Single Visit Endodontic in the Management of Symptomatic Irreversible Pulpitis and Pulp Necrosis with Apical Periodontitis: Report of Two Cases
Dennis*, Cut Nurliza
Department of Conservative Dentistry, Faculty of Dentistry, University of Sumatera Utara, Indonesia.
*Corresponding Author
Dennis,
Department of Conservative Dentistry Faculty of Dentistry,
University of Sumatera Utara, Indonesia.
E-mail: dennis_dionisius@yahoo.co.uk
Received: January 22, 2017; Accepted: February 07, 2017; Published: February 08, 2017
Citation: Dennis, Cut Nurliza (2017) Single Visit Endodontic in the Management of Symptomatic Irreversible Pulpitis and Pulp Necrosis with Apical Periodontitis: Report of Two Cases. Int J Dentistry Oral Sci. 4(2), 418-421. doi: dx.doi.org/10.19070/2377-8075-1700083
Copyright: Dennis© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Single visit endodontic (SVE) therapy may be defined as the conservative non surgical treatment of an endodontically involved tooth, consisting of complete chemicomechanical instrumentation and obturation of the root canal system accomplished in one visit. This case report aims to describe two cases namely mandibular first molar with symptomatic irreversible pulpitis and maxillary first molar with pulp necrosis with apical periodontitis referred to the Clinic of Department of Conservative Dentistry, Faculty of Dentistry University of Sumatera Utara treated with single visit endodontic treatment. All cases were successfully completed in one visit with direct composite onlay as final restoration. Following one-year evaluation, there was no clinical symptoms and healing of periapical tissue was observed. Under controlled circumstances including accurate diagnosis, proper case selection, and skilled treatment technique, with single visit treatment, postoperative sequelae and healing will produce a high success rate.
2.Introduction
3.Case Series
3.1 Case 1
3.2 Case 2
4.Discussion
5.Conclusion
6.References
Keywords
Single Visit Endodontics; Irreversible Pulpitis; Pulp Necrosis; Apical Periodontitis; Healing.
Introduction
Since its introduction, single visit endodontics has been a form of focus of controversy [1, 2]. Some advocate that all root canal treatments to be done in one visit while others do not consider it even in cases of vital pulp extripation [1-3]. Some studies have reported statistically insignificant difference between single and multiple visit endodontics in terms of survival, post-operative pain or flare-ups [4]. So, it depends only on the preference of the operator to adopt single or multiple visit endodontics [5].
Single-visit endodontic therapy is defined as ‘the conservative non-surgical treatment of an endodontically involved tooth consisting of complete biomechanical cleansing, shaping and obturation of the root canal system during one visit’ [6]. With the advent of new instrumentation techniques, material science and technology, it is no more an orthodox empirical procedure for obturation of root canals [7]. However, with the introduction of magnifying loupes surgical microscopes, NiTi rotary instrument systems, ultrasonic devices, newer obturation systems (injectable obturation system), it is now considered as an acceptable alternative treatment procedure for endodontic problems [8]. Although a number of clinical research studies have shown favourable results with single visit protocols, evidence-based studies do report that there is a lack of clinical evidence to support these results [9]. Thus, it is still a dilemma for the contemporary general practitioner as well as the specialist as to when and how to proceed with single visit endodontics [10, 3, 11].
This article describes two cases of irreversible pulpitis and pulp necrosis with apical periodontitis treated in one visit.
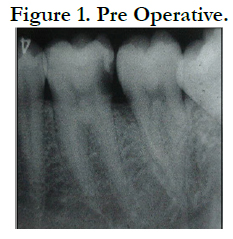
A 25-year-old female patient presented to the Dental Clinic at Department of Conservative Dentistry, University of Sumatera Utara, with the chief complaint of a toothache in her right mandible. She had spontaneous throbbing pain during her sleep and she felt discomfort on eating. Clinical examination revealed that the tooth #46 had deep caries that had reached the pulp from distal part. The tooth gave positive response to electric pulp test and was not tender to percussion and palpation. A diagnosis of symptomatic irreversible pulpitis with a normal periapical tissue and pre operative radiography was was made (Figure 1).
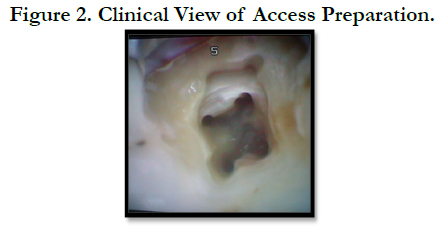
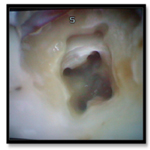
The patient’s medical history was non-contributory and an emergency pulpectomy was performed at the first visit. During examination with an operating microscope (JedMed/Kaps, St Louis, MO, USA) the anatomy of the first right mandibular molar was determined as follows: two canals in the mesial root and distal root (Figure 2). Under the microscope it was possible to insert a size #10 and #15 K-file for glidepath and working length was determined with electronic apex locator (Root ZX, J. Morita MFG. Corporation, Kyoto, Japan) (Figure 3).
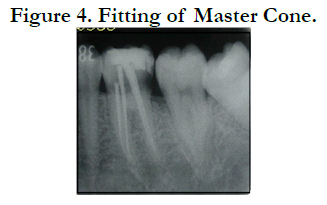
These four canals were completely instrumented and cleaned thoroughly in one visit using pathfile (Dentsply) and Mtwo rotary Niti files (VDW) until 40/0.04 for each canal. 2.5% Sodium hypochlorite and 17% EDTA were used as irrigants alternatively. Final irrigation was 3% Chlorhexidine. Fitting master cone was done and the radiography was taken (Figure 4).
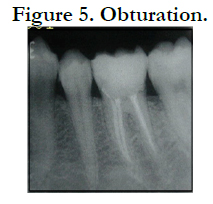
Obturation was done using combination of lateral condensation and warm gutta percha technique using System B tip (Sybron) and hot injection (Discuss Dental) (Figure 5).
Composite resin with fiber reinforced onlay restoration was made as final restoration. Twelve months later the patient was recalled for a follow-up. At the clinical examination the tooth was asymptomatic and the radiographic examination revealed normal periapical tissue (Figure 6).
A 28 year-old female patient presented to the Dental Clinic at Department of Conservative Dentistry, University of Sumatera Utara with a chief complaint of discomfort and pain while chewing with his right maxillary first molar for past few weeks. History revealed a diffuse pain and discomfort with biting on the tooth. On clinical examination pain on percussion and negative response to thermal tests were present in relation to with restoration. Preoperative radiograph showed slight periapical radiolucency (Figure 7).
During the access cavity preparation, the pulpal floor was inspected for the canal opening. Examination with an operating microscope (JedMed/Kaps, St Louis, MO, USA) showed the anatomy of the right maxillary first molar was determined as follows: two canals in the mesiobuccal root, one canal in distobuccal root and one canal in palatal root (Figure 8).
The negotiation of canals began with no. 10 and 15 ISO file. On closer inspection with 4.5 times magnification prismatic loupes the pulp chamber floor was carefully examined. The working lengths of all root canals were estimated using an electronic apex locator (Root ZX, J. Morita MFG. Corporation, Kyoto, Japan) and then confirmed radio graphically with initial files (Figure 9).
All canals were initially cleaned using smaller K-files ISO 10 and 15 as glidepath followed by ultrasonic files. 2.5% Sodium hypochlorite and 17% EDTA were used as irrigants alternatively. Final irrigation was 3% Chlorhexidine. Cleaning and Shaping were completed using rotary Mtwo instruments with crown-down technique until 40/0.04 for palatal canal and 35/0.05 for buccal canals.
The master cone was selected and the root canals dried with absorbing paper points (Figure 10). Root canals were obturated using combination of cold lateral condensation technique and compaction technique of warm guttapercha with MTA based sealer (Fillapex, Angelus Brazil). After obturation, glass ionomer cement was used to seal coronal portion (Figure 11).
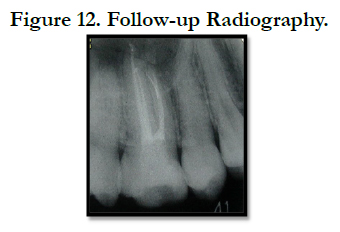
The tooth was then restored with composite resin onlay restoration with polyethylene fiber reinforced. Follow-up was done for one year. There was good prognosis with no clinical symptom and the radiograph showed complete periradicular healing (Figure 12).
Discussion
Endodontic treatment aims at the complete elimination of microbial invaders of the root canal system [1-4]. Studies have shown that instrumentation and irrigation of the root canal system substantially reduce the number of cultivable microorganisms but rarely lead to a total eradication [1-3]. Minute differences in periapical healing were observed among individuals undergoing single visit and multiple visit root canal treatment and bacterial growth at the second appointment had a significant negative impact on healing of the periapical lesion [4, 5]. In addition to this, the clinical efficacy of sodium hypochlorite irrigation in the control of root canal infection is much more than the effectiveness of interappointment calcium hydroxide dressing, in disinfecting the root canal system and treatment outcome, indicating the need to develop more efficient inter-appointment dressings [6, 7]. E. faecalis is the most resistant bacterium against calcium hydroxide while sodium hypochlorite is effective against it in both buffered and unbuffered states [8]. However, quantity of the irrigant is more important than type of the irrigant, therefore copious irrigation is recommended [9].
Intra-canal medicaments can only work efficiently if they are in direct contact with microorganisms [10]. Most of the microorganisms causing endodontic failure, resides deep in dentinal tubules or accessory canals and multiple visits allow them to proliferate resulting in poor apical healing and endodontic failure [3]. Therefore these days it is considered a better option to disinfect the canals with copious irrigation of sodium hypochlorite and sealing the canals resulting in elimination of the sources which will allow the multiplication of micro-organisms and therefore allow better periapical healing and better treatment outcome [11].
In recent years, single-appointment endodontics has gained increased acceptance [3-6]. Recent studies have shown little or no difference in the quality of treatment or success rates between single- and multiple-visit root canal treatment [5-9].
However, Nair et al., found that 14 of 16 (88%) mandibular molars that were treated in a single-visit endodontic treatment harbouredintracanal microorganisms immediately after completion of the treatment [8]. Other studies have also recommended that endodontic treatment of non-vital teeth with infected root canals should be completed in one session, without any intracanal microbicidal dressing [9]. Intraradicular microbes surviving root canal treatment are argued to be entombed by obturation of the root canal and die off as a result of inadequate nutrients [10]. ‘These microbes may no longer interfere with the periapical healing process [3]. According to Sjögrenet al., the periapical healing of some teeth occurs even when microbes are present in the canals at the time of obturation [11]. Although this may imply that the organism may survive post-treatment, it is possible that the microbes may be present in quantities and virulence that may be subcritical to sustaining the inflammation of the periapex, or that they remain in a location where they cannot communicate with the periapical tissues [10,3, 11].
Conclusion
The single-visit root canal treatment is safe in terms of endodontic flare-ups as far as results of this study are concerned. It is safer in both vital and non-vital teeth, and even teeth with periapical pathosis. A thorough understanding of the basic endodontic principles is important in considering each case on an individual basis before making a decision as to whether or not it can be completed in one visit.
The effectiveness of single-visit and multiple-visit root canal treatment is not substantially different. Therefore, the use of an inter appointment intracanal medication might be unnecessary when the operator, during a single visit, carefully debrides the canals, uses an adequate antimicrobial irrigant, and accomplishes an effective obturation of the root canal system. The incidence of post operative discomfort/pain is also similar, although patients undergoing single visit RCT might experience a higher frequency of swelling and are more likely to take analgesics. Long term success using radiographic assessment is also similar to both the groups.
References
- Kakehashi S, Stanley H, Fitzgerald R (1965) The effect of surgical exposures of dental pulps in germ free and conventional laboratory rats. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 20: 340–9.
- Moller AJ, Fabricius L, Dahlén G, Ohman AE, Heyden G (1981) Influence on periapical tissues of indigenous oral bacteria and necrotic pulp tissue in monkeys. Scand J Dent Res. 89(6): 475–84.
- Weiger R, Rosendahl R, Löst C (2000) Influence of calcium hydroxide intracanal dressings on the prognosis of teeth with endodontically induced periapical lesions. Int Endod J. 33(3): 219–26.
- Cohen S, Burns RC (2002) Pathways of thepulp. 8th (Edn), St Louis, Mosby : US.
- Sathorn C, Parashos P, Messer HH (2005) Effectiveness of single- versus multiple-visit endodontic treatment of teeth with apical periodontitis: a systematic review and meta-analysis. Int Endod J. 38(6): 347–55.
- Peters LB, Wesselink PR (2002) Periapical healing of endodontically treated teeth in one and two visits obturated in the presence or absence of detectable microorganisms. Int Endod J. 35(8): 660–7.
- Field JW, Gutmann JL, Solomon ES, Raakusin H (2004) A clinical radiographic retrospective assessment of the success rate of single-visit root canal treatment. Int Endod J. 37(1): 70– 82.
- Nair PNR, Henry S, Cano V, Vera J (2005) Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after ‘one-visit’ endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Endod. 99(2): 231–52.
- Pekrun RB (1986) The incidence of failure following single-visit endodontic therapy. J Endod. 12(2): 68–72.
- Peters LB, Wesselink PR, Moorer WR (1995) The fate and the role of bacteria left in root dentinal tubules. Int Endod J. 28(2): 95–9.
- SjögrenU, FigdorD, PersonS, SundqvistG (1997) Influence of infection at the time of the root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J. 30(5): 297–306.