Dental Involvement in a Child with Triple A Syndrome
Melek BD1*, Yacine R1, Mehdi D2, Badiaa J3
¹ Resident in Pediatric Dentistry, Dentistry Department, Hospital La Rabta, Tunis, Tunisia.
2 Orthodontist, Privative Practice, Faculty of Dental Medicine, Monastir, Tunisia.
3 Professor in Pediatric Dentistry, Head of Dentistry Department, Hospital la Rabta Tunis, Tunisia.
*Corresponding Author
Ben Daya Meleke
Resident in Pediatric Dentistry, Dentistry Department, Hospital La Rabta, Tunis, Tunisia.
Tel: 0021652001502
E-mail: bendaya.meleke@gmail.com
Received: May 26, 2017; Accepted: June 22, 2017; Published: June 30, 2017
Citation: Melek BD, Yacine R, Mehdi D, Badiaa J (2017) Dental Involvement in a Child with Triple A Syndrome. Int J Dentistry Oral Sci. 4(6), 498-502. doi: dx.doi.org/10.19070/2377-8075-1700098
Copyright: Melek BD©2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Allgrove (or triple A) syndrome is a rare autosomal recessive disorder. The triad consists of three most prominent features of the syndrome. First, Alacrimia (absence of tears). Second, achalasia (oesophageal motility disorder). Finally, adrenocorticotropic hormone (ACTH)-resistant adrenal insufficiency (Addison’s disease). The syndrome is caused by mutations in the AAAS gene on chromosome 12q13. Besides, Consistent oral findings could be noticed such as high arched palate, oral pigmentation, fissured or atrophic tongue and xerostomia.
Case Report: We report the case of a 12-year-old girl who presented at the oral department of hospital La Rabta (Tunisia) with specific dental abnormalities.
Conclusion: The aim of this report is to highlight dental involvement in Allgrove syndrome that could be of great clinical importance in both diagnosis and dental management.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.References
Keywords
Allgrove Syndrome; Triple A Syndrome; Oral Findings; Dental Management.
Introduction
The triple A syndrome (AAAS), also known as Allgrove syndrome (AS), is a very rare autosomal recessive disorder which was first identified in 1978. Although the incidence of AS is still unknown [1]. It has an estimated prevalence of 1 per 1,000,000 individuals [2]. About 200 cases have up to now been reported worldwide, showing a great variability in severity as well as in clinical manifestations [3].
The disease stands for the three most prominent features of the syndrome. Firstly, alacrimia (absence of tears). Secondly, achalasia (esophageal motility disorder) and thirdly, adrenocorticotropic hormone (ACTH)-resistant adrenal insufficiency. More global autonomic disturbances and peripheral neurologic manifestations could be detected. Thus, leading to recommend the name 4A syndrome.
A part from neurologic features patients may suffer from various abnormalities that consist of dermatologic abnormalities, osteoporosis, lack of eye lashes, poor wound healing added to nasal polyps [4].
The disease gene called the AAAS gene (achalasia-addisonianism alacrimia syndrome) was localized at 12q13 in 1996, which was mutant in individuals affected by this syndrome. This gene has an autosomal recessive inheritance. Besides it codes the protein Alacrimia Achlasia Adrenal insufficiency Neurologic disorder protien (ALADIN) [5]. This syndrome is characterized by significant allelic heterogeneity with more than 60 mutations previously identified according to the Human Gene Mutation Database [6].
Age at onset of symptoms is variable. Thus the disease has been classified into early and adult onsets based on the ages it manifests, either in childhood or after 30 years of age. The early onset disease usually presents with hypoglycemic episodes, hyperpigmentation or hypolacrimia. On the other hand, the adult onset disease has been reported to be more as neurological, with the endocrinologic or gastrointenstinal signs being minor [7].
The orofacial abnormalities of the Allgrove patients reported in the literature include the following ones: long narrow dysmorphic faces, long philtrum, down-turned mouth with thin upper lip, cleft palate, uncompletely developed fungiform papillae of the tongue, mandibular malocclusion, relaxed speech musculature, movable soft palate, high gothic hard palate, cross bite, macroglossia, fissured tongue, atrophic tongue and hyperpigmentation of the buccal mucosa, gums, lips and perioral area [5].
Case Report
The affected propositus is a female patient aged 12 years old. She had the classic triad of achalasia, alacrima and adrenal insufficiency (although no genetic analysis was done), and was thus diagnosed with Allgrove syndrome. She was referred to the Department of Oral Medicine, hospital La Rabta, Tunis, Tunisia, with the chief complaint of oral dryness, candida and teeth extensive demineralisation.
Family history revealed that both parents were healthy and had no prior history of neither adrenal insufficiency, alacrima, achalasia nor neurological or developmental problems. A history of the genetic disorder was not reported in relatives either. Furthermore, there was known evidence for a familial relationship between the parents, thus making consanguinity a likely explanation for Allgrove syndrome.
Alacrima is the earliest and the most consistent symptom, followed by glucocorticoid deficiency and achalasia [8]. Ophthalmologic evaluation and schirmer test revealed alacrimia. Our patient’s past medical history suggests that her alacrima had begun during childhood and artificial tears were then prescribed.
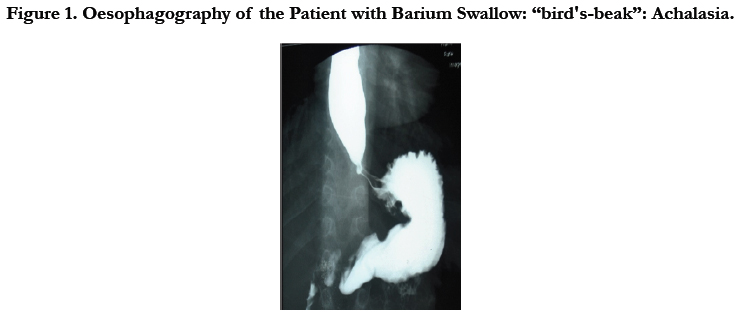
Oesophageal achalasia, however, is rare in children [9]. It consists in the absence of peristalsis within the body of the oesophagus and it is characterised by a relaxation defect in the gastro-oesophageal sphincter as well as a dilatation in the proximal oesophagus. Oesophagography of the patient with Barium swallow showed a narrowing in the cardio-oesophageal junction and a dilatation of the oesophagus proximal to the junction with “bird's-beak” tapering of the distal esophagus, which pointed to suspected achalasia (Figure 1). Consequently, progressive dysphagia, vomiting and feeding difficulties resulting in weight loss were found in our patient.
In AS, adrenal insufficiency known as Addison’s disease is typically diagnosed concurrently with or after achalasia detection [10]. Laboratory investigation revealed ACTH-resistant adrenocortical insufficiency with high plasma levels of ACTH, low levels of cortisol, hence, substitution treatment with hydrocortisone was commenced. Hydrocortisone, possessing both glucocorticoid and mineralocorticoid properties, is the treatment of choice in patients with adrenal insufficiency.
Subtle neurological particulary autonomic abnormalities can be detected at an early age. That leads to suggest the term of 4A and sometimes prescribe, as in the case of our patient, Tri B treatment (folic acid, vitamins B12 and B6) as prevention of neurologic disorder. The clinical interview with the patient revealed some associated neurologic symptoms. These symptoms include, at first sight, Mild cognitive dysfunction with a slight mental retardation, Dysautonomia, scholar difficulties reported by the parents, muscular weakness and visual impairment more precisely photophobia (Figure 2a).
Other than neurologic features patients may suffer from dermatologic abnormalities, osteoporosis, lack of eye lashes, poor wound healing and nasal polyps [4].
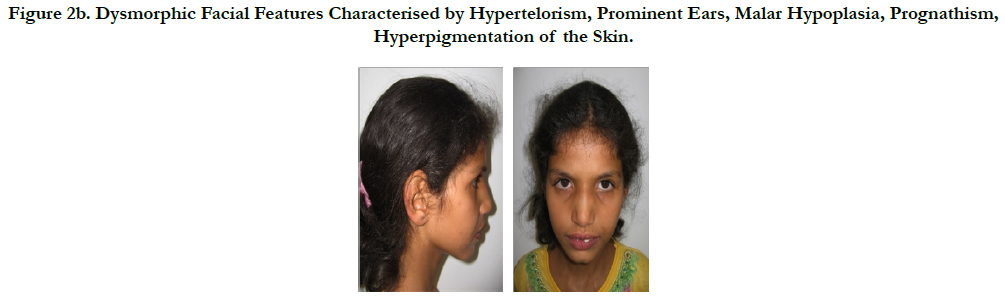
At the age of 12 years, the time of our first extra oral observation, the facial appearance revealed dysmorphic facial features. These are characterised by hypertelorism, prominent ears, malar hypoplasia, prognathism, asthenia, relaxed speech musculature, and dysarthria with nasal speech giving witness to velar insufficiency (Figure 2b).
Figure 2b. Dysmorphic Facial Features Characterised by Hypertelorism, Prominent Ears, Malar Hypoplasia, Prognathism, Hyperpigmentation of the Skin.
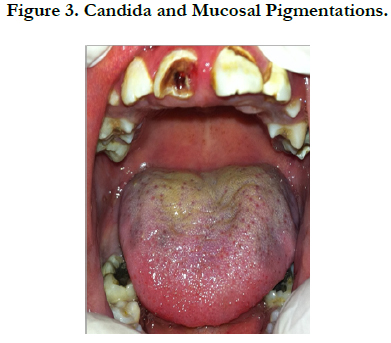
Careful intra oral examination in our case showed Xerostomia, candida infection and mucosal pigmentation on the dorsal surface of the tongue. Simultaneously found high rate of dental caries associated with widespread enamel demineralization on almost all palatal surfaces of the teeth (Figure 3).
In 2000 Dumic et al., reported the Xerostomia as a newly recognized finding of triple A syndrome and performed sialometry on 5 patients who presented this syndrome and all had oral dryness [11]. In our case, the results of the sialometry was 0.18ml/mn. This low salivary non stimulated flow was considered as xerostomia according to Sreebny and Valdini [12] and saliva substitutes were prescribed for the patient to ease swallowing. Xerostomia and poor oral hygiene could explain the candida infection found in the examination of the fissured tongue of our patient to whom triple mouth rinses was prescribed for 15 days including separately chlorexidine 0.12%, sodium bicarbonate 14‰ and an antifungal (Amphotericine B: fungisone 10%).
In Addison’s disease, deficient production of cortisol results in increased production of adrenocorticotropic hormone (ACTH). This could explain generalized cutaneous hyperpigmentations mostly in sun exposed skin surfaces and in the oral mucosa in our patient’s oral findings [13].
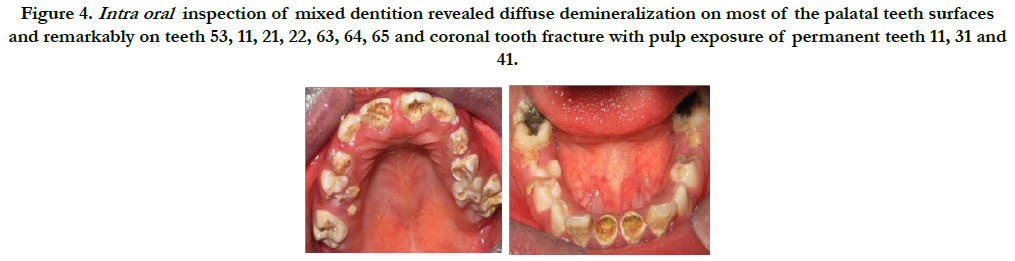
An accurate inspection of mixed dentition revealed diffuse demineralization often referred to as dental erosion on most of the palatal teeth surfaces and remarkably on teeth 53, 11, 21, 22, 63, 64, 65 (Figure 4). Generally Dental erosion is caused by dietary or gastric acid. In our case the Common causative factors for the presence of the gastric acid in the oral cavity are the consequences of the achalasia notably gastric acid reflux and repeated vomiting inducing, thereafter, oral acidity almost consistently. Gastric acid is hydrochloric acid produced by the parietal cells in the stomach and has a pH of 1–1.5 [14]. Clinical manifestation of this chemical erosion occurs when teeth are exposed to acid over several months [15]. Erosion resulting from gastric acids is often initially noted on the palatal surfaces of the maxillary incisors. In more severe cases, as in the case of our patient, the palatal surfaces of the maxillary molars will become involved and eventually the erosion pattern becomes more widespread, involving the occlusal and facial surfaces of the teeth. Furthermore, tendency to bad eating habitudes and poor oral hygiene, are aggravating factors making it worse by leading to appear readily tooth decay as shown on teeth 64, 65, 26. As a consequence of xerostomia, enamel demineralization and tooth decay, the dental inspection revealed severe hard dental tissue damages. Furthermore coronal tooth fracture with pulp exposure of permanent teeth 11, 31 and 41 and persistence of several deciduous root fragments of 54, 55, 75, and 85 were revealed as well.
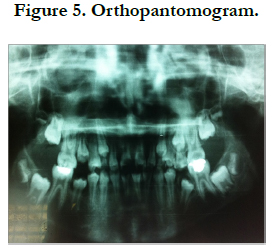
The orthopantomogram defined the severity of the damage and support the claim for extracting the deciduous teeth 53, 54, 55, 63, 64, 65 which were clinically evident and physiologically at the end of root resorption stage (Figure 5).
Figure 4. Intra oral inspection of mixed dentition revealed diffuse demineralization on most of the palatal teeth surfaces and remarkably on teeth 53, 11, 21, 22, 63, 64, 65 and coronal tooth fracture with pulp exposure of permanent teeth 11, 31 and 41.
Besides, Patients with chronic adrenal insufficiency have Immunosuppression secondary to chronic steroid usage such as hydrocortisone. They may not be able to tolerate a transient bacteremia following invasive dental procedures. This can place a patient with compromised immunity at risk for distant site infection from a dental procedure [16]. Discussion of antibiotic prophylaxis with the child’s physician was recommended. Since the patient was not allergic to penicillin 2g of amoxicillin as systematic antibiotic prophylaxis necessary commenced before and after extractions.
Moreover, all patients with adrenal insufficiency are at risk of an adrenal crisis in situations, usually of physiological stress, where the requirement for cortisol is greater than its availability in the circulation [17]. Thus, short dental care sessions in the morning were advocated just after the hydrocortisone intake and that in a de-stressing atmosphere especially during local anesthesia and extraction.
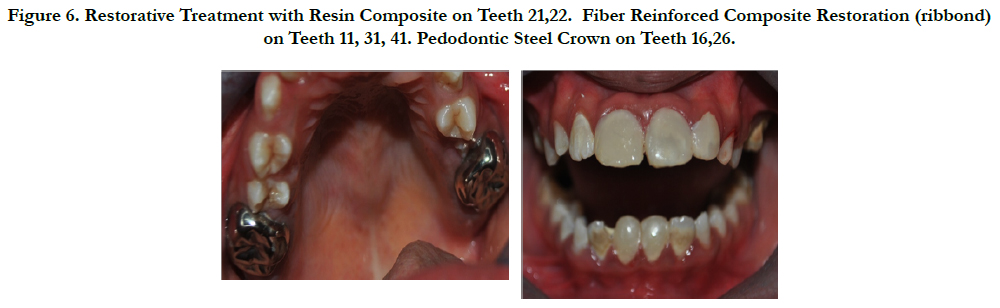
Since none of pulp treatment was contraindicated in Allgrove syndrome, our proposed conservative approach was launched with pulpectomy of the teeth 11, 31, 41 which revealed mature apex, followed by root canal filling with Gutta and then restorative treatment with resin composite and Fiber Reinforced Composite Restoration (ribbond) for teeth 21, 22 and 11, 31, 41 respectively (Figure 6). However, it is relevant to consider the role of acid conditioning by phosphoric acid prior to bonding. In fact, erosion may increase the hybrid layer thickness, which obviously hampered a proper infiltration of the adhesive resin. Fortunately, previous study have shown that Phosphoric acid relatively aggressively etches dentin, thereby dissolving thick and compact smear layers as well. The acid conditioning usually used in bonding protocols may have somehow contributed to masking or minimizing the effect of these alterations such as wear, roughness and loss of hardness [18]. Moreover, Long-term bonding to eroded dentin was clearly affected by the way the eroded dentin surface was prepared. Studies have shown that a minimally invasive cavity preparation approach with a diamond bur is highly recommended to adhesively restore erosion lesions [19].
Figure 6. Restorative Treatment with Resin Composite on Teeth 21,22. Fiber Reinforced Composite Restoration (ribbond) on Teeth 11, 31, 41. Pedodontic Steel Crown on Teeth 16,26.
Finally, prothetic treatment with pedodontic steel crown was recommended to safeguard demineralized surfaces of permanent upper molars after placing an adhesive restorations. Since amalgam is not recommended in such conditions as xerostomia and buccal acid are preponderant, its removing and placing adhesive restoration like resin composite was necessary since there was no visible dental hard loss substance on them (Figure 6).
Discussion
We report a 12-year-old young girl with Allgrove syndrome who, in addition to the original three 'A's (alacrimia, achalasia and adrenal insufficiency), presented some specific dental abnormalities. The most common oral features in Allgrove syndrome reported in the literature are xerostomia [13], malar hypoplasia, prognathism in concomitance with normal permanent teeth, fissured tongue. A combination of xerostomia, caries, periodontal disease, and premature teeth loss has been described by Li et al., in three out of six patients [2014] [20]. Dental abnormalities found in our patient such xerostomia and its sequalae, pigemented tongue and mucosa, demineralized enamel could be of great clinical importance when associated with alacrimia, achalasia or adrenal insufficiency in diagnosis of allgrove syndrome. Connection between alterations in the oral cavity and systemic health has been widely proven [21]. Alterations within the oral cavity can be the first sign of systemic or gastrointestinal disease as oral cavity is a part of the gastrointestinal system and may thus allow for an early diagnosis and treatment.
Besides, a delay of eruption was noticed in the orthopantomogram. It could be probably due to the syndrome itself or the intake medication precisely the corticosteroid therapy (Hydrocortisone) as discussed in previous studies. In fact, Hydrocortisone inhibits protein and glycoprotein synthesis, decreases amount of proliferating cells, accelerates their differentiation and thus delays formation of the root and tooth growth. According to that, dental age assessment could also be of great importance, as it shows mismatch with the chronological age so that empeted tooth eruption may be, from now on, a dental feature associated to Allgroove [22].
In addition to early diagnosis and appropriate treatment, prevention from other potential allgrove features should not be underestimated. In addition to hard tissue alteration by erosion, some previous studies have reported alterations in periodontal tissue in some cases associated with triple A syndrome. As pedodontists examine patient at infancy or early adolescence, no signs of periodontal probems may be noticed during that period, studies reported that premature permanent teeth loss may occur [23]. Allgrove patients have been stated to be more susceptible to oxidative damage, accounting for susceptibility of the patients to severe periodontal disease But since the other characteristic features of the syndrome are believed to be linked potential to progress through the years future periodontal recall appointments, seem reasonable for these patients [24].
Conclusion
The effective care of the patient with suspicious oral alterations requires interdisciplinary cooperation. Pediatric dentists can exert a dual contribution, firstly assistance in possible detection of the syndrome by facing the patient’s dental treatment needs to assessment of the relevant intraoral complaints and secondly the management of the complications associated with a poor salivary flow by Periodic fluoride therapy, professional oral care, saliva substitutes and oral hygiene instructions.
References
- Kilicli F, Acibucu F, Senel S, Dokmetas HS (2012) Allgrove syndrome. Singapore Med J 53(5): e92-94.
- Brown B, Agdere L, Muntean C, David M (2016) Alacrima as a Harbinger of Adrenal Insufficiency in a Child with Allgrove (AAA) Syndrome. Am J Case Re. 17: 703-706.
- Capataz Ledesma M, Méndez Pérez P, Rodríguez López R, Galán Gómez E (2013) Allgrove syndrome (triple A). Finding of a mutation not described in the AAAS gene. AnPediatr (Barc). 78(2): 109-112.
- Clark A, Hughes C, Metherell L (2009) ACTH insensitivity syndromes. Endocrine Rev. 19(6): 828-43.
- DavarmaneshM, Zahed M, ShahrzadS (2012) Oral manifestations of triple a (allgrOve) syndrome in siblings. Intl j dent clin. 4(4): 441.
- Krawczak M, Cooper DN (1998) The human gene mutation database. Nucleic Acids Res. 26(1): 285-287.
- Salmaggi A, Zirilli L, PantaleoniC, De Joanna G, Del Sorbo F, et al., (2008) Late-onset triple A syndrome: a risk of overlooked or delayed diagnosis and management. Horm Res. 70(6): 364-372.
- Ben Abdallah C, Lakhoua Y, Nagara M, Khiari K, Elouej S, et al., (2014) A Tunisian patient with two rare syndromes: triple a syndrome and congenital hypogonadotropic hypogonadism. Horm Res Paediatr. 82(5): 338-343.
- Khelif K, De Laet MH, Chaouachi B, Segers V, Vanderwinden JM (2003) Achalasia of the cardia in Allgrove’s (triple A) syndrome: histopathologic study of 10 cases. Am J Surg Pathol. 27(5): 667-72.
- Pedreira CC, Zacharin MR (2004) Allgrove syndrome: when a recognisable paediatric disorder occurs in adulthood. Med J Aust. 180(2): 74-5.
- Vucicevic-Boras V, JurasD, Gruden-Pokupec J, Vidovic A (2003) Oral manifestations of triple A syndrome. Eur j med res. 8(7): 318.
- Sreebny LM, Valdini A (1987) Xerostomia. A neglected symptom. Arch Intern Med. 147(7): 1333-1337.
- Meleti M, Vescovi P, Mooi WJ, van der Waal I (2008) Pigmented lesions of the oral mucosa and perioral tissues: a flow-chart for the diagnosis and some recommendations for the management. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 105(5): 606-616.
- Taji S, Seow WK (2010) A literature review of dental erosion in children. Aust Dent J. 55(4): 358–367.
- Tolia V, Vandenplas Y (2009) Systematic review: the extra-oesophageal symptoms of gastro-oesophageal reflux disease in children. Aliment Pharmacol Ther. 29(3): 258–272.
- Lockhart PB, Loven B, Brennan MT, Baddour LM, Levinson M (2007) The evidence base for the efficiency of antibiotic prophylaxis in dental practice. J Am Dent Assoc. 138(4): 458-74.
- Rushworth RL, Torpy DJ, Falhammar H (2017) Adrenal crises: perspectives and research directions. Endocrine. 55(2): 336-345.
- Wang L, Casas-Apayco LC, Hipólito AC, Dreibi VM, Giacomini MC, et al., (2014) Effect of simulated intraoral erosion and/or abrasion effects on etch-and-rinse bonding to enamel. Am j dent. 27(1): 29-34.
- Zimmerli B, De Munck J, LussiA, Lambrechts P, Van Meerbeek B (2012) Long-term bonding to eroded dentin requires superficial bur preparation. Clin Oral Investig. 16(5): 1451–1461.
- Adini G, Besagni F, Callea M, Brena M, Rossi LC, et al., (2015) Allgrove syndrome: a report of a unique case characterised by peculiar dental findings resembling those of ectodermal dysplasia. Eur J Paediatr Dent. 16(4): 324-326.
- Mantegazza C, Crippa R, Zuccotti GV (2016) Oral manifestations of gastrointestinal diseases in children. Part 1: General introduction. EJPD. 17(1): 80-2.
- Mazhuga PM , Kabak KS, ZhitnikovAIa, Kalion PT (1987) Reproduction and differentiation of cells in the tissues of growing rat teeth in response to parathyroid hormone and hydrocortisone. ArkhivAnat Gistol Embriol. 92(5): 57-62.
- Razavi Z, Taghdiri MM, Eghbalian F, Bazzazi N (2010) Premature Loss of Permanent Teeth in Allgrove (4A) Syndrome in Two Related Families. Iran J Pediatr. 101-6.
- Storr HL, Kind B, Parfitt DA, Chapple JP, Lorenz M, et al., (2009) Deficiency of ferritin heavy-chain nuclear import in triple a syndrome implies nuclear oxidative damage as the primary disease mechanism. Mol Endocrinol. 23(12): 2086-94.