A Hybrid Peripheral Giant Cell Granuloma-Peripheral Ossifying Fibroma Lesion Presenting as a Solitary Gingival Enlargement
Ramesh R1*, Sadasivan A2, Pradeesh S3
1 Associate Professor, Department of Periodontics, Government Dental College, Alappuzha, Kerala, India.
2 Professor, Department of Periodontics, Sree Mookambika Institute of Dental Sciences, Kulasekharam, Tamilnadu, India.
3 Reader, Department of Oral Pathology, Sree Mookambika Institute of Dental Sciences, Kulasekharam, Tamilnadu, India.
*Corresponding Author
Dr. Roshni Ramesh MDS,
“DIYA”, KMLRA-131, Mosque Lane, Kumarapuram,
Trivandrum-695011, Kerala, India.
Tel: 9847230052
E-mail: roshni_arun@hotmail.com
Received: March 08, 2017; Accepted: May 26, 2017; Published: May 29, 2017
Citation: Ramesh R, Sadasivan A, Pradeesh S (2017) A Hybrid Peripheral Giant Cell Granuloma-Peripheral Ossifying Fibroma Lesion Presenting as a Solitary Gingival Enlargement. Int J Dentistry Oral Sci. 4(5), 487-489. doi: dx.doi.org/10.19070/2377-8075-1700095
Copyright: Ramesh R©2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Clinical and radiographic presentations of gingival enlargements often overlap. Definitive diagnosis is made after histological evaluation of excised tissues. Sometimes this is also confusing because it may show features of different clinical entities producing a diagnostic dilemma. Hybrid lesions are lesions which present features from different pathologies.
We present a case of hybrid lesion which shows features of peripheral giant cell granuloma (PGCG) and Peripheral ossifying fibroma (POsF) presenting as solitary gingival enlargement involving the maxilla in a 57 year old female patient. The clinical, radiographic and histological features are described in detail.
The purpose of this paper is to highlight the importance of thorough evaluation of hybrid lesion to get a proper diagnosis, understand their biologic behaviour and plan treatment to minimise tissue destruction and prevent recurrence. This case also points to the need to reconsider our diagnostic criteria of various enlargements and incorporate hybrid lesions as distinct clinical entity.
2.Introduction
3.Case Presentation
4.Discussion
5.Conclusion
6.References
Keywords
Hybrid Lesion; Peripheral Giant Cell Granuloma; Peripheral Ossifying Fibroma; Case Report.
Introduction
Solitary gingival enlargements are commonly seen in adult patients and are usually seen as a reaction to local irritation or chronic trauma. Among them, Peripheral ossifying fibroma (POsF) and peripheral giant cell granuloma (PGCG) are site specific lesions which are seen as lesions of the gingiva or alveolar ridge. They often present as painless, lobular, and ulcerated masses that are clinically indistinguishable from one another [1, 2]. The diagnosis is usually made based on which predominant morphologic feature is present in any specific case. However, very few reports are available of lesions showing histological features of both PGCG and POsF, distinctly, within the same lesion [3, 4].
This case reports the clinical, histopathological and surgical management of a case of PGCG which shows a distinct region of bony trabeculae and calcifications within the stroma, which could be diagnosed as a case of hybrid PGCG-POsf, as reported by Ogbureke et al., [5].
Case Presentation
A 57-year-old female patient was referred to our clinic with a complaint of a swelling in the maxillary right anterior region which was present for 4 months. She had undergone extraction of the maxillary right lateral incisor as she had a small swelling, mild pain, mobility of upper left lateral incisor about 5 months back. However after the extraction, there was an increase in size of the swelling. The patient was diabetic since 7 years, which was under control with medication.
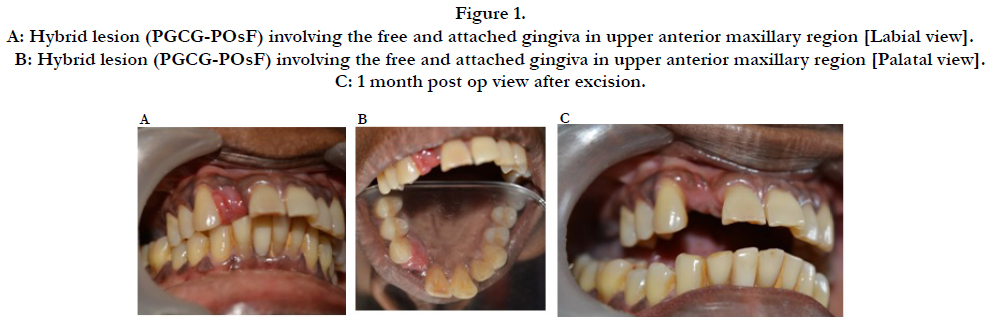
On intra-oral examination, a 10 X 12 X 8 mm sessile lobular soft tissue mass was seen which seemed to proliferate from the extraction site of 12. The mucosal covering of the lesion appeared reddish with areas of ulceration [Figure 1A & 1B].
Figure 1. A: Hybrid lesion (PGCG-POsF) involving the free and attached gingiva in upper anterior maxillary region [Labial view]. B: Hybrid lesion (PGCG-POsF) involving the free and attached gingiva in upper anterior maxillary region [Palatal view]. C: 1 month post op view after excision.
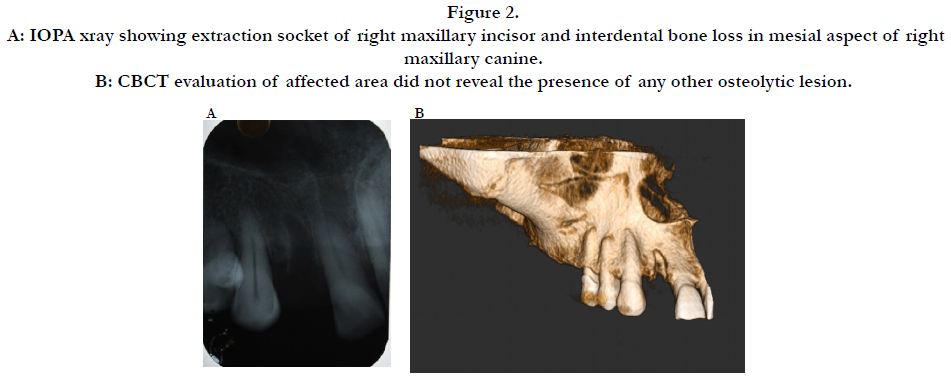
An Intra-oral peri apical radiograph of site revealed superficial a radiolucency of interdental bone in the mesial aspect of maxillary right canine. [Figure 2 A]. A CBCT section revealed [Figure 2B] unmineralised extraction socket seen in 12 region. No evidence of any other osteolytic lesion in the anterior maxillary region was reported.
The clinical and radiographic findings indicated a benign lesion, and the following differential diagnosis were considered: pyogenic granuloma, POsF, peripheral odontogenic fibroma and PGCG.
A complete blood examination showed results to be within normal limits. After initial phase 1 periodontal therapy, a wide excision of the lesion was done [Figure 1C].
Figure 2. A: IOPA xray showing extraction socket of right maxillary incisor and interdental bone loss in mesial aspect of right maxillary canine. B: CBCT evaluation of affected area did not reveal the presence of any other osteolytic lesion.
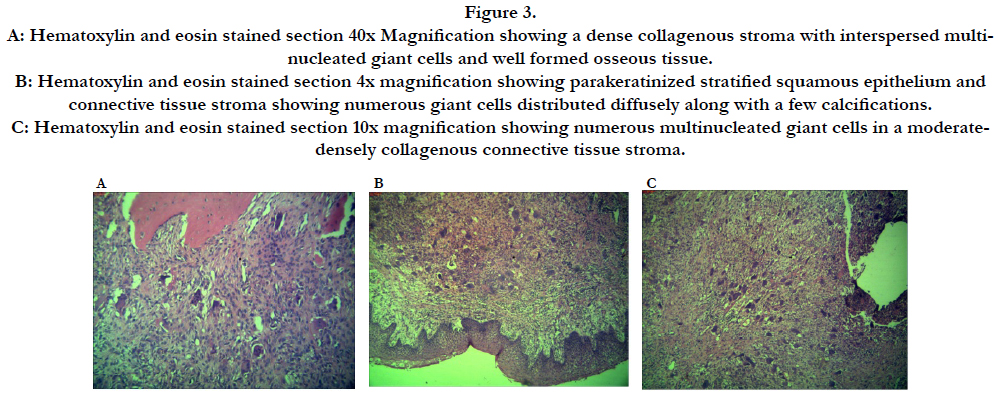
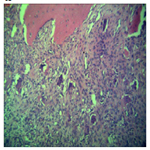
Microscopic examination of the hematoxylin and eosin stained sections of the specimen revealed parakeratinized stratified squamous epithelium which is mildly hyperplastic, proliferating in the form of long rete ridges overlying a moderate to densely collagenous connective tissue stroma. The underlying connective tissue presented plump fibroblasts. Diffuse foreign body type giant cells were seen throughout the stroma. A zone of dense fibrous connective tissue separates the area of giant cell proliferation from mucosal surface. Chronic inflammatory cell infiltrate were also seen, consisting mainly of lymphocytes and macrophages. Slightly deeper areas show distinct bony trabeculae and calcifications within the stroma [Figure 3 A, B & C].
Figure 3. A: Hematoxylin and eosin stained section 40x Magnification showing a dense collagenous stroma with interspersed multinucleated giant cells and well formed osseous tissue. B: Hematoxylin and eosin stained section 4x magnification showing parakeratinized stratified squamous epithelium and connective tissue stroma showing numerous giant cells distributed diffusely along with a few calcifications. C: Hematoxylin and eosin stained section 10x magnification showing numerous multinucleated giant cells in a moderatedensely collagenous connective tissue stroma.
The histopathological examination showed features of both PGCG and POsF, without one predominating. Thus a diagnosis of a PGCG-POsF hybrid lesion was made.
Discussion
Both POsF and PGCG represent an unusual response to tissue irritation. In the present case, the probable etiological factor could be the presence of calculus. The extraction of the lateral incisor could have been the triggered the sudden proliferation of the pre-existing lesion. Both are said to originate from the interdental tissues (periosteum or periodontal membrane) [4]. The lesions are present in all age groups with increased incidence in 40-60 year old patients, with a female predilection reported [4]. The size of the lesion was 1 cm, which is in accordance with Kfir et al., who have mentioned that 94% of these lesions are less than 1.5 cm in size [6]. The location of the lesion in the anterior maxillary region was also in agreement with Ginsanti and Waldron who suggested that it generally occurs in the incisor and canine region [7].
The diagnostic dilemma is in differentiating whether it is a case of an intra bony lesion that eroded to the surface and involving the overlying gingival soft tissue or an originally soft tissue lesion that has proliferated into bone. In our case, radiographic evaluation does not reveal the presence of deeper alveolar bone involvement, thereby precluding diagnosis of central lesions of bone.
The current case does not show massive amounts of cementoid like calcifications and more of osseous components are found. It is to be noted that even case conformed as POsFs tend to not always show presence of cementum like calcifications. It has been postulated that inherently, not all POsFs have the ability to produce cementum like calcifications [5]. The present case falls in a similar category of lesion, considering similar histopathological and clinical findings.
Ogbureke et al., have reported a case of PGCG with distinct area of extensive osseous formation and stromal area, reminiscent of the characteristic of POsF. The combined classic histopathologic features of both lesions represented in similar proportions justify the diagnosis of a combined PGCG-POsF. They conclude that the biologic behaviour of the combined lesion is not anticipated to deviate significantly from that of either of the lesions in their commonly single entity presentations [5].
Both POsF and PGCG are reactive inflammatory hyperplasias, it could be that both entities represent points on a spectrum of the same reactive disease process [8]. To avoid recurrence after treatment, in addition to complete simple excision with extensive clearing of the base of the lesion, the source of irritation needs to be removed [6].
Conclusion
We report a case in which histopathological features of both PGCG and POsF are seen in similar proportions to justify a diagnosis of a “Hybrid PGCG - POsF” lesion. Whether both these lesions originated independently or whether they belong to the spectrum of a single disease entity is open to debate. A paradigm shift in our understanding and classifying various reactive lesions of the gingiva may soon be seen with more cases with similar clinical and histopathological findings being reported in literature.
References
- Cawson RA, Speight P, Binnie WH, Wright J (1998) Lucas’s Pathology of the Oral Tissues. (5th edn), WB Saunders, Philadelphia.
- Neville BW, Damm DD, Allen CM, Bouquot JE (2008) Oral and Maxillofacial Pathology. (3rd edn), WB Saunders, Philadelphia.
- Dayan D, Buchner A, Spirer S (1990) Bone formation in peripheral giant cell granuloma. J Periodontol. 61(7): 444-446.
- Katsikeris N, Kakarantza-Angelopoulou E, Angelopoulos AP (1988) Peripheral giant cell granuloma. Clinicopathologic study of 224 new cases and review of 956 reported cases. Int J Oral Maxillofac Surg. 17(2): 94-99.
- Ogbureke EI, Vigneswaran N, Seals M, Frey G, Johnson CD, et al., (2015) A peripheral giant cell granuloma with extensive osseous metaplasia or a hybrid peripheral giant cell granuloma-peripheral ossifying fibroma: a case report. J Med Case Rep. 9:14.
- Kfir Y, Buchner A, Hansen LS (1980) Reactive lesions of the gingival. A clinicopathological study of 741 cases. J Periodontol. 51(11): 655-661.
- Giansanti JS, Waldron CA (1969) Peripheral giant cell granuloma: review of 720 cases. J Oral Surg. 27(10): 787-791.
- Bouquot JE, Muller S, Nikai H (2009) Lesions of the oral cavity. Diagnostic Surgical Pathology of the Head and Neck. (2nd edn),WB Saunders, Philadelphia. 191-308.