Assessment of Right Ventricular Function In Patients with Inferior Wall Myocardial Infarction by Echocardiography
G Rami Reddy, A Sarat Kumar Patra, M Shobana, P Arunachalam*
Department of cardiology, Meenakshi Academy of Higher Education and Research, Meenakshi Medical College Hospital and Research Institute, Kanchipuram, Tamil Nadu, India.
*Corresponding Author
P. Arunachalam,
Professor and Head, Department of Cardiology, Meenakshi Medical College Hospital and Research Institute,
Enathur, Kanchipuram, Tamil Nadu, India.
Tel: 9000770148
E-mail: p.arunachalam@gmail.com
Received: January 05, 2019; Accepted: December 05, 2019; Published: December 07, 2019
Citation: G Rami Reddy, A Sarat Kumar Patra, M Shobana, P Arunachalam. Assessment of Right Ventricular Function In Patients with Inferior Wall Myocardial Infarction by Echocardiography. Int J Cardiol Res. 2019;6(3):146-151. doi: http://dx.doi.org/10.19070/2470-4563-1900025
Copyright: P Arunachalam© 2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: In the present study was investigate the comparison of various echo methodologies in assessing Right Ventricular function in the setting of Inferior wall myocardial infarction with and without right ventricular involvement. Right ventricular dysfunction and stunning frequently is of a transient nature, such that estimation of its true incidence is even more difficult. Criteria have been set for to diagnose RVMI; but, even when strictly employed, the criteria lead to underestimation of the true incidence of right ventricular infarction.
Materials and Methods: The study is a prospective case control study involved 124 patients. Both male and female patients are selected for the study. There was no age limit in our study population with a first Q wave acute inferior myocardial infarction with or without RVMI.
Results: During the study period, 104 patients were evaluated and underwent a complete echo-Doppler examination. Among these patients, 44 had an RVMI, and constituted Group 1, and the remaining 60 patients had an inferior wall myocardial infarction without right ventricular involvement of Group 2.
Conclusion: We conclude that Echo- Dopper assessment was significantly differentiating the early diastolic velocity in patients with RVMI and without RVMI.
2.Materials and Methods
2.1 Experimental Design
2.2 Electrocardiography
2.3 Echocardiography
2.4 RV Dimensions
2.5 Right ventricular contractile function
3.Results
3.1 Electrocardiography
3.2 Echocardiography.
4.Discussion
4.1 Tissue Doppler Imaging
5.Conclusion
6.References
Introduction
Inferior wall myocardial infarction in complicated by right ventricular infarction (RVMI) in as much as 50% of cases. In a series by Anderson et al., in 1989, the incidence of RVMI in patients with inferior wall myocardial infarction was between 10 – 50%. Isolated infarction of the right ventricle is extremely rare [1].
Although right ventricular infarction is clinically evident in a sizable number of cases, the incidence is considerably less than that found at autopsy.1 A major reason for the discrepancy is the difficulty in establishing the presence of RVMI in living patients [2, 3].
In patients with RVMI, the risk of death in the hospital is high and major complications are greater. Right ventricular infarction contributes markedly to hemodynamic instability, atrio-ventricular conduction blocks, and in-hospital mortality in patients with inferior wall myocardial infarction. Systolic right ventricular function is an important predictor in the course of myocardial infarction. Despite this initial observation nearly two decades ago, this condition has received little clinical attention until recent years [4, 5].
According to the Shock Trial Registry 38, despite the younger age, lower rate of anterior MI, and higher prevalence of single vessel coronary disease of RV compared with LV shock patients, and their similar benefit from revascularization, mortality is unexpectedly high in patients with predominant RV shock and similar to patients with LV shock [6].
Cardiogenic shock and the requirement for temporary transvenous cardiac pacing are more common in patients with right ventricular dilatation. Furthermore, by implying multivessel coronary artery disease, the presence of right ventricular dysfunction carries an adverse prognosis irrespective of infarct location [7]. The demonstration of right ventricular dysfunction is important because it is often associated with a distinct clinical syndrome requiring specific management. In the presence of low cardiac output volume loading to restore left ventricular filling pressure is required [8, 9]. Inappropriate vasodilator and/or diuretic therapy may prove fatal. Information about right ventricular function can be applied in thrombolysis decision making when a relative contraindication is present. In fact, the findings of one study suggested that patients with inferior myocardial infarction derived no benefit from thrombolysis in the absence of right ventricular involvement. Interest in recognizing right ventricular infarction non-invasively has grown because of the therapeutic implications of distinguishing patients with right ventricular dysfunction from those without right ventricular dysfunction [10].
Materials and Methods
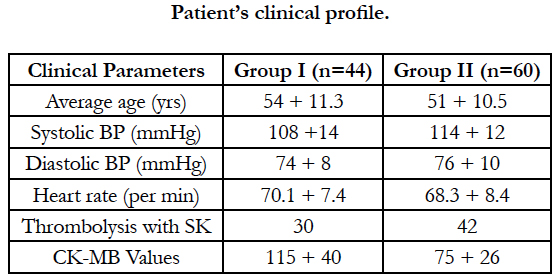
The present study was carried out period from November-2017 to October 2018 in Department of Cardiology, Meenakshi Medical College and Research Institute, Kanchipuram. Ethical clearance was obtained from institution ethical committee. The study is a prospective case control study involved 124 patients. Both male (78) and female (26) patients are selected for the study. There was no age limit in our study population with a first Q wave acute inferior myocardial infarction with or without RVMI.
The patients were divided into two groups:
Group 1 - Patients with IWMI with RVMI (n = 51)
Group 2 - Patients with IWMI without RVMI (n = 73)
Out of the 124 patients, 20 patients (7 from Group 1 & 13 from Group 2) were excluded from the study due to various reasons described below.
20 patients were excluded from the study due to- Delayed presentation >2 days after onset of chest pain (n=8) and Presence of preexisting cardiac dysfunction due to myocardial infarction, corpulmonale, DCM or valvular heart disease (n=6)-Atrial fibrillation (n=1) - Technically inadequate echo (n=5).
Finally, Group 1 (IWMI with RVMI) consisted of 44 patients and Group 2 (IWMI without RVMI) consisted of 60 patients, and these 104 patients underwent clinical evaluation, investigations including EKG, Echocardiography and coronary angiography in whom-ever it was feasible.
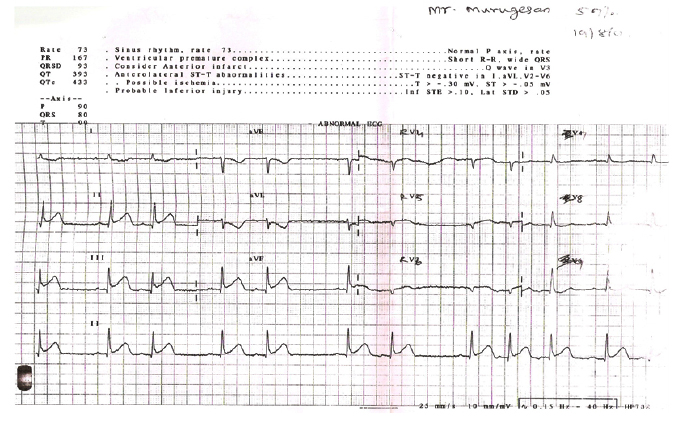
ECG changes, including an ST segmental elevation of greater than 0.1 mV with or without Q waves in at least two of the leads II, III, and aVF, also were required. In all patients, a standard 12 lead ECG and right precordial leads (V3 to V6R) were recorded at hospitalization. A 1mm ST segment elevation with or without Q waves in V4R lead was required to diagnose the involvement of the right ventricle.
Transthoracic echocardiography was performed in each patient using a Philips HD7.
echocardiography machine with a 3.5 MHz transducer including second harmonic and tissue Doppler imaging technology. Echocardiography was done within 24 hours of symptom onset whenever technically possible and in all patients within 48 hours of symptom onset. Subjects were examined in supine, left-lateral position. They underwent conventional M-mode and two dimensional echocardiography from a left parasternal and apical window. The baseline LV volumes and ejection fraction were calculated by Simpson’s biplane method.
The following measurements were done using Philips HD7. RT echo machine:
- RV dimensions
- RV contractile function & Inter-ventricular septum movement
- Tricuspid regurgitation jet & Pulmonary artery systolic pressure
- Tricuspid annular movement - M-mode
- Doppler tissue imaging – lateral & septal wall systolic/early, late diastolic velocities
- Myocardial performance index (Tei index)
Right and left ventricular end diastolic diameters in the supine position using the same M-mode cross-section in the parasternal long axis view. Normal values were defined as less than 26 mm for the right ventricular end diastolic diameter, greater than 37 mm for the left ventricular end diastolic diameter, and less than 0.5 for the ratio of the right ventricular diameter to the left ventricular diameter 26.
Right ventricular wall motion was assessed in parasternal long axis, parasternal short axis, RV inflow and apical four chamber views. The right ventricle was divided into anterior wall of RVOT, anterior free wall, lateral free wall and inferior wall. Each segment was analyzed as normal, hypokinetic, akinetic and dyskinetic.
Results
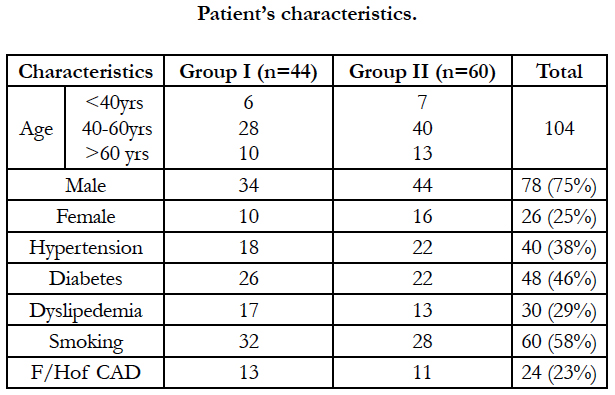
During the study period, 104 patients were evaluated and underwent a complete echo-Doppler examination. Among these patients, 44 had an RVMI, and constituted Group 1, and the remaining 60 patients had an inferior wall myocardial infarction without right ventricular involvement (Group 2).
Most of the patients were in the age group of 40-60 years (68/104 = 65%).
Most of the study population were male patients, with 78 out of the 104 patients being male (75%), the rest 26 patients were female.
As far as the history was concerned, 40/104 (38%) were hypertensives, 48/104 (46%) had a history of diabetes mellitus, 60/104 (58%) of patients were smokers, and a family history of ischemic heart disease was evaluated in 24/104 patients (23%).
Various complications were noted in the study patients, the commonest being conduction disturbances. Conduction disturbances were noted in 15/44 patients (34%) of Group 1, and in only 6/60 (10%) of patients in Group 2. Cardiogenic shock complicated 3/44 patients (7%) of Group 1, and none of the patients in Group 2.
Pulmonary artery systolic pressures >30mmHg were noted in 30/44 (69%) of Group 1, while in Group 2 patients, only 1/60 patients (2%) had PASP exceeding 30mmHg.
8 patients died due to complications of which 7 patients belonged to Group 1 and 1 patient belonging to Group 2 died. All patients died within 1 week of the acute event. Elevated pulmonary artery pressures were noted in 7/8 patients who died with a mean pulmonary artery systolic pressures of 40mmHg. We can hypothesize that patients with persisting sign of pulmonary hypertension did not experience reperfusion of the related artery and had an unfavorable course.
12 lead electrocardiography was done in all patients. Right sided chest leads and posterior wall leads were also placed and ECG recorded in all patients. By using the criteria described in methods, the culprit artery was identified as Proximal RCA – 42 patients, Distal RCA – 45 patients, Left circumflex – 17 patients.
Evidence of right ventricular involvement as defined by 1mm ST elevation in V4R was fund in 38 patients (of which, 34 patients had proximal RCA as the culprit vessel on ECG and 4 had left circumflex as the vessel causing myocardial infarction).
Echocardiography was done in all 104 patients within 48 hours after the onset of the acute event, of which, echocardiography was done within 24 hours of symptom onset in 48 patients. The results of the investigation is as below:
-RV end-diastolic diameter was increased in patients with RVMI, compared with those without RV involvement (Picture 9), although it failed to achieve statistical significance (p=0.1).
RV contraction abnormalities and IV septal motion abnormalities were noted in 41% of patients with RVMI, and only in 3% of patients without it. Significantly, the wall motion abnormalities were noted in those patients who had their echo done within 24 hours of symptom onset, stressing the fact that, the right ventricle recovers fast after an ischemic insult.
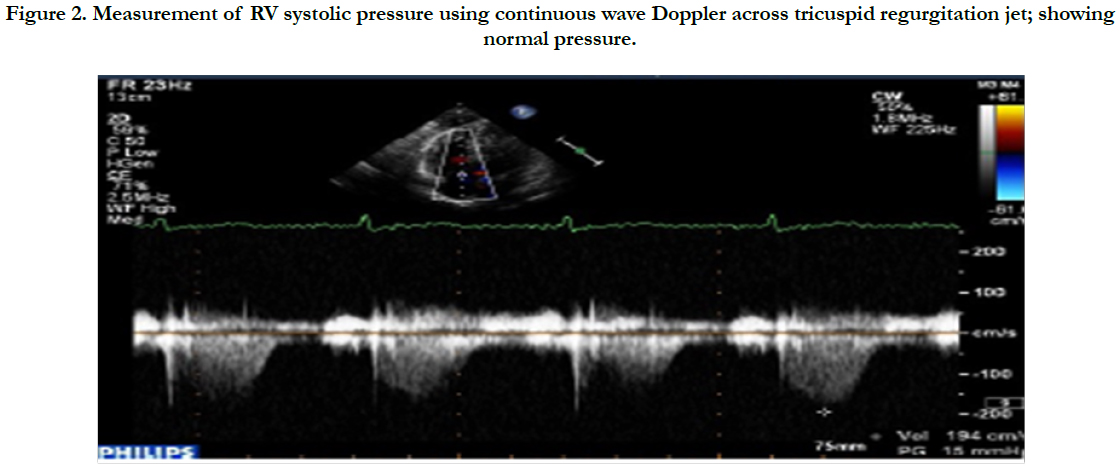
Tricuspid regurgitation was noted in nearly half of the patients with right ventricular involvement; this regurgitation, when quantified by colour doppler, was mild in a majority of cases, moderate in some and severe in none.
The pulmonary artery systolic pressure was slightly elevated and above normal in patients of Group 1, compared to Group 2, statistically not significant (p=0.2).
Figure 2. Measurement of RV systolic pressure using continuous wave Doppler across tricuspid regurgitation jet; showing normal pressure.
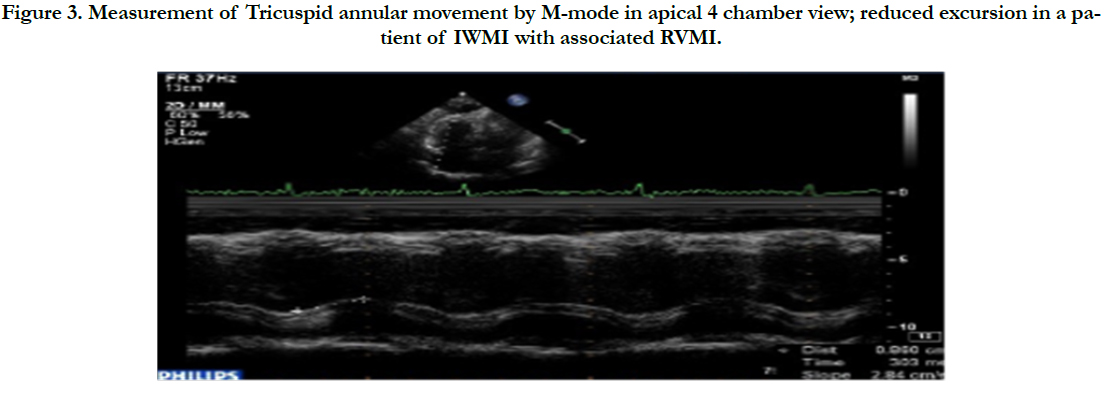
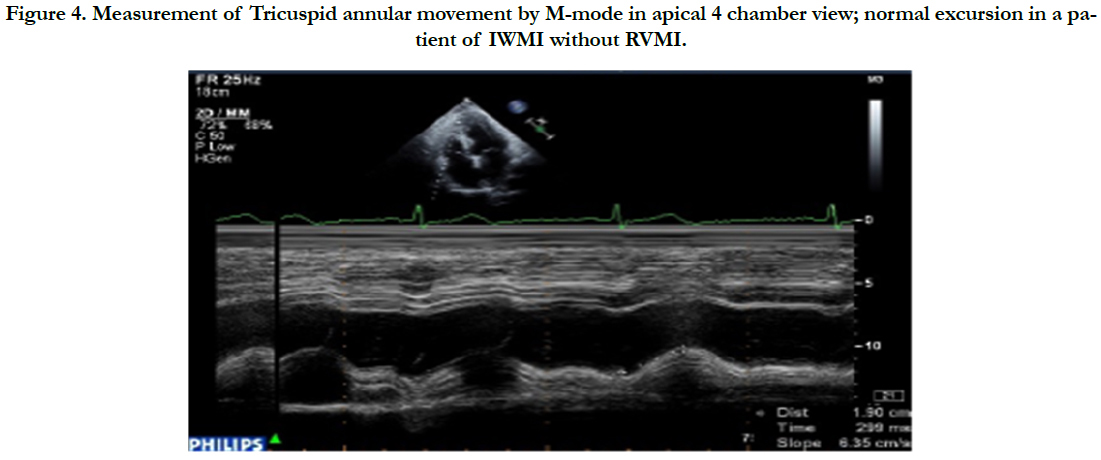
The tricuspid annular excursion was statistically significantly decreased in patients with right ventricular myocardial infarction, signifying that RV systolic function was depressed in those patients (p=0.05).
Figure 3. Measurement of Tricuspid annular movement by M-mode in apical 4 chamber view; reduced excursion in a patient of IWMI with associated RVMI.
Figure 4. Measurement of Tricuspid annular movement by M-mode in apical 4 chamber view; normal excursion in a patient of IWMI without RVMI.
Myocardial performance index was found to be statistically significant, it is raised to nearly two fold the reference values in patients with RVMI; the values were not much high compared to controls in those without right ventricular involvement. (p=0.01).
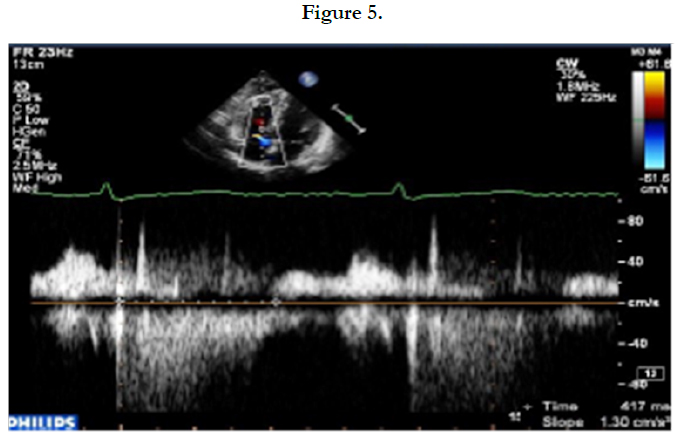
Tissue doppler was done in the right ventricular free wall and the septal regions and the systolic (Sm), early diastolic (Em) and late diastolic (Am) velocities were noted. It was found that the right ventricular free wall Sm and Em values were statistically significantly depressed in patients with right ventricular myocardial infarction (p=0.02). The values were near normal in those without RV involvement. However, the RV free wall late diastolic velocities (Am) and the septal velocities did not differ much in patients with and without right ventricular myocardial infarction (p=0.22).
Discussion
In patients with RVMI, the risk of death in the hospital is high and major complications are greater. Right ventricular infarction contributes markedly to hemodynamic instability, atrio-ventricular conduction blocks, and in-hospital mortality in patients with inferior wall myocardial infarction. Systolic right ventricular function is an important predictor in the course of myocardial infarction. The poorer outcomes among patients with RVMI are not mediated entirely by RV dysfunction.
Recent research points towards a new explanation for the higher complications even when the extent of RV infarction is small. Stimulation of RV vagal afferents by stretch leads to cardioinhibitory Bezold- Jarish reflex resulting in higher than expected incidence of complications especially in the first few days after acute coronary event with RV involvement.
The use of electrocardiography for the diagnosis of right ventricular infarction, which is the most common modality used, also lacks sensitivity and specificity and the changes are also transient in nature. Hence, the need for other non-invasive modalities for the assessment of right ventricular function in the presence of right ventricular myocardial infarction.
In an extensive adult patient population, a Swiss study [11] demonstrated that TDI of the systolic lateral tricuspid annular long axis velocity (TVlat) is accurate to characterize systolic RV function independent of most, pathophysiologically meaningful cofactors. A velocity of 12 and 9 cm/s differentiates among normal and moderately reduced RV ejection fraction, respectively between moderately and severely impaired RV EF.
Since it is only above 40 mm Hg that pulmonary artery pressures impacts on TVlat, it affects the relationship between TVlat and RV EF especially in patients with pure PAHT in whom the former cannot be used for RV function assessment. With regard to the specific TVlat threshold value of 12 cm/s for the distinction between normal and impaired RV function in our investigation, the study by Oezdemir [12] and coworkers using RV TDI has to be cited, because it found an identical cut-off with almost identical sensitivity and specificity of 81 and 82% for the diagnosis of RV myocardial infarction. The limitations of TDI is that it represents myocardial motion only in the longitudinal direction, and not in the circumferential plane.
Furthermore, on the basis of the correlation between isovolumic contraction velocity at basal segment and right atrial mean pressure, we tested the sensitivity and specificity of a cut off value below 6 cm/s indicating an increased right atrial pressure (>6mmHg). The sensitivity and specificity were 100% and 78%, respectively [13]. These findings may be of importance as disturbance of myocardial motion occurs predominantly during the isovolumic phases (i.e. contraction and / or relaxation), and may therefore be a sensitive marker for myocardial dysfunction.
Alam et al., [14] in his study from Sweden, patients with RV infarction had a significantly decreased peak systolic tricuspid annular velocity (13.3 and 10.3 cm/s, P<.001) and peak early diastolic velocity (13 and 8.2 cm/s, P<.001) when compared with patients with inferior wall myocardial infarction without RV involvement.
Mustafa Yilmaz et al., [15] in his study of forty-eight patients with acute inferior myocardial infarction and 24 age- and sex-matched healthy controls were included in this study. Twenty-four patients had electrocardiographic signs of inferior myocardial infarction without right ventricular infarction (group I), and the other 24 patients had electrocardiographic signs of inferior myocardial infarction with right ventricular infarction (group II). From the echocardiographic apical four-chamber view, peak systolic, early diastolic, and late diastolic velocities of the tricuspid annulus at the right ventricular free wall were recorded with the use of pulsed-wave Doppler tissue imaging.
The tricuspid annular peak tissue Doppler imaging systolic velocity was significantly lower in group I (14.03 ± 2.57 cm/s, P<0.005) and in group II (8.50 ± 0.84 cm/s, P<0.005) than in controls (16.63 ± 2.31 cm/s).
Conclusion
In the present study we conclude that the tissue doppler imaging, right ventricular free wall systolic velocity and early diastolic velocity in patients with RVMI was less compared to patients without RVMI and the correlation was statistically significant.
References
- Bates ER, Clemmensen PM, Califf RM, Gorman LE, Aronson LG, George BS, et al. Precordial ST segment depression predicts a worse prognosis in inferior infarction despite reperfusion therapy. The Thrombolysis and Angioplasty in Myocardial Infarction (TAMI) Study Group. J Am Coll Cardiol 1990;16:1538-1544. PMID: 2123903.
- Cohn JN, Guiha NH, Broder MI, Limas CJ. Right ventricular infarction: clinical and hemodynamic features. Am J Cardiol 1974; 33: 209-214. PMID: 4810018.
- Nasmith J, Marpole D, Rahal D, Homan J, Stewart S, Sniderman A. Clinical outcomes after inferior myocardial infarction. Ann Intern Med 1982; 96: 22-26. PMID: 7053698.
- Radford MJ, Johnson RA, Daggett WM Jr, Fallon JT, Buckley MJ, Gold HK, et al. Ventricular septal rupture: a review of clinical and physiologic features and an analysis of survival. Circulation 1981; 64:545-553. PMID: 7020978.
- Geva T, Powell AJ, Crawford EC, Chung T, Colan SD. Evaluation of regional differences in right ventricular systolic function by acoustic quantification echocardiography and cine magnetic resonance imaging. Circulation 1998; 98: 339–345. PMID: 9711939.
- Louridas G, Angomachalelis N, Patakas D, Stavropoulos C. Right ventricular echocardiographic,vectorcardiographic and electrocardiographic study in cor pulmonale. Acta Cardiol 1980; 35: 429–436. PMID: 6453492.
- Bommer W, Weinert L, Neumann A, Neef J, Mason DT, DeMaria A. Determination of right atrial and right ventricular size by two-dimensional echocardiography. Circulation 1979; 60: 91–100. PMID: 445737.
- Levine RA, Gibson TC, Aretz T, Gillam LD, Guyer DE, King ME, et al. Echocardiographic measurement of right ventricular volume. Circulation. 1984; 69: 497–505. PMID: 6692511.
- Ishii M, Eto G, Tei C, Tsutsumi T, Hashino K, Sugahara Y, et al. Quantitation of the global right ventricular function in children with normal heart and congenital heart disease: a right ventricular myocardial performance index. Pediatr Cardiol. 2000; 21: 416–421. PMID: 10982698.
- Meluzín J, Spinarová L, Bakala J, Toman J, Krejcí J, Hude P, et al. Pulsed Doppler tissue imaging of the velocity of tricuspid annular systolic motion; a new, rapid, and non-invasive method of evaluating right ventricular systolic function. Eur Heart J. 2001; 22: 340–348. PMID: 11161953.
- Tüller D, Steiner M, Wahl A, Kabok M, Seiler C. Systolic right ventricular function assessment by pulsed wave tissue Doppler imaging of the tricuspid annulus. Swiss Med Weekly 2005;135: 461-468. PMID: 16208583.
- Oezdemir K, Altunkeser BB, Icli A, Ozdil H, Gok H. New parameters in identification of right ventricular myocardial infarction and proximal right coronary artery lesion. Chest 2003; 124: 219–26. PMID: 12853526.
- Lindqvist P, Waldenström A, Wikström G, Kazzam E. The use of isovolumic contraction velocity to determine right ventricular state of contractility and filling pressures. Euroechocardiography. 2005 Aug; 6(4): 264-70. PMID: 15992709.
- Alam M, Wardell J, Andersson E, Samad BA, Nordlander R. Right ventricular function in patients with first inferior myocardial infarction : Assessment by tricuspid annular motion and tricuspid annular velocity. Am Heart J. 2000 Apr;139(4):710-5. PMID: 10740156.
- Yilmaz M, Erol MK, Acikel M, Sevimli S, Alp N. Pulsed Doppler tissue imaging can help to identify patients with right ventricular infarction. Heart & Vessels. 2003 Jul;18(3):112-6. PMID: 12955425.