Orofacial Manifestations of Robinow’s Syndrome: 5 years Follow-up Case
Jihène Z*, Anas B, Jemmali B
Faculty of Dentistry, Monastir Pediatric Dentistry Department, Hospital La Rabta, Carthage, Tunisia.
*Corresponding Author
Zaroui Jihène,
Faculty of Dentistry, Monastir Pediatric Dentistry Department,
Hospital La Rabta, Street of the Oasis, Ettaalok Residence, Block B,
Floor 3, Apart 1, Mohamed Ali, 2016, Carthage, Tunisia.
Tel: 0021622535160
Fax: 0021671570506
E-mail: dr-jihenezaroui@hotmail.fr
Received: August 26, 2017; Accepted: October 26, 2017; Published: October 31, 2017
Citation:Jihène Z, Anas B, Jemmali B. Orofacial Manifestations of Robinow’s Syndrome: 5 years Follow-up Case. Int J Dentistry Oral Sci. 2017;4(10):537-540. doi: dx.doi.org/10.19070/2377-8075-17000106
Copyright: Jihène Z©2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The Robinow’s syndrome or “foetal face” is an extremely rare genetic disorder with characteristic craniofacial, skeletal, genital and oral findings.
The main craniofacial deformities are frontal bossing, midfacial hypoplasia, hypertelorism, wide palpebral fissures and a short upturned nose. Skeletal features included short stature, mesomelic shortening limb, small hands with brachydactyly, camptodactyly and hemangioma. Genital hypoplasia is often observed. Oral findings included a triangular mouth, along upper lip philtrum, micrognathia, a shortened tongue with a devoid tongue tip, gingival hyperplasia, abnormal uvula, misaligned, crowded teeth and delayed tooth eruption. The purpose of the present case report is to describe the clinical findings and dental treatment in a 3-year-old female patient with a decline of 5years.
2.Introduction
3.Case History
4.Discussion
4.1 Capillary Hemangioma
4.2 Mental Retardation
4.3 Consanginity and Inheritance
4.4 Dental Management
4.5 Genetic Testing
5.Conclusions
6.References
Keywords
Robinow Syndrome; Oral Findings; Missing Tooth Key Messages; Oral Manifestations.
Introduction
Robinow syndrome was first described by Robinow and colleagues in 1969 [1].
It is a very rare genetic disorder with an incidence of about 1:500000 and a 1:1 male-to-female ratio [2, 3].
Both autosomal recessive and autosomal dominant inheritance have been described [4].
These patients have craniofacial, oral, musculo skeletal and genital features [5].
Intelligence is usually normal and prognosis is good when there is no congenital heart disease [2].
The aim of this article is to present a case of Robinow syndrome in a pediatric patient and to describe its craniofacial and oral abnormalities.
Case History
A 3-year-old girl, previously diagnosed with Robinow syndrome was referred to our clinic because of misaligned and missing teeth. She was born to healthy and not related parents. Her female sibling was normal.
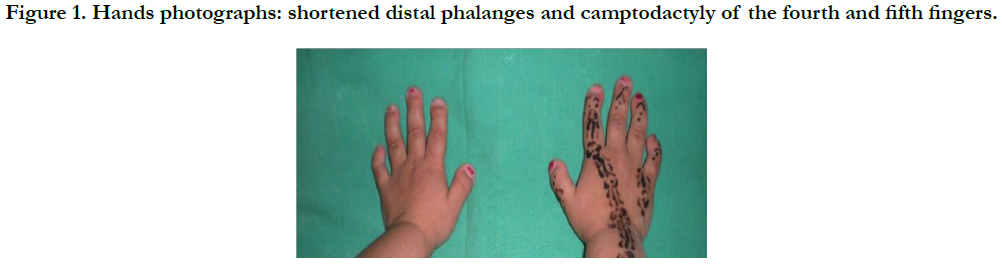
During anamnesis, the mother reported a nun eventful pregnancy. She had a mesomelic shortening limb, small hands with shortened distal phalanges and camptodactyly of the fourth and fifth fingers (Figure 1).
There was hemangioma in the thorax.
Figure 1. Hands photographs: shortened distal phalanges and camptodactyly of the fourth and fifth fingers.
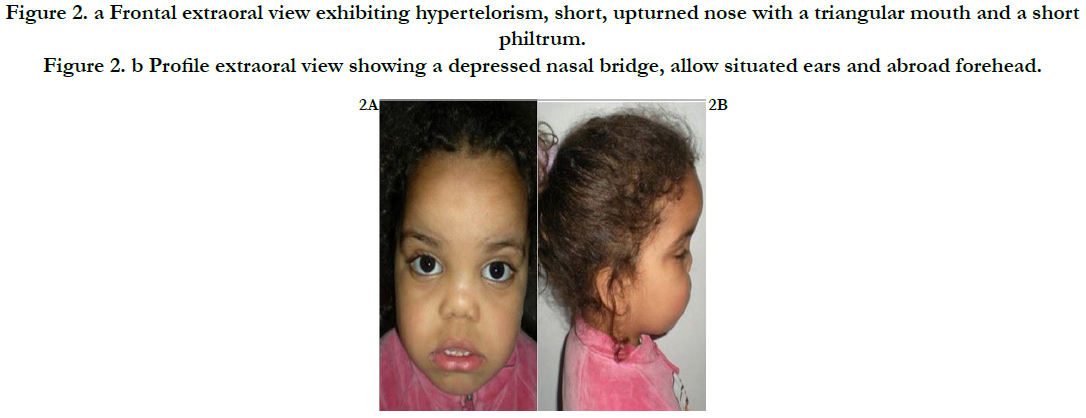
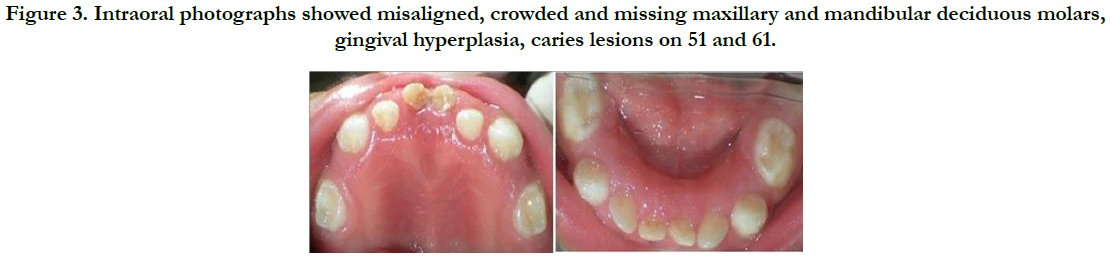
The eyes were laterally displaced so there was hypertelorism, she had also a short up turned nose with a triangular mouth and a short philtrum (Figure 2a).
Then asal bridge was depressed, ears were low situated and the forehead was broad (Figure 2b).
Figure 2. (a) Frontal extraoral view exhibiting hypertelorism, short, upturned nose with a triangular mouth and a short philtrum. (b) Profile extraoral view showing a depressed nasal bridge, allow situated ears and abroad forehead.
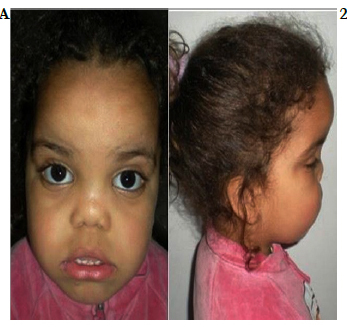
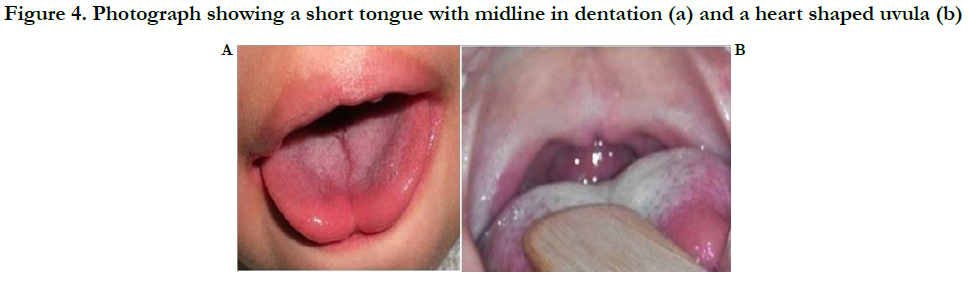
Oral examinations showed misaligned, crowded and missing maxillary and mandibular deciduous molars, gingival hyperplasia, caries lesions on 51 and 61 (Figure 3), short tongue with midline in dentation which appeared as a bifid tongue and the mobility of the tongue is missing (Figure 4a).
The uvula was abnormal: heart shaped (Figure 4b).
Figure 3. Intraoral photographs showed misaligned, crowded and missing maxillary and mandibular deciduous molars, gingival hyperplasia, caries lesions on 51 and 61.
Figure 4. Photograph showing a short tongue with midline in dentation (a) and a heart shaped uvula (b).
The Dental treatment that we proposed was pulpotomy on 51 and 61 followed by restoration with glass-ionomer (Figure 5). The patient was not cooperative during dental appointments. Dietary and oral hygiene instructions were also given to the parents. Follow-up visits were scheduled to allow the continuous monitoring of dental development.
One year follow–up of the patient revealed the eruption of 55, 65, 75 and 85 at the age of 4 years.
When the patient was more cooperative at the age of 8 years, we ask the patient for a conebeam.
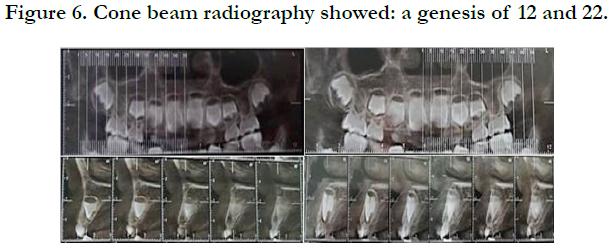
We concluded that the rear eagenesis of 12 and 22 (Figure 6).
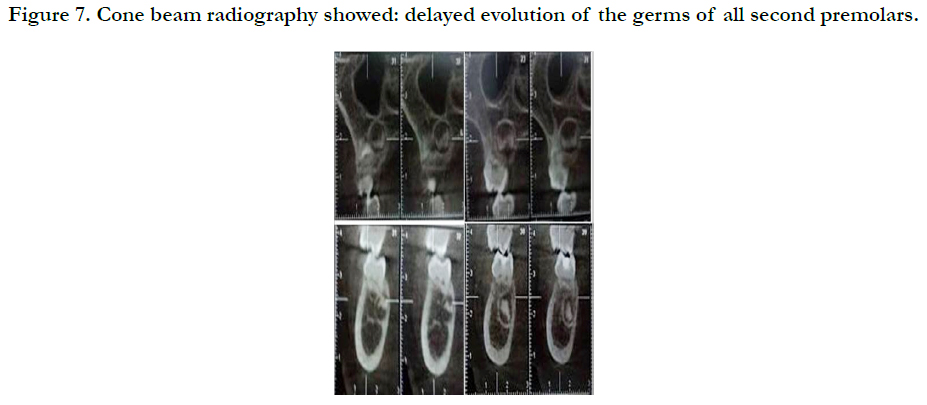
There are also a delayed evolution of the germs of all second premolars and first permanent molars (Figure 7).
41 and 31 erupted lingually while 81 and 71 were over retained.
Discussion
The Robinow syndrome (RS) was introduced by Meinhard Robinow for the first time in 1969, who described several family cases exhibiting mesomelic limb shortening, hypertelorism and hypoplastic genitalia [1]. Since then, 200 patients with this disorder have been reported around the world [3].
In 1978, Wadia et al., [5] reported a new autosomal recessive syndrome known with COVESDEM (cost over tebral segmentation defects with mesomelia). This form includes a mesomelic limb shortening, a pattern of facial characteristics, hypoplastic genitalia and cost over tebral defects. Two variants of RS were then recognized: autosomal dominant (DRS) and recessive (RRS) [4].
The mutated gene responsible for RRS has been identified as ROR2 at 9q22, a member of the receptor tyrosine kinase-like gene family that encodes an orphan membrane-bound tyrosine kinase involved in cell growth and differentiation [6-8]. Mutations in WNT5A, locus 3p 14.3 are responsible for the DRS which is characterized by more prominent oral manifestations [4].
Regarding the diagnosis, it relies heavily on the clinical picture not ably the typical foetal face appearance. Radiological examination is however necessary to confirm the presence of skeletal malformations [2].
Ocular hypertelorism, low-set ears, broad prominent forehead, mid face hypoplasia, prominent eyes, short up turned nose with depressed nasal bridge and flared nostrils are the facial features of this clinical entity [2, 4, 5]. For the oral manifestations, patients exhibit large and triangular mouth with exposed incisors and upper gums, gum hypertrophy, crowding teeth, an kyloglossia, and micrognathia [2, 4, 5, 7].
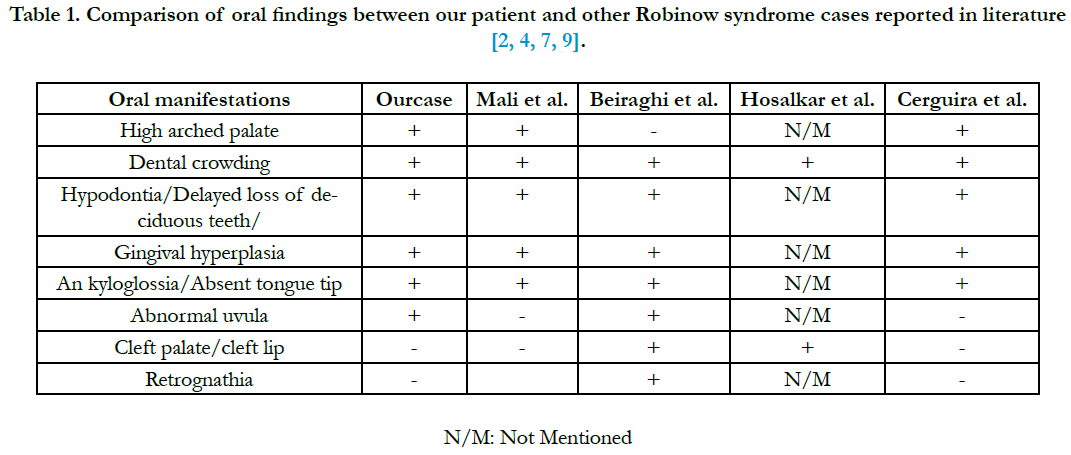
Our patient had a convex profile. Convex, straight or concave facial profiles were described in the literature. Beiraghi et al. Reported that straight and concave profiles were more common in RRS [4] (Table 1).
The present report describes a midline capillary hemangioma which has a rare occurrence in the literature.
Some degree of mental retardation may be exhibited, but in majority, the intelligence is normal [7].
Our patient was normal.
Parental age has not been found to be significant fact or in autosomal dominant form, although consanguinity seems to play an important role in the recessive form [10].
The dental treatment that should be proposed includes restorations and fluoride application for hypoplastic teeth in serious caries risk. Follow-up visits should be scheduled to ensure monitoring of dental development [7].
Parents must be advised for the possible need for orthodontic/prosthodontic treatment and orthopaedic and plastic surgery procedure for facial reconstruction in case of psychological problems caused by patient’s craniofacial anomalies [2].
The important role of genetic testing by the knowledge about the molecular basis of the disorder enabled us to make a prenatal diagnosis, genetic carrier detection and proper genetic counselling for families [6].
Prenatal diagnosis is possible by means of foetal ultrasound at 19 weeks of pregnancy [2].
Conclusion
Robinow syndrome is a very rare disease. Affected patients share characteristic facial features, with many constant oral manifestations like retained deciduous teeth, an kyloglossia, arched palate, gingival hyperplasia, dental abnormalities and delayed tooth eruption.
This case report emphasizes the importance of oral manifestations of this syndrome. These patients need specific dental care so dentists and pediatric dentists should be well informed about oral findings of RS syndrome.
References
- Robinow M, Silverman FN, Smith HD. A newly recognized dwarfing syndrome. Am J Dis Child. 1969 Jun;117:645-651. PubMed PMID: 5771504.
- Mali S, Bansal N, Dhokar A, Yaday M. Orofacial Manifestations of Autosomal Recessive Robinow's Syndrome: A Rare CaseReport. J Clin Diagn Res. 2016 Mar;10(3): ZD09-10. PubMed PMID: 27135013.
- Mishra S, Agarwalla SK, Pradhan S. Robinow Syndrome: A Rare Diagnosis. J Clin Diagn Res. 2015 Dec;9(12): SD04-SD05. PubMed Central PMCID: PMC4717695.
- Beiraghi S, Leon-Salazar V, Larson BE, John MT, Cunningham ML, Petry k, et al. Craniofacial and intraoral phenotype of Robinow syndrome forms. Clin Genet. 2011 Jul;80(1):15-24. PubMed PMID: 21496006.
- Soman C, Lingappa A. Robinow Syndrome: A Rare Case Report and Review of Literature. Int J Clin Pediatr Dent. 2015 Aug;8(2):149-152. PubMed PMID: 26379386.
- Tamhankar PM, Vasudevan L, Kondurkar S, Yashaswini K, Agarwalla SK, Nair M, et al. Identification of novel ROR2 genemutations in Indian children with Robinow syndrome. J Clin Res Pediatr Endocrinol. 2014;6:79-83.
- Cerqueira DF, deSouza IP. Orofacial manifestations of Robinow's syndrome:a case report in a pediatric patient. 2008 Mar;105(3):353-357. PubMed 18061493.
- Mazzeu JF, Pardono E, Vianna-Morgante AM, Richieri-Costa A, Ae Kim C, Brunoni D, et al. Clinical characterization of autosomal dominant and recessive variants of Robinow syndrome. Am J Med Genet A. 2007 Feb 15;143(4):320-325. PubMed PMID: 17256787.
- Hosalkar HS, Gerardi J, Shaw BA. Robinow syndrome. JPGM. 2002;48(1):50-51.
- Patton MA, Afzal AR. Robinow syndrome. J Med Genet. 2002 May;39(5):305-310. PubMed PMID: 12011143.