Clinical Manifestations of Demodicosis of Human Skin
Kravchenko A*
Russian Medical Academy of Continuous Professional Education of the Ministry of Healthcare of the Russian Federation, Barrikadnaya street, Moscow, Russia.
*Corresponding Author
Kravchenko A,
Russian medical academy of continuous professional education of the Ministry of Healthcare of the Russian Federation,
125993, 2/1 Barrikadnaya street, Moscow, Russia.
Tel: +44 7491814698
E-mail: angkravchenko@gmail.com
Received:October 04, 2017; Accepted: October 26, 2017; Published: October 28, 2017
Citation: Kravchenko A (2017) Clinical Manifestations of Demodecosis of Human Skin. Int J Clin Trails Case Stud. 2(2), 4-7.
Copyright: Kravchenko A © 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
The article presents the experience of observing the clinical picture of acne and rosacea in the presence of Demodex mites in therapeutically significant amounts found in preparations of human skin scraping (5 or more individuals per 1 cm2). In particular, observing different clinical cases of acne and rosacea with demodicosis, we consider it legitimate to divide demodecosis into primary and secondary.
2.Introduction
3.Materials and Methods
4.Results
4.1 A Clinical Example
5.Discussion
6.Conclusions
7.References
Keywords
ACNE; Demodex; Demodex Mites; Demodecosis; Rosacea; Treatment; Therapy; Clinical Cases; Reports; Metronidazole; Clinical Picture.
Introduction
Human skin mites, known as Demodex mites, belong to the genus Demodex, the family Demodicidae, suborder Trombidiformes, order Acariformes. For the first time the mite was identified by F. Berger in the earwax of a man's auditory canal in 1841. Then, F.G.J. Henle discovered mites on the human skin. A year later, in 1842, G. Simon revealed the main place of parasitizing mites - hair follicles. Having studied and described the morphological properties of mites, he named them Acarus folliculorum (from the Greek - "greasy animal"). Later G. Simon (1842) and R. Owen (1843) attributed the mites found to the genus Demodex [1]. The English acarologist S. Hirst (1917-1923) identified 21 species and several subspecies of Demodex mites in animals. Subsequently, studying the parasitizing of a mites on human skin, the Soviet scientist Akbulatova L.Kh. (1970) on the bases of laboratories based in the cities of Kokand (Uzbek SSR) and Leningrad, discovered and described two forms: Demodex folliculorum longus and Demodex folliculorum brevis [2].
Contrary to the well-known fact that Demodex mites are conditionally pathogenic parasites, none of the authors since the discovery of Demodex in the 19th century claims that this parasite is pathogenic to humans, and the identification of it on the skin is a dermatozoonosis, the issue of carrier mite is still open [3]. In addition, one can not ignore the fact that in the population it occurs in 55-100% of cases, including patients with no papulopustular eruptions on the skin of the face [4].
According to the studies of various authors described in the literature, there are two clinical variants of demodecosis: primary and secondary [1]. The diagnosis of primary demodecosis can be established if the following criteria are available:
- late debut of the disease (after 40 years);
- defeat of the face, mainly in perioral, periorbital, periauricular areas;
- asymmetric arrangement of inflammatory elements;
- subjective sensation of itching;
- high colonization of mites on the skin in the absence of acne and rosacea;
- remission of disease after therapy with acaricide medicines [5, 6].
Secondary demodecosis is exposed in the presence of Demodex mites in combination with cutaneous or other diseases (leukemia, HIV infection), with long-term use of topical glucocorticoids and calcineurin inhibitors [7, 8]. Secondary demodecosis begins at any age and is characterized by extensive areas of damage. These patients have a clinical picture of the corresponding diseases and a concomitant anamnesis.
In order to achieve the elimination of mites, antiparasitic (acaricides) medicines are used. Metronidazole, which is a derivative of 5-nitroimidazole, proved to be the most effective for many years. This medicine is administered at a course of 4 to 6 weeks [9].
Given the relevance of the research topic, we conducted clinical observations of acne and rosacea.
Materials and Methods
We conducted clinical observation of acne patients (n = 55) and rosacea (n = 45). The study included patients over the age of 18 with acne and rosacea on the skin of a person of varying severity in the absence of somatic complications in a history and after signing informed consent to participate in the study.
For the diagnosis of acne, the classification of the European Guidelines for the Treatment of Acne (EU Guidelines group, 2012) [10]:
- comedonal acne,
- mild - moderate papulopustular acne,
- Severe papulopustular acne, moderate nodular acne,
- Severe nodular acne, acne conglobata.
The diagnosis of rosacea was exposed using the improved classification of the American National Rosacea Society, proposed in 2002, according to which the following rosacea subtypes are distinguished:
Subtype I - erythematous-telangiectatic
Subtype II - papulopustular
Subtype III - fimatose
Subtype IV - ophthalmic [11].
All patients underwent scraping for the presence of Demodex mites before and after treatment. The study included patients who had a positive analysis with the presence of mites more than 5 individuals per 1 cm2. The material for analysis was taken with a sterile scalpel from the areas of the face that have the largest accumulation of sebaceous glands (nose, chin, inter brow area). The resulting material on the slide was placed in a drop of 10% KOH solution, then microscopies. Respondents included in the study were divided into two groups according to the treatment method. The course of treatment of patients was 20 days. Patients of I group received only topical therapy in the form of an ointment containing 7% metronidazole once a day. Patients of the II group received antiparasitic treatment in the form of metronidazole 250 mg 2 times a day inside and simultaneously external therapy in the form of an ointment containing 1% metronidazole once a day.
Results
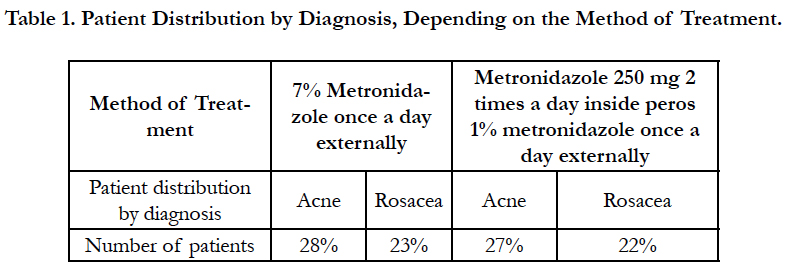
The study included patients with acne complicated by demodecosis - 55 people, rosacea patients complicated by demodecosis - 45 people. According to the chosen scheme of treatment in group I included 28 people with a diagnosis of acne and 23 people diagnosed with rosacea. Group II consisted of 27 patients with acne and 22 patients with rosacea (Table 1).
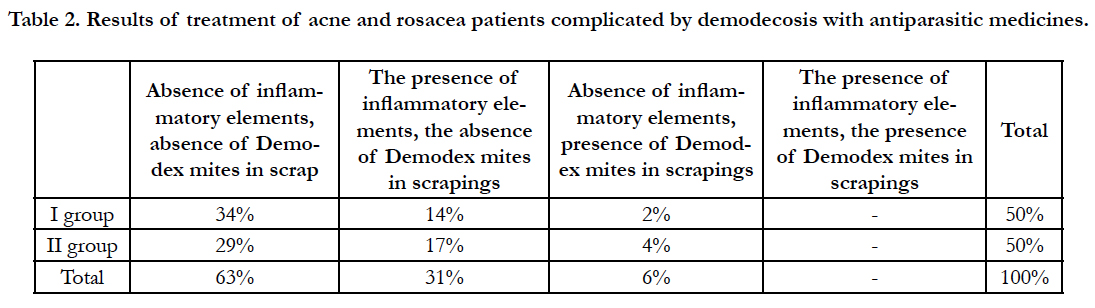
After the end of treatment, all patients were repeatedly scraped for the presence of Demodex mites. The results of the treatment were evaluated according to the data obtained after a laboratory study of the presence/absence of Demodex mites, as well as the clinical picture, and are presented in Table 2. The clinical picture was assessed by the condition of the pathological skin process-the presence and localization of morphological elements, regression, appearance or complete disappearance of the inflammatory process. For a more objective assessment, we photographed patients before and after the treatment.
Table 2. Results of treatment of acne and rosacea patients complicated by demodecosis with antiparasitic medicines.
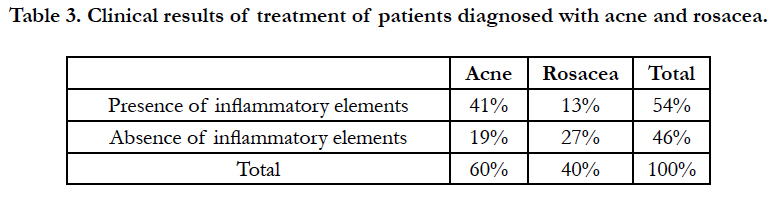
Thus, clinical recovery and complete sanation reached 34% of patients treated only with topical medication and 29% receiving general therapy. Inflammation persisted with complete sanation in 14% of the first group and in 17% of patients in the second group. At the same time, clinical recovery was observed in 6% of patients with preservation of Demodex on the skin. Comparing the percentage of patients with clinical recovery in the absence of Demodex mites in scrapes using external therapy with systemic therapy (34% and 29%, respectively), it can be concluded that external therapy with higher concentrations of metronidazole is not only more effective, but also avoids systemic application of the drug with the subsequent possible development of adverse events. Table 3 shows the clinical results of treatment for patients diagnosed with acne and rosacea.
As can be seen from the table, after the antiparasitic treatment, in most patients (41%) the inflammatory elements on the skin of the face continued to persist, in the presence of a diagnosis of "Rosacea", on the contrary, in 27% of patients the pathological process regressed.
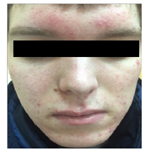
Figure 1 shows the clinical case of a patient before and after therapy.
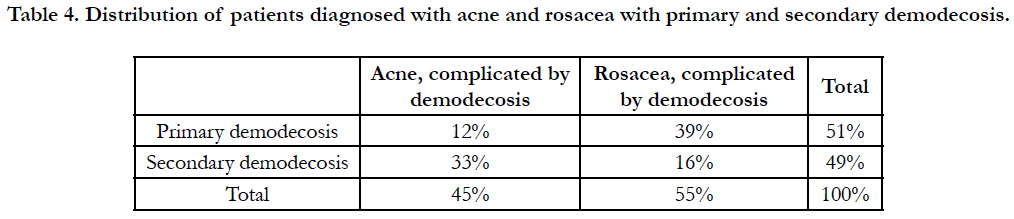
Table 4. Distribution of patients diagnosed with acne and rosacea with primary and secondary demodecosis.
The patient of 28 years has addressed with complaints to rashes in the field of the face, an itch. Acne is sick for 14 years. The onset of the disease is associated with hormonal changes in the body during the transition years. Previously, as a treatment used tar soap. In the scrapie before treatment, 7 Demodex folliculorum longus mites were found to be 1 cm2. Diagnosis: Acne, papulopustular form. Demodecosis. Treatment: 7% metronidazole cream on the entire surface of the face once a day for 20 days.
The results of treatment after a month: in scrapings - the absence of mites, the preservation of pathological elements on the skin of the face in the form of pustules of red and pink, closed comedones, perifocal erythema. Despite the preservation of pathological elements, photographs show an improvement in the clinical picture after antiparasitic treatment.
Discussion
In the course of the observation, it can be stated that the mites were found both in acne patients and in patients with rosacea. However, the greatest duration of the disease was noted in patients with rosacea. Assessing the clinical picture of patients after antiparasitic treatment, it should be noted that the acne patients, in most cases, retained inflammatory elements, while in most patients with rosacea the pathological process regressed. In the opinion of the authors, in cases where inflammatory elements on the skin of a person are completely resolved with a negative analysis for mites, the diagnosis of demodecosis is considered primary. In the presence of inflammatory elements and the absence of mites in scrapings, the main diagnosis is acne or rosacea, demodecosis is secondary [1]. Therefore, in the absence of inflammatory pathological elements on the skin of the face and in the presence of Demodex mites in scrapings of less than 5 individuals per 1 cm2, treatment of patients is impractical.
The analysis of the obtained data made it possible to distribute patients to primary and secondary demodecosis (Table 4).
As can be seen from the table, most often secondary demodecosis was observed in acne patients, and in primary rosacea patients primary demodecosis was diagnosed.
Conclusions
Thus, according to our observations, primary demodecosis in most cases was observed in patients with rosacea (39%), secondary demodecosis in patients with acne (33%). Clinical observations prove the necessity of conducting demodecosis diagnosis in the presence of papulopustular eruptions on the face skin. The presence of Demodex mite can cause a primarylesion of the skin in the form of inflammatory elements that are resolved after appropriate antiparasitic therapy, or complicate the course of diseases such as acne and rosacea. Achievement of patients in a greater percentage of cases of clinical and laboratory improvement with the use of high-concentration metronidazole topical allows to avoid the systemic effect of the drug on organs and systems.
References
- Chen W, Plewig G. Human demodicosis: revisit and a proposed classification. Br J Dermatol. 2014 Jun;170(6):1219–1225. PubMed PMID: 24471456.
- Akbulatova LK. The pathogenic role of mite Demodex and the clinical form of demodicosis in man. Vestn Dermatol Venerol. 1966 Dec;40(12): 57-61. PubMed PMID: 6000237.
- Baima B, Sticherling M. Demodicidosis revisited. Acta Derm Venereol. 2002;82(1):3–6. PubMed PMID: 12013194. PubbMed PMID: 12013194.
- Lacey N, Kavanagh K, Tseng SC . Under the lash: Demodex mites in human diseases. Biochem (Lond). 2009 Aug 1;31(4): 2–6. PubMed PMID: 20664811.
- Pallotta S, Cianchini G, Martelloni E, Ferranti G, Girardelli CR, Di Lella G et al. Unilateral demodicidosis. Eur J Dermatol. 1998 May;8(3):191–2. PubMed PMID: 9649702.
- Plewig G, KligmanAM. Acne and Rosacea. 3rd ed. Berlin Heidelberg: Springer;2000.
- Antille C, Saurat JH, Lubbe J. Induction of rosaceiform dermatitis during treatment of facial inflammatory dermatoses with tacrolimus ointment. Arch Dermatol. 2004 Apr;140(4):457–60. PubMed PMID: 15096374.
- Benessahraoui M, Paratte F, Plouvier E, Humbert P, Aubin F. Demodicidosis in a child with xantholeukaemia associated with type 1 neurofibromatosis. Eur J Dermatol. 2003 May;13(3):311–12.
- Hsu CK, Hsu MM, Lee JY. Demodicosis: A clinicopathological study. J Am Acad Dermatol. 2009 Mar;60(3):453–62. PubMed PMID: 19231642.
- Nast A, Dreno B, Bettoli V, Degitz K, Erdmann R, et al. Guidelines for the Treatment of Acne. JEADV. 2012 Feb; 26(s1): 1-29.
- Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification of rosacea: Report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002 Apr;46(4):584-7.