Primary Cheiloplasty using the Technique of Millard
de Siqueira Bringel RJ1,2,3*, Cruz RG1, Pereira Lucena Franco JM4, Bringel DN5, Bringel GN6, Pereira Júnior FB7, Campolongo GD8, de Barros TP8, Silva Araújo MT9, Santos ES4, Pinto LP4, Reis Rodriques LM2
1 School of Dentistry, University Center Leão Sampaio, UNILEÃO, Juazeiro do Norte, Ceará, Brazil.
2 Laboratory of Study Design and Scientific Writing, ABC Medical School, Saint Andrew, Sao Paulo, Brazil.
3 Department of Oral and Maxillofacial Surgery, Hospital Agamenon Magalhãe, HOSPAM, Serra Talhada, Ceará, Brazil.
4 Department of Oral and Maxillofacial Surgery, Hospital Geral de Fortaleza, HGF, Fortaleza, Ceará, Brazil.
5 School of Medicine, Federal University of Ceara, Fortaleza, Ceará, Brazil.
6 School of Medicine, University Center Unichristus, Fortaleza, Ceará, Brazil.
7 Department of Health of the State University of Feira of Santana, Feira de Santana, Bahia, Brazil.
8 Department of Oral and Maxillofacial Surgery, Faculdade FACIG, University of São Paulo, Guarulhos, Brazil.
9 School of Medicine, Federal University of Cariri, Barbalha, Ceará, Brazil.
*Corresponding Author
Romildo José de Siqueira Bringel D.D.S, M.Sc.,
Professor, University Center Leão Sampaio,
Vital Lisboa Santos, 370 Ap. 1601, Jardim Gonzaga,
Juazeiro do Norte, Ceará, Zip Code: 63046-610, Brazil.
Tel/Fax: +55 88 99965-5883
E-mail: romildobringel@hotmail.com
Received: May 28, 2017; Accepted: June 22, 2017; Published: June 26, 2017
Citation: de Siqueira Bringel RJ, Cruz RG, Pereira Lucena Franco JM, Bringel DN, Bringel GN, et al., (2017) Primary Cheiloplasty using the Technique of Millard. Int J Dentistry Oral Sci. 4(6), 490-493. doi: dx.doi.org/10.19070/2377-8075-1700096
Copyright: de Siqueira Bringel RJ©2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Malformations of the craniomaxillofacial complex affect thousands of live births worldwide. The cleft lip and palate are congenital deformities that promote a series of harms to health, since the functions of stomatognathic system are compromised, potentially leading to systemic changes. The technique of Millard, although presents difficulties of implementation by some surgeons-in-training, due to the inherent fragility of the nasolabial structures, on the other hand, has excellent aesthetic results with low rates of surgical complications, in addition to maintaining the suture line in the philtral column, generating this way satisfactory cosmetic results. The main objectives to be achieved with this procedure are: restoring the functioning of the orbicular muscle of mouth (aiming the restoration of normal function of the upper lip), the re-establishment of normal anatomical structures of the lip and the correction of nasal deformity caused by the rift. Therefore, this article aims to present a clinical case of cleft lip/palate in adult, proceeded with its surgical correction by applying the technique of Millard, emphasizing the proper treatment and surgical technique.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.References
Keywords
Cleft Lip; Cleft Palate; Epidemiology.
Introduction
Malformations of the craniomaxillofacial complex affect thousands of live births worldwide. Birth defects like cleft lip and palate are considered an important category among the malformations, since orofacial functions like sucking, chewing, swallowing, breathing, phonation and diction, which are of paramount importance to the stomatognathic system, are compromised [1, 2].
In the last decades, the cleft lip/palate has been shown to be increasingly present throughout the world. The prevalence of this abnormality varies mainly according to geographic region, race, ethnicity, socioeconomic condition and maternal habits during pregnancy. The global estimate is 1/600-700 live births has lip and palate clefts [3-5].
Between the 8th and 32nd week of gestation, a sequence of changes in the development and/or ripeness of the embryonic processes occurs, highlighting the lack of fusion of the nasal processes with the maxillary processes, and these with each other, resulting in congenital deformities affecting the middle third of the face [5, 6]. The involvement of environmental and genetic factors and teratogens during the period of human embryonic development gives the cleft lip/palate a multifactorial character and of high complexity [7].
Due to the varied presentation of lip and palate fissures, Spina et al., 1972, ranked the malformations, taking as a point of reference the incisive foramen, into four groups (being the ranking most used in Brazil). In this way, the cracks are divided into: preincisive foramen fissure – which can be unilateral (right or left) or bilateral; trans-incisive foramen fissure–unilateral (right or left) or bilateral; post-incisive foramen fissure and rare fissures [4, 8-10].
Many surgeons have contributed to the evolution of the methods of cleft lip repair, however, the technique introduced by Ralph Millard in 1955 is the most accepted until the moment, since this surgical technique aims to restore the aesthetics and function with minimal trauma and maximum conservation of the labial structures [4, 8].
Aiming the growth and development of the craniomaxillofacial complex, as well as the perfect execution of the tasks of the stomatognathic system (phonation, swallowing, irruption of the dental elements), it is necessary multidisciplinary approach, seeking early treatment and better resolution of the case, which will last until adulthood [3, 11-14].
Therefore, this article aims to present a clinical case of cleft lip/palate in adult, proceeded with its surgical correction by applying the technique of Millard, emphasizing the proper treatment and surgical technique.
Case Report
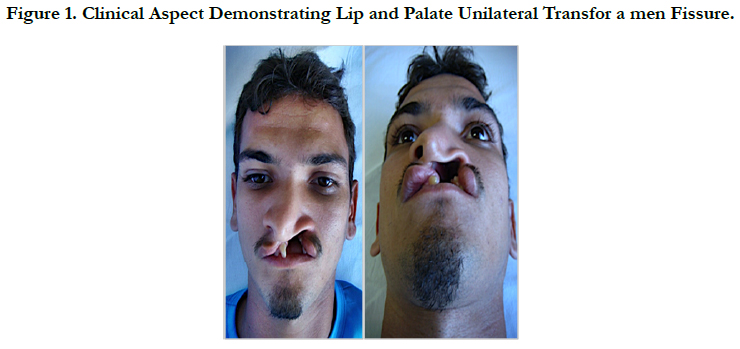
Patient A.C.S., feoderm, 28 years old, male, attended the service of Oral and Maxillofacial Surgery and Traumatology of the Hospital and Maternity São Vicente de Paula (HMSVP) in Barbalha- CE, Brazil, reporting halitosis, foul odor, ear infection, dysphagia, dyspnea and low self-esteem, showing good general state of health. At the clinical examination, it was observed a unilateral transforamen lip/palate fissure with nasal involvement, displacement and enlargement of the left nasal wing, increased cross-section and deviation of the anterior segment of the nasal septum to the right (Figure 1).
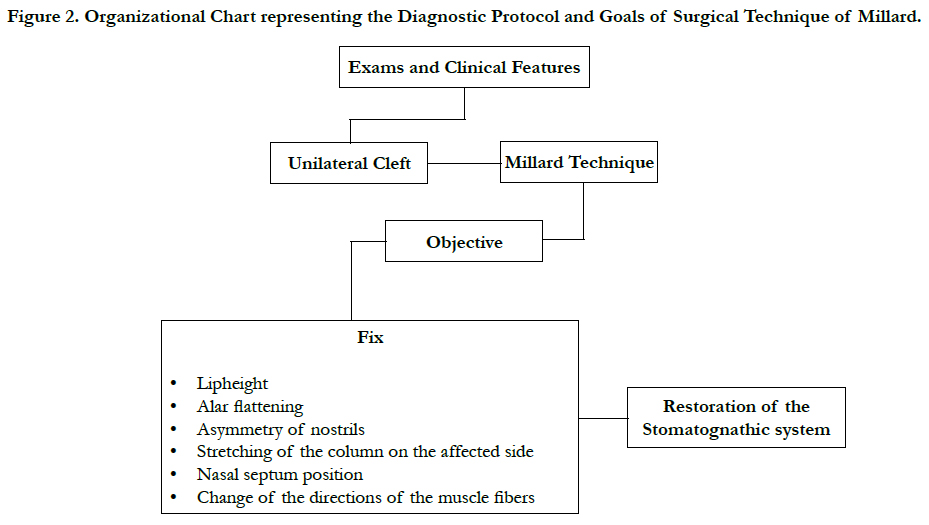
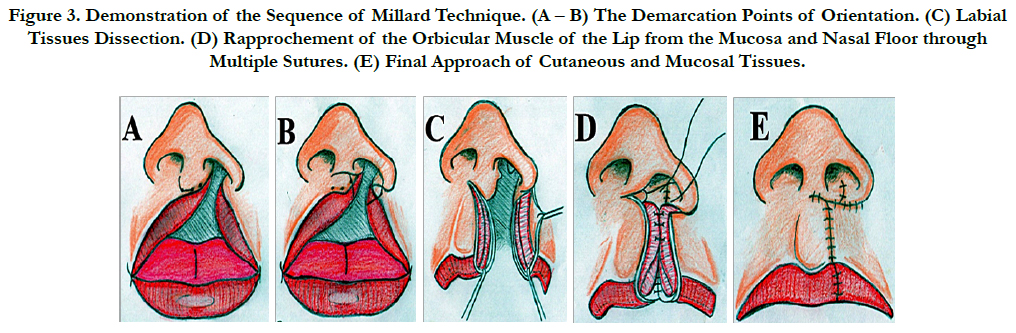
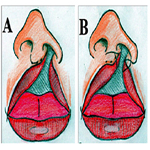
Through the clinical findings, it was proposed the implementation of cheiloplasty for surgical correction of unilateral lip cleft under general anesthesia and endotracheal intubation, with the use of the technique of Millard, adopting the protocol shown in Figure 2, involving the demarcation of points that guided the incisions, with posterior rotation of the medial flap and traction of the lateral flap. Initially, the orientation points were painted to guide the surgical incisions, it was visualized the real importance of the hypoplastic tissue removal and the rapprochement between the cutaneous- mucosa line and the red part of the lip (Figure 3 – A, B). Then, the incisions of the tissues were made, followed by careful dissection of the cutaneous, subcutaneous, muscle, and mucosa, releasing the orbicular muscle of the lips of their abnormal insertions of the anterior nasal spine and lateral alar base (Figure 3 – C). Then, the reconstruction of complex cutaneous-mucosa line was made, by approaching the orbicular muscle of the lip through multiple interrupted sutures, approaching also the mucosal flaps, and nasal floor (Figure 3 – D). Following with the advance of the lateral flap and rotation of the medial segment down, creating a scar line that reminds the crest of the lateral filter on the opposite side (Figure 3 – D).
Figure 2. Organizational Chart representing the Diagnostic Protocol and Goals of Surgical Technique of Millard.
Figure 3. Demonstration of the Sequence of Millard Technique. (A – B) The Demarcation Points of Orientation. (C) Labial Tissues Dissection. (D) Rapprochement of the Orbicular Muscle of the Lip from the Mucosa and Nasal Floor through Multiple Sutures. (E) Final Approach of Cutaneous and Mucosal Tissues.
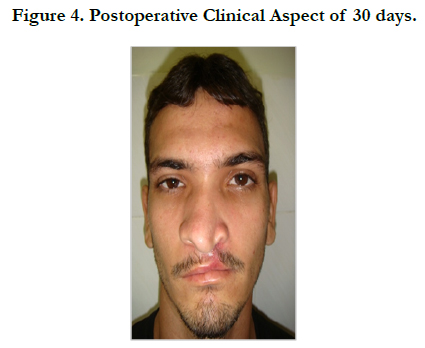
In postoperative follow-up of 2 months, the patient is with good aesthetic and functional rehabilitation, expressing intense satisfaction with the results obtained (Figure 4). Waits second surgical time for reconstruction of the palate and alveolar grafting with posterior prosthetic rehabilitation.
Discussion
Facial malformations, among them the lip and palate fissures, constitute a major scientific challenge, concerning the exact causal determination, because it is known the multifactorial influence that occurs in these defects, such as: conditions attributed to genetics, the environment and unknown factors or not defined or the associations of several factors [15].
There is a fondness of the lip and palate cracks for the male, with a higher incidence in Asian, being the trans-incisive foramen fissure on the left side sorted by SPINA et al., 1972 the most prevalent in literature [1, 16, 17], according to the type of the crack of the case presented in this article.
Surgical procedures of cleft lip and palate are diverse, since the cracks vary in: width, extent, amount of hard and soft tissue, extension of the palate. The main objective of the initial surgery is the closure of the soft tissues, and the authors of this case report are in accordance with the author in question [15-18].
The technique of Millard, although presents difficulties of implementation by some surgeons in training due to inherent fragility of nasolabial structures was chosen, for presenting excellent aesthetic results with low rates of surgical complications, in addition to maintaining the suture line in the phyltral column, generating this way satisfactory cosmetic results, being diffused worldwide [18, 19].
Among patients with craniofacial defects, cleft lip and lip/palate, simple or complex, associated with syndromes or not, have in their lives and those of their families the social conviviality harmed as a result of this change. For this reason, it is of utmost importance to provide these patients adequate guidelines about diagnosis and treatment, in order to improve their social skills and self-esteem, as well as to keep them safe from the procedures of health professionals [17, 20].
Conclusion
It can be concluded from this study that:
Millard's technique shows up as a good option among the available therapeutic arsenal, as it provides good cosmetic and functional results to patients with these lesions, as well as minimizes the psychological consequences inherent in these conditions, returning, to the patient, an improvement of self-esteem and social conviviality.
The making of preoperative and postoperative planning by the team is a condition that determines the success of the surgery and recovery. And, added to this, it becomes indispensable criteria for the rehabilitation of the patient the work of a multidisciplinary team, aiming at the conquest of biopsychosocial harmony.
References
- Rebouças PD, Moreira MM, Chagas MLB, Filho JFC (2014) Prevalence of cleft palate in a hospital of reference in northeastern of Brazil. Rev Bras Odontol. 71(1): 39-41.
- Pita Neto IC, Franco JMPL, Bringel RJS, et al., (2015) Transnasal Removal of Ectopic Supernumerary Tooth from Cleft Patient. iMed Pub J. 8: 197- 202.
- Kuhn VD, Miranda C, Dalpian DM, Moraes CMB, Backes DS, et al., (2012) Cleft Lip and Palate: Literature Review. DisciplinarumScientia. 13: 237-245.
- Ribeirov EM, Moreira ASCG (2005) Update about the multidisciplinary treatment Of cleft lip and palate. Revista Brasileira em Promoção da Saúde. 18: 31-40.
- Bringel RJS, Pita Neto IC, Franco JMPL, Araujo JLD, et al., (2015) Cleft Lip/Palate Reconstruction Using Techniques from Abbé and Von Langenbeck. iMed Pub J. 8: 198-204.
- Farronato G, Kairyte L, Giannini L, Galbiati G, Maspero C (2014) How various surgical protocols of the unilateral cleft lip and palate influence the facial growth and possible orthodontic problems? Which is the best timing of lip, palate and alveolus repair? Literature Review. Stomatologija. 16(2): 53-60.
- Cvjetkovic N, Maili L, Weymouth KS, Letra A, Yuan Q, et al., (2015) Regulatory variant in FZD6 gene contributes to nonsyndromic cleft lip and palate in an African-American family. Mol Genet Genomic Med. 3(5): 440–51.
- Spina V, Psillakis JM, Lapa FS (1972) Epidemiological data of patients with cleft lip and palate from a specialized institution in Londrina, State of Paraná. Rev Hosp Clin Fac Med São Paulo. 27(1): 50-56.
- Baroneza JE, Faria MJSS, Kuasne H, Carneiro JLVC, Oliveira JC (2005) Epidemiologic data of cleft lip and palate bearers from a specialized institution of Londrina, Parana State. Acta Sci Health Sci. 27(1): 31-35.
- Alonso N, Tanikawa DYS, Lima-Junior JE, Ferreira MC (2010) Comparative and evolutive of attendance protocols of patients with clef lip and palate. Rev Bras Cir. Plást. 25(1): 434-8.
- Kim DW, Chung SW, Jung HD, Jung YS (2015) Prenatal ultrasonographic diagnosis of cleft lip with or without cleft palate; pitfalls and considerations. Maxillofac Plast Reconstr Surg. 37(1): 1-5.
- Rossell-Perry P (2015) Flap Necrosis after Palatoplasty in Patients with Cleft Palate. BioMed Res Intl. 2015: 1-14.
- Raposo-do-Amaral CE, Kuczynski E, Alonso N (2011) Quality of life among children with cleft lips and palates: a critical review of measurement instruments. Rev Bras Cir. Plást. 26(4): 639-44.
- Furr MC, Larkin E, Blakeley R, Albert TW, Tsugawa L, et al., (2011) Extending Multidisciplinary Management of Cleft Palate to the Developing World. J Oral Maxillofac Surg. 69(1): 237-41.
- Figueiredo MC, Pinto NF, Fabricio FK, Boaz CMS, Faustino-Silva DD (2010) Patients with cleft lip and palate – clinical cases follow up. ConScientiae Saúde. 9(2): 300-308.
- Macháčová E, Bánsky R, Špaleková M, Guzanin Š, Sabovčík R, et al., (2016) Incidence of orofacial clefts in the Slovak Republic. Cent Eur J Publ Health. 14(3): 122-125.
- Cymrot M, Sales FCD, Teixeira FAA (2010) Prevalence of kinds of cleft lip and palate at Pediatric Hospital in Northeast of Brazil. Rev Bras Cir Plást. 25(4): 648-51.
- Mccomb HK, Coghlan BA (1996) Primary Repair of the Unilateral Cleft Lip Nose: Completion of a Longitudinal Study. Cleft Palate Craniofac J. 33(1): 23-30.
- Urmenyi GL, Filho JAF, Fernandez EC, Hupsel JM (2006) Primary approach to the unilateral cleft lip nose. Rev Soc Bras Cir Plást. 21(2): 67-72.
- Ajmal S, Khan MA, Khan AT, Yousaf K, Shadman M, et al., (2010) Evaluating anatomical subunit approximation technique for unilateral cleft lip repair. J Postgrad Med. 24(1): 68-72.