and sleep. Each respiratory event can last 20 to 40 seconds [6].
During wakefulness, OSA patients compensate for compromised
airway through protective reflexes to increase upper airway dilator
muscle activity to maintain patency of airway [7]. Obstructive
sleep apnea occurs due to anatomic factors that cause pharyngeal
narrowing which include large neck circumference, cervical soft
tissue, vessels and bony structures. Many of these factors cause
pharyngeal collapse by decreasing the caliber of the upper airway
or by increasing the upper airway surrounding pressurewhich happens
during Rapid Eye Movement (REM) sleep when protective
reflexes to maintain upper airway is lost, leading to a period of
hyponea or apnea [8].
Clinical Manifestation
Symptoms of OSA include, snoring, excessive daytime sleepiness,
choking or gasping at night, night sweats, neurocognitive impairment,
heartburn, morning headaches, maintenance insomnia,
erectile dysfunction and nocturia [9]. Snoring due to redundant
pharyngeal muscles can be an early symptom of OSA. This proceeds
to episodes of apnea leading to excessive daytime sleepiness
which is usually the first complaint given by the patient. These
patients become somnolent in passive situations or during monotonous
activities such as watching television, reading books, or during a long drive. If the aforementioned problem occurs despite
getting adequate amount of sleep during the preceding night
the patient may have a problem with quality of his/her sleep [10].
The symptoms of OSA are the result of sleep disturbance which
will in most cases be unnoticed by the patient.
Clinical fiindings in OSA patients will be obesity, enlarged neck
circumference, crowded upper airway, hypertension, accentuated
P2 heart sounds, retrognathia, nalsa obstruction, decreased oxygen
saturation, S3 heart sound, lower extremity edema (heart failure)
[9].
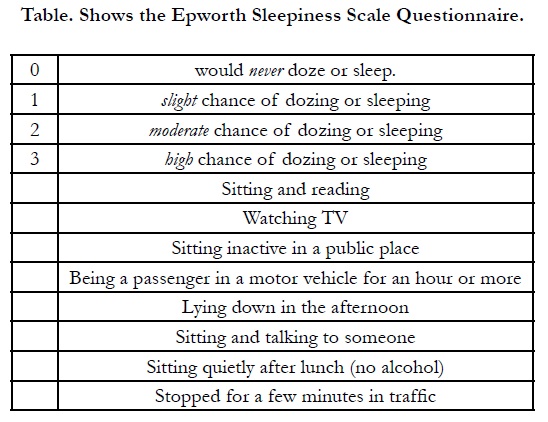
Diagnosis of OSA
The clinician should search for clinical features that are listed in
Epworth Sleepiness Scale Questionnaire. Having ≥ 2 of those
symptoms indicate the need for further assessment or a sleep
study.
The patient should choose one of the 0-3 numbers as described
below in the recent two weeks. Scores greater than 10 out of 24
are regarded as presence of daytime sleepiness.
Polysomnography
Overnight polysomnography is the gold-standard diagnostic test
for OSA. Patients who are diagnosed with OSA and choose continuous
positive airway pressure (CPAP) therapy are then brought
back for follow up study, during which the pressure of CPAP
device is titrated. Alternatively those two studies can be done in
selected patients over one night, followed by a “split-night protocol”.
The two parts of the split night study complement each
other; diagnosis of OSA is made during the first part, followed by titration of CPAP during the second half of the study. If there
are more than 20 respiratory events per hour in the first half of
the study in a patient with a high pre-test probability (having two
or more clinical features), or ≥ 40 respiratory events in a patient
with a pretest low-probability, splitting the study is recommended.
Starting CPAP titration during the same night sleep study is timeand
cost effective while expediting delivery of treatment to the
patients. It should be noted that the first half of the split night
sleep study has to have at least 2 hours of recorded sleep data.
A negative polysomnogram does not exclude diagnosis of OSA
particularly in high-risk patients. In such patients repeating the
polysomnogram should be considered.
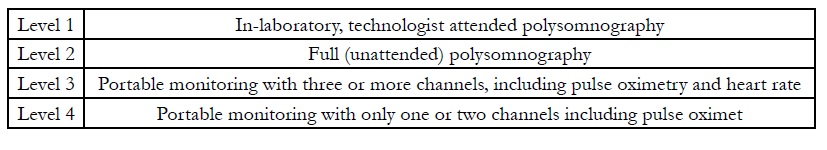
Portable monitoring
There are a variety of devices that are used for in-home, portable
monitoring of cardiorespiratory parameters. An effective portable
monitor requires at least three channels to asses airflow, thoracoabdominal
movements, and blood oxygenation [12]. In general
the sensitivity and specificity of these devices seem to be high
in populations at high risk for OSA assuming there are no other
comorbid medical or sleep disorders. Clinical practice guidelines
from the American Academy of Sleep Medicine (AASM) indicate
that portable monitoring may be used as an alternative to
polysomnography to diagnose OSA in patients with a high pretest
probability of moderate to severe OSA [13]. Portable monitoring
should not be used if another sleep disorder is suspected
or the patient has comorbid medical conditions that predispose
to non-OSA sleep related breathing disorders. These comorbid
conditions include, but are not limited to, moderate to severe pulmonary
diseases, neuromuscular diseases, congestive heart failure,
movement disorders, parasomnias, sleep seizures, etc.
Continuous PAP (CPAP), generally administered through the
nose (nCPAP), is undoubtedly considered the gold standard treatment
for OSA. Since its invention in 1983 by Dr Sullivan, the
clinical application of this device has deeply modified the course
of the disease over the last three decades, offering to thousands
of patients the first noninvasive method to control their disorder
[14]. Worldwide, nCPAP is constantly recommended as the firstchoice
treatment for patients with moderate to severe OSA.
Positional Therapy
The supine position, mainly due to the effect of the gravity on
tongue and soft palate position, is generally associated with an
increased number of apnoeas/hypopnoeas.
If postural OSA is diagnosed, patients can benefit from a positional
therapy (PT), which should prevent them from sleeping in
the supine posture. Many PT strategies are available. These include
the simple ‘tennis ball technique’, consisting of a tennis ball
strapped to the back to discourage supine position, supine alarm
devices and a number of positional pillows [15].
Oral Appliances
The most commonly used oral appliances are mandibular advanced
splints (MAS). These devices attach to both the upper and
lower dental arches in order to advance and retain the mandible
in a forward position. This will relocate laterally the pharyngeal
fat pads from the airway and the tongue base will move forward.
Consequently, the upper airway will be widened, particularly in its
lateral dimension, and the function of upper airway dilator muscles,
particularly the genioglossus, will improve.
Surgical management
Patients with OSA generally have excessive tissue in the oropharyngeal
tract. Uvulo-palatopharyngoplasty (UPPP), either
conventional or laser assisted (LAPP), is a widely established surgical
procedure for the treatment of OSA in selected patients.
This technique consists of the resection of uvula, part of the
soft palate and tissue excess in the oropharynx, and is usually performed
with simultaneous tonsillectomy.
Maxillomandibular advancement (MMA) is obtained by osteotomy
of the maxilla and mandibular. The advancement of the
skeleton structures passively induces an anterior displacement of
the soft palate and the tongue with a simultaneous widening of
the pharyngeal space.
Weight control
Obesity is an important risk factor for OSA and over 70% of patients
with OSA have obesity; a strict correlation has been documented between body mass index (BMI) and AHI. Weight loss
is therefore a main goal in the management OSA and all patients
should be encouraged to control their weight. Bariatric surgery
offers a good option of weight loss if conventional methods fail.
Educational and behavioural intervention
Educational and behavioural interventions represent the first step
in approaching patients with OSA, independently from the treatment
chosen. Patients should be instructed to avoid risk factors
such as smoking, drinking alcohol (particularly in the evening),
using sedatives and hypnotics.
References
- Heinzer R, Vat S, Marques-Vidal P, Marti-Soler H, Andries D, Tobback N, et al. Prevalence of sleep-disordered breathing in the general population: the HypnoLaus study. Lancet Respir Med. 2015 Apr;3(4):310-8. PubmedPMID: 25682233.
- Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008 Feb 15;5(2):136-43. PubmedPMID: 18250205.
- Osman AM, Carter SG, Carberry JC, Eckert DJ. Obstructive sleep apnea: current perspectives. Nat Sci Sleep. 2018 Jan 23;10:21-34. PubmedPMID: 29416383.
- Appleton SL, Vakulin A, McEvoy RD, Vincent A, Martin SA, Grant JF, et al. Undiagnosed obstructive sleep apnea is independently associated with reductions in quality of life in middle-aged, but not elderly men of a population cohort. Sleep and Breathing. 2015 Dec 1;19(4):1309-16.
- Simpson L, Hillman DR, Cooper MN, Ward KL, Hunter M, Cullen S, et al. High prevalence of undiagnosed obstructive sleep apnoea in the general population and methods for screening for representative controls. Sleep Breath. 2013 Sep;17(3):967-73. PubmedPMID: 23161476.
- Eckert DJ, Malhotra A. Pathophysiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008 Feb 15;5(2):144-53. PubmedPMID: 18250206.
- Mezzanotte WS, Tangel DJ, White DP. Waking genioglossal electromyogram in sleep apnea patients versus normal controls (a neuromuscular compensatory mechanism). J Clin Invest. 1992 May;89(5):1571-9. Pubmed PMID: 1569196.
- Sankri-Tarbichi AG. Obstructive sleep apnea-hypopnea syndrome: Etiology and diagnosis. Avicenna J Med. 2012 Jan;2(1):3-8. PubmedPMID: 23210013.
- Stansbury RC, Strollo PJ. Clinical manifestations of sleep apnea. J Thorac Dis. 2015 Sep;7(9):E298-310. PubmedPMID: 26543619.
- Foroughi M, Razavi H, Malekmohammad M, AdimiNaghan P, Jamaati H. Diagnosis of Obstructive Sleep Apnea Syndrome in Adults: A Brief Review of Existing Data for Practice in Iran. Tanaffos. 2016;15(2):70-74. Pubmed PMID: 27904537.
- Canadian Sleep Society, Blackman A, McGregor C, Dales R, Driver HS, Dumov I, et al . Canadian Sleep Society/Canadian Thoracic Society position paper on the use of portable monitoring for the diagnosis of obstructive sleep apnea/hypopnea in adults. Can Respir J. 2010 Sep-Oct;17(5):229-32. PubmedPMID: 21037998.
- Collop NA, Tracy SL, Kapur V, Mehra R, Kuhlmann D, Fleishman SA, et al. Obstructive sleep apnea devices for out-of-center (OOC) testing: technology evaluation. J Clin Sleep Med. 2011 Oct 15;7(5):531-48. PubmedPMID: 22003351.
- Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ, et al. Portable Monitoring Task Force of the American Academy of Sleep Medicine. Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2007 Dec 15;3(7):737-47.Pubmed PMID: 18198809.
- Sullivan CE, Berthon-Jones M, Issa FG. Nocturnal nasal-airway pressure for sleep apnea. N Engl J Med. 1983 Jul 14;309(2):112.PubmedPMID: 6343875.
- Frank MH, Ravesloot MJ, vanMaanen JP, Verhagen E, de Lange J, de Vries N. Positional OSA part 1: Towards a clinical classification system for positiondependent obstructive sleep apnoea. Sleep Breath. 2015 May;19(2):473-80. Pubmed PMID: 24943728.