Effectiveness of Pre-and Post-Archwire Insertion Acetaminophen Vs. Non-Pharmacologic Management of Pain During Orthodontic Tooth Movement
Nicole D. Teifer1 , Larry J. Oesterle2*, W. Craig Shellhart3, Sheldon M. Newman4
1 Private Practice, Canton, MI,USA.
2 Professor, Director of Research, Department of Orthodontics, University of Colorado, Aurora, CO, USA.
3 Professor and Interim Chair, Program Director, Department of Orthodontics, University of Colorado Denver, Aurora, CO, USA.
4 Associate Professor, Department of Restorative Dentistry and Department of Orthodontics, University of Colorado Denver, Aurora, CO, USA.
*Corresponding Author
Larry J. Oesterle DDS, MS,
Professor and Director of Research,
Department of Orthodontics, University of Colorado,
Mail Stop F849,13065 E. 17th Avenue,Aurora, CO 80045
Business Phone: (303) 724-6992; Fax: (303) 724-6999
Email: larry.oesterle@ucdenver.edu
Article Type: Research Article
Received: August 30, 2014;Accepted: October 01, 2014;Published: October 02, 2014
Citation: Nicole D. Teifer, Larry J. Oesterle, W. Craig Shellhart, Sheldon M. Newman (2014) Effectiveness of pre- and post-archwire insertion acetaminophen vs. non-pharmacologic management of pain during orthodontic tooth movement. Int J Dentistry Oral Sci. 2(1), 1-5.
doi: dx.doi.org/10.19070/2377-8075-140001
Copyright: Murr L E © 2014. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Some patients undergoing orthodontic treatment perceive discomfort at levels that may negatively impact their feelings about their treatment and decrease their compliance. The purpose of this investigation was to study the effectiveness of either pre- or post-archwire insertion acetaminophen versus a placebo or telephone call in controlling discomfort.
Materials/Methods: A total of 120 patients, aged 12 to 18 years, undergoing fixed comprehensive orthodontic treatment were randomly
assigned to one of six experimental groups:
(1) 600 mg acetaminophen pre-treatment, 600 mg acetaminophen post-treatment;
(2) lactose placebo pre-treatment, 600 mg acetaminophen post-treatment;
(3) 600 mg acetaminophen pre-treatment, lactose placebo post-treatment;
(4) lactose placebo pre-treatment and post-treatment;
(5) courtesy phone call pre-treatment, courtesy phone call posttreatment;
(6) no courtesy phone call pre-treatment or post-treatment.
Medication group subjects were instructed to take the oral medications at prescribed time intervals before and after initial archwire insertion. The patient’s level of discomfort was assessed using a 100mm visual analogue scale (VAS) approximately 1 hour prior to initial archwire placement and at 3, 7, 19, 24, 31, and 48 hours after archwire placement.
Results: The peak level of mild to moderate discomfort occurred 19 hours after archwire placement and the differences in VAS scores between the six groups and gender were not statistically significant.
Conclusions: All of the interventions were equally effective in controlling the pain following initial orthodontic appliance placement,indicating a relatively low level of pain.
2.Introduction
3.Material and Methods
4.Results
5.Discussion
6.Conclusions
7.References
Keywords
Orthodontic pain, Pre-treatment and post-treatment Acetaminophen, Courtesy Phone Calls, Pharmacologic pain management, Non-pharmacologic pain management
Introduction
Orthodontic treatment results in high patient and parent satisfaction, but a discouraging factor for many patients is the post-adjustment discomfort.[1] Oliver et al[1] found that patients ranked pain as the worst aspect of orthodontic treatment and the foremost reason in wanting to discontinue care. Jones and Chan[2] even found that the prevalence, intensity, and duration of pain following archwire insertion were greater than post-extraction pain. Significant variability was found in the perception of pain associated with orthodontic treatment, varying with gender, age, types of forces applied, and personality type.[3] Berqius et al[3] in their review reported that pain was significantly higher for girls than boys and the highest frequency of pain was in a group of 13-16 year olds, but the pain intensity did not differ between age groups. Since pain is a routine part of orthodontic treatment, orthodontists should provide the patient information in advance concerning any discomfort that may occur.[4] Poor management of pain perception may lead to avoidance of treatment, missed appointments or poor compliance. Therefore, it is critical that orthodontists give appropriate instructions on how to control pain to obtain good treatment cooperation.[4]
According to Doll et al[4] treatment cooperation and attitude to treatment after 6 months correlated with the amount of pain that the patient experienced. Their finding was confirmed by Sergl et al[5] who found that the patient’s acceptance of their orthodontic appliance and treatment was affected by the amount of initial pain that the patient experienced. In other words, the success of orthodontic treatment may be significantly influenced by the pain management instructions provided to the patient and the ensuing pain that the patient experienced[4].
Pain management may include pharmacologic or non-pharmacologic methods.[6] Pharmacologic methods decrease pain, but the most appropriate analgesic to administer to our orthodontic patients must be determined.[4] Salmassian et al[7] found that ibuprofen, acetaminophen and a placebo were equally effective in controlling post-appliance placement pain. Kehoe et al[8] found that when comparing acetaminophen and ibuprofen, that acetaminophen was more suitable and recommended acetaminophen should be taken for the relief of minor discomfort associated with orthodontic treatment. Walker and Buring’s[9] animal study, however, found decreased tooth movement following ibuprofen administration and recommended future studies employ acetaminophen to avoid undesirable effect on tooth movement. Kehoe et al[8] found that acetaminophen was an effective analgesic for the relief of minor discomfort associated with orthodontic treatment. Simmons and Brandt[10] suggested that analgesics should be taken prior to the procedure and for a minimum of 24 hours following the procedure.
An important consideration is the timing of the pain experienced by the patient and the procedures associated with the pain. Bernhardt et al[11] found that the administration of ibuprofen prior to separator placement significantly decreased reported pain 2 hours after placement and at bedtime. On the second day following separator placement, they reported that patients that had taken pre-treatment (60 min prior to insertion) and post-treatment ibuprofen doses had lower pain scores than the groups that did not. They suggested that the best method for treatment of acute pain was to stop immediate peripheral sensitization and prevent subsequent central sensitization. Preemptive administration of pain medications[11] is one way to stop the immediate peripheral sensitization that results in pain perception. Salmassian et al[7] found that routine initial archwire insertion resulted in mild to moderate pain that began at 3 hours and peaked at 19 hours. An important consideration in determining whether pre-treatment or post-treatment administration of acetaminophen is preferred is to determine the placebo effect of taking a medication.
Although pharmacologic means are traditionally used to control orthodontic pain, non-pharmacologic methods may also be effective. Hathaway[6] found decreased pain perception with psychosocial patient management. Miranda et al[12] found that patients with greater anxiety responses felt more peak pain than patients with lower anxiety responses. Hathaway[6] also found that a patient’s perception of their post-treatment pain experience was a crucial component of their overall level of satisfaction with care. Patients who consider themselves well informed were more likely to have positive outcomes and increased satisfaction with their care.[6] Similar to Hathaway’s[6] findings, Bartlett et al[13] found that when a patient received a pre-appointment telephone call from their health care provider their anxiety decreased and, more importantly, the pain that they reported also decreased. One simple way to reassure patients about their treatment was through pre-treatment and post-treatment follow-up courtesy calls. Few studies have studied whether phone calls pre-treatment and posttreatment decrease a patient’s pain perception. Provider phone calls allow patients to ask any questions and to be reassured. An important question is whether phone calls decrease their perception of pain and lessen their dependence upon analgesics.
The purpose of this study was to compare the effectiveness of pre-treatment or post-treatment acetaminophen or telephone calls following initial archwire placement.
Materials and Methods
This was a partially blinded, randomized clinical trial.
One hundred twenty consecutive patients from the University of Colorado, Department of Orthodontics Clinic were randomly assigned into six groups of 20 subjects each. All patients met the following inclusion criteria:
(1) scheduled to begin comprehensive orthodontic treatment (banding/bonding of at least 10 teeth in one arch and archwire insertion in at least one arch);
(2) extractions, if required, performed at least two weeks prior to appliance placement and archwire insertion;
(3) healthy with no significant medical findings;
(4) no prophylactic antibiotic coverage required;
(5) currently not taking any antibiotics or analgesics;
(6) no contra-indications to the use of acetaminophen;
(7) no lactose intolerance;
(8) minimum age of 12 years and minimum weight requirement of 88 lbs (as required by the FDA for the use of OTC pediatric dosage label guidelines); and
(9) a maximum age of 18 years to exclude the adult population.
Colorado Multiple Institutional Board (COMIRB) approval was obtained prior to patient recruitment (Protocol #07-0640). At the time of recruitment, all patients meeting the inclusion criteria were given a brief explanation of the study by the principal investigator, consented to participation in the study, and signed the necessary consent forms. A script was used for patient recruitment and for the courtesy telephone calls (Appendix 1). Random group allocation and coding of patients was completed by a co-investigator. Both the subjects and principal investigator were blinded to the group allocation. In the non-pharmacologic subject groups, the main investigator was not blinded to the group allocation because the patients needed to be contacted.
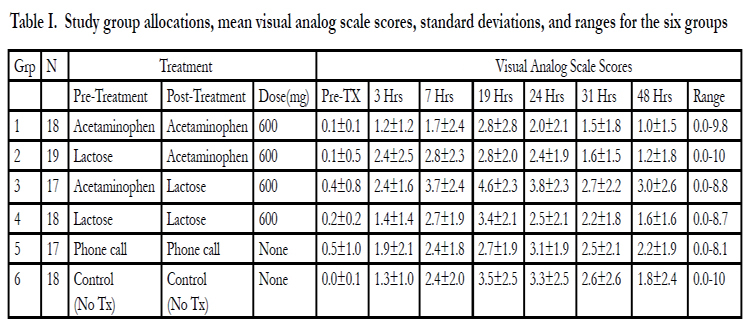
For the pharmalogical part of the study, each patient was given nine copies of a 100mm Visual Analog Scale (VAS) along with one medication envelope with two pre-treatment tablets and one envelope containing twelve post-treatment tablets (if they were assigned to groups 1-4) (Table I). The acetaminophen and placebo tablets were compounded by a licensed pharmacist (Wise Pharmacy, Littleton, CO) according to our specifications and were all identical in shape and color. The final sample (Table I) consisted of 107 patients: Group 1 (6 males, 12 females), Group 2 (9 males, 10 females), Group 3 (8 males, 9 females), Group 4 (8 males, 10 females), Group 5 (4 males, 13 females), Group 6 (8 males, 10 females). The other thirteen patients did not return for follow-up visits in a timely manner and were dropped from the study.
In the pharmacologic part of the study the following protocol was used: Group 1 took two 300 mg acetaminophen tablets orally 1 hour prior to initial archwire placement and two 300 mg tablets acetaminophen after each of the scheduled VAS survey recordings (Table I); Group 2 took two lactose tablets (placebo) orally 1 hour prior to initial archwire placement and two 300 mg acetaminophen tablets orally after each of the scheduled VAS survey recordings (Table I); Group 3 took two 300 mg acetaminophen tablets orally 1 hour prior to initial archwire placement and two lactose tablets were taken orally after each of the scheduled VAS survey recordings (Table I); and Group 4 took two lactose tablets orally 1 hour prior to initial archwire placement and two lactose tablets orally after each of the scheduled VAS survey recordings (Table I). The patients in the pharmacologic part of the study were not contacted by telephone by the investigator or any other orthodontic provider the day prior to or the day following the initial archwire insertion appointment.
Table I. Study group allocations, mean visual analog scale scores, standard deviations, and ranges for the six groups.
In the non-pharmacologic part of the study the following protocol was followed: Group 5 patients were contacted by telephone by the investigator the day prior to and the day following the initial archwire insertion appointment and in Group 6 the patients were not contacted by telephone by the investigator or any other orthodontic provider the day prior to or the day following the initial archwire insertion appointment, serving as the control.
All subjects were asked to mark their degree of discomfort (0 being no pain and 10 being the worst pain imaginable) on the VAS survey at that moment, prior to appliance placement. This initial marking constituted the baseline point (pre-treatment). The principal investigator monitored the first recording (baseline) to assure the subject’s full comprehension of treatment protocols. Immediately following the initial recording, the patients in Groups 1-4 took the first two tablets orally. The patients had fixed orthodontic appliances placed on at least one arch (with 10 teeth minimum) and an initial archwire inserted. The subjects were discharged following the archwire insertion and instructed to continue marking their levels of discomfort on the VAS surveys at 3, 7, 19 (next morning), 24, 31 (following night after dinner), and 48 hours. No discrimination was made between various activities (eating, chewing, or biting). Immediately following each recording, the subjects in Groups 1-4 were instructed to take 2 tablets of the medications provided. The VAS recording followed by medication intake was performed at each of the time points starting at the baseline mark, up to 48 hours. Excluding baseline, each subject made a total of six (6) recordings and subjects in Groups 1-4 took medication total of 6 times.
The subjects were instructed to take the medication unless their pain level (VAS recording) was zero because the side effects of the medications were extremely low to almost none at the dosages used. When the patient’s VAS recording was zero (0), they were instructed to record that they stopped taking the study medication. The subjects were encouraged not to take any additional analgesics. However, if absolutely necessary, they were allowed to take whatever they usually took for pain but were required to record the exact time, dosage, and type of medication taken and whether it relieved their pain or not. For younger patients (less than 15 years old), the parents were asked to monitor the scheduled medication intakes, but the subject recorded his/her pain levels, not their parents. The VAS booklet was returned to the principal investigator in person at one of their regularly scheduled appointments. After the questionnaire was returned in full, each subject was compensated $10 for participation. If a subject took any additional medication, then the VAS scores only up to that point were used for analysis. Participation in this study, howhowever, had no bearing on the subjects’ treatment and all treatment proceeded as normal, whether or not they participated and completed the study.
Descriptive statistics were calculated at each time interval for the groups. A two-way Analysis of Variance (ANOVA) was used to compare differences in mean pain scores between the six groups. If the results of the two-way ANOVA were found significant, then a one-way ANOVA was carried out for each time interval. A Student t-test was also used to test differences between males and females. The level of statistical significance in this study was set at p≤0.05.
Results
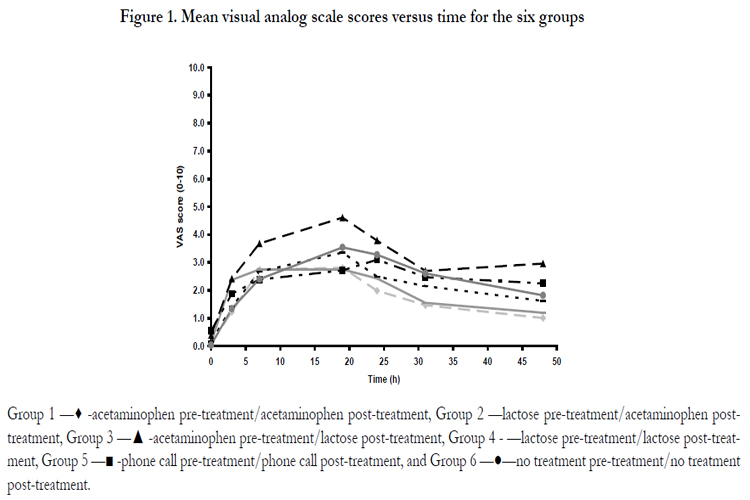
Results are reported in Table I and Figure I. Inferential statistics found no differences between males and females at any time points studied. Therefore, both genders were combined for analysis. Graphic views of the findings are presented in Figure 1. A comparison of time and treatment groups was performed and no significant differences were found.
Group 1 —♦ -acetaminophen pre-treatment/acetaminophen post-treatment, Group 2 —lactose pre-treatment/acetaminophen posttreatment,Group 3 —▲ -acetaminophen pre-treatment/lactose post-treatment, Group 4 - —lactose pre-treatment/lactose post-treatment,Group 5 —■ -phone call pre-treatment/phone call post-treatment, and Group 6 —●—no treatment pre-treatment/no treatment post-treatment.
In all six groups there was a trend for pain to start 3 hours following archwire insertion and to gradually increase to a peak level at 19 hours (next morning). The pain level then gradually decreased from 31 hours to 48 hours, but did not return to the pre-treatment baseline. The highest average pain level occurred in Group 3 (acetaminophen, lactose) at 19 hours, but the pain level was only moderate (VAS score of 4.6 on a 0-10 scale). There is a trend starting at 7 hours indicating that post-archwire insertion acetaminophen and courtesy telephone calls decreased the pain level (VAS scores) more than in the control groups, the differences did not rise to statistical significance at any of the studied times. There was a wide range of VAS scores reported (Table I). The highest VAS scores at 19 hours in the groups were 9.8 (Group 1), 8.1 (Group 2), 8.8 (Group 3), 7.1 (Group 4), 6.6 (Group 5), and 9.5 (Groups 6). Five patients in the study took additional medication. Three patients self-administered ibuprofen (one patient in Group 4-lactose/lactose, one patient in Group 5-phone call/phone call, and one patient in Group 6-no treatment). Two patients self-administered Tylenol (Group 6-no treatment). The VAS scores of those patients that self-administered additional medication were excluded from analysis at the time point they took the additional medication and for the remaining times.
When averaging all treatments together over time, the pain recordings were significantly higher at 7, 19, and 24 hours than at the beginning or end time points. There were no statistical differences between the scores either for the absolute scores or change in scores from the baseline value.
Discussions
Previous studies examined gender, timing, and type of medication administered. Several studies[2,14,15,16] found no correlation between pain and gender. In our study, no gender differences were found for VAS scores and, therefore, both genders were combined for data analysis. The onset of pain in all six groups was observed at the second recording (3 hours) and the peak pain level was recorded at 19 hours (following morning) post-archwire insertion. The findings of this study agreed with those of Salmassian et al[7] and Bernhardt et al.[11] The findings of Ngan et al[16]are also similar, finding discomfort at 4 hours post-archwire insertion or post-separator insertion, but they found the peak pain at 24 hours post-treatment. Polat et al[17] found peak pain levels the first night approximately 24 hours post-archwire insertion because of when they took the measurement. Our study found a trend of lower pain with administration of acetaminophen than with the placebo both pre- and post-archwire insertion; however, this apparent trend was not statistically significant. The Polat et al study[17] had a larger sample (20 patients per group) and also did not find a statistically significant difference between ibuprofen and a placebo. Orthodontic pain studies rarely have sample sizes that are significantly large, which is a limitation.
Pre- and post-treatment telephone calls did have an effect on the subject’s perceived pain, resulting in a trend of lower pain than the control subjects, but this apparent trend was not statistically significant. In addition, the telephone calls resulted in an apparent trend of lower pain than the analgesic groups, but this trend again was not statistically different. This trend of lower perceived pain experiences following archwire insertion with pre-treatment and follow-up calls was also observed by Bartlett et al.[13]
The absence of statistically significant differences between the six groups may be explained in several ways. Pain is subjective and wide individual variation exists. Many obstacles exist when measuring pain and the amount of pain experienced.[2,5,14,18] Since pain is experienced on an individual basis; large variability was observed in the VAS scores. Several patients did not report any pain during the study period even though they were in the control group and did not receive analgesics or follow-up calls. Other patients were administered 600 mg acetaminophen pre- and postarchwire insertion and still reported high individual scores of 9 and above on the VAS survey. The multifactorial and individual basis of pain perception between individuals contributed to the lack of statistically significant differences in the groups.
An additional explanation is that the pain due to initial archwire insertion during orthodontic treatment is so mild for most individuals that no analgesic is required. Since groups receiving a placebo and the control (no treatment) experienced the same analgesic effect as acetaminophen or courtesy phone calls, it is possible that the pain due to orthodontic treatment was so minimal that most patients can effectively control the pain with nothing at all. Scheurer et al[19] also found a low percentage of patients requiring analgesics post-orthodontic treatment. The results of our study were similar. During the VAS recordings to 48 hours postarchwire insertion, the highest average VAS score was only 3.7 on a 0-10 scale, which was also reported by the group that was given lactose placebo tablets post-archwire insertion. An average of 3.7 is only mild to moderate pain and could be effectively managed without analgesics for many patients.
It is also possible that no differences were found between groups in our study because the dosages used were too low to be effective. Polat et al[17] found that increasing the analgesic frequency was recommended because one preoperative dose was not considered to be adequate to control discomfort. Our study used the smallest dose recommended by the manufacturer. Additional research with higher dosages of pre-archwire insertion acetaminophen may be necessary to see any significant differences; however, higher doses may not be justified due to the mild nature of the pain.
Olson et al[20] compared the efficacy of acetaminophen (1000mg) and a placebo to treat dental pain and found statistically significant differences. However, their study had a sample size of 66 patients, used double the acetaminophen dose that we used, and studied patients with more significant dental pain than what occurs with orthodontic treatment. Other studies[21,22] examined the pain control following oral operative procedures, such as impacted third molar removal. Since these surgical pain studies found statistically significant differences between the analgesic and placebo groups, their findings are probably an example of the large difference between the pain from oral surgery and the minimal pain from orthodontic treatment. In our study the highest average pain levels were low for the all groups: acetaminophen/acetaminophen (2.8), lactose/acetaminophen (2.8), acetaminophen/lactose (3.8), lactose/lactose (3.4), phone call/phone call (3.1), and control (3.5). While individual patients reported higher and lower pain levels, on a 0-10 VAS scale, the average orthodontic pain reported was only mild to moderate, illustrating the subjective nature of pain and the wide individual variation of pain perception.
Additional methods to increase an analgesic’s effectiveness may incorporate psychological methods, such as follow-up or pretreatment telephone calls by the health care provider to ensure that the patient feels comfortable and at ease. Bartlett et al[13] found in a similar study that a pre-treatment phone call from the health care provider decreased anxiety and self-reported pain. Although our study did not find statistically significant differences between the medication groups (1-4) and the telephone call group (5), there was a trend of lower average VAS score in the groups that received telephone calls compared to the analgesic groups (1-4). Future studies using a combination of analgesics and telephone calls may show greater differences.
Pre- and post-archwire insertion analgesics, placebos, telephone calls, and no treatment were equally effective for orthodontic pain control. Pain control modalities may need to be customized based on the patient’s individual needs and pain responses. Due to acetaminophen’s proposed neutral effects on tooth movement movement,[23] it is a good adjunct to follow-up calls or when the patient is seeking a medication for their orthodontic pain. Therefore, orthodontic pain control should be customized to the individual patient.
Conclusions
1. No differences were found between males and females in reported pain levels.
2. Post-orthodontic pain peaks at 19 hours and then decreases.
3. Orthodontic pain is of low to moderate intensity with a wide individual variation.
4. Acetaminophen, placebo, courtesy telephone calls, and no treatment were all equally effective in controlling orthodontic pain.
References
- Oliver RG, Knapman YM (1985) Attitudes to orthodontic treatment. Br J Orthod 12:179-88.
- Jones M, Chan C (1992) The pain and discomfort experienced during orthodontic treatment: a randomized controlled clinical trial of two initial aligning arch wires. Am J Orthod Dentofacial Orthop 102:373-81.
- Bergius M, Kiliaridis S, Berggren U (2000) Pain in orthodontics. A review and discussion of the literature. J Orofac Orthop 61:125-137
- Doll GM, Zentner A, Klages U, Sergl HG (2000) Relationship between patient discomfort, appliance acceptance and compliance in orthodontic therapy. J Orofac Orthop 61:398-413. [
- Sergl HG, Klages U, Zentner A (1998) Pain and discomfort during orthodontic treatment: causative factors and effects on compliance. Am J Orthod Dentofacial Orthop 114:684-91.
- Hathaway D (1986) Effect of pre-operative instruction on postoperative outcomes: A meta analysis. Nurs Res 35:269-75.
- Salmassian R, Oesterle L, Shellhart C, Newman S ( 2007) Comparison of the efficacy of ibuprofen versus acetaminophen in controlling pain following orthodontic tooth movement. Am J Orthod Dentofac Orthop, accepted for publication.
- Kehoe MJ, Cohen SM, Zarrinia K, Cowan A (1996) The effect of acetaminophen, ibuprofen, and misoprostol on prostaglandin E2 synthesis and the degree and rate of orthodontic tooth movement. Angle Orthod 66:339-350.
- Walker JB, Buring SM. (2001) NSAID impairment of orthodontic tooth movement. Ann Pharmacother 35:113-15.
- Simmons KE, Brandt M (1992) Control of orthodontic pain. J In Dent Assoc 71:8-10.
- Bernhardt MK, Southard KA, Batterson KD, Logan HL, Baker KA, et al. (2001) The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. Am J Orthod Dentofacial Orthop 120:20-7.
- Miranda LS, Logan H, Southard KA, Parks CT. State-trait anxiety and discomfort levels experienced by orthodontics patients. Seq #220 – Orofacial Pain, TMD, and Xerostomia. iadr.confex.com/iadr/2002SanDiego/techprogram/abstract_12489.htm
- Bartlett BW, Firestone AR (2005) The influence of a structured telephone call on orthodontic pain and anxiety. Am J Orthod Dentofacial Orthop 128:435-41.
- Erdinc AM, Dincer B. ( 2004) Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod 26:79-85.
- Jones ML, Chan C (1992) Pain in the early stages of orthodontic treatment. J Clin Orthod 26:311-3.
- Ngan P, Kess B, Wilson S (1989) Perception of discomfort by patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop 96:47-53.
- Polat O, Karaman AL, Durmus E (2005) Effects of Pre-Operative Ibuprofen and Naproxen Sodium on orthodontic pain. Angle Orthod 75:791-96.
- Bergius M, Berggren U, Kiliaridis S (2002) Experience of pain during an orthodontic procedure. Eur J Oral Sci 110:92-8.
- Scheurer P, Firestone A, Burgin W (1996) Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod 18:349-57.
- Olson NZ, Otero AM, Marrero I, Tirado S, Cooper S, et al. (2001) Onset of analgesia for liquid gel ibuprofen 400mg, acetaminophen 1000mg, ketoprofen 25mg, and placebo in the treatment of post-operative dental pain. J Clin Pharmacol 41:1238-47.
- Dionne RA, Campbell RA, Cooper SA, Hall DL, Buckingham B (1983) Suppression of postoperative pain by preoperative administration of ibuprofen in comparison to placebo, acetaminophen, and acetaminophen plus codeine. J Clin Pharmacol 23:37-43.
- Forbes JA, Kehn CJ, Grodin CD, Beaver WT (1990) Evaluation of ketorolac, ibuprofen, acetaminophen and an acetaminophen-codeine combination in postoperative oral surgery pain. Pharmacother 10:94S-105S.
- Arias OR, Marquez-Orozco MC (2006) Aspirin, acetaminophen, and ibuprofen: Their effects on orthodontic tooth movement. Am J Orthod Dentofacial Orthop 130:364-70.