Giant Pilomatricoma of the Scalp: A Case Report
Chakiri R1*, Gallouj S1, Mernissi FZ1, Rimani M2
1 Department of Dermatology, University Hospital Hassan II de Fez, Morocco.
2 Center of Anatomopathology, Hassan, Rabat, Morocco.
*Corresponding Author
Radia Chakiri
Department of Dermatology, University Hospital Hassan II de Fez, Morocco.
E-mail: r.chakiri.87@gmail.com
Received: April 21, 2017; Accepted : May 22, 2017; Published: June 30, 2017
Citation: Chakiri R, Gallouj S, Mernissi FZ, Rimani M (2017) Giant Pilomatricoma of the Scalp: A Case Report. Int J Clin Dermatol Res. 5(5), 144-146.doi: dx.doi.org/10.19070/2332-2977-1700032
Copyright: Chakiri R© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Pilomatricoma is a benign cutaneous tumor originating from hair follicle matrix cells and characterized by the presence of subcutaneous nodules of up to 3.0 cm in diameter, usually on the head, neck and upper extremities. It is most common in the first two decades of life and after the age of 60.
We report a case of an adult female patient was evaluated, presenting a solid tumoral lesion, with approximately 3.5 x 3.0 cm in size, in the scalp. It was thought to be a squamous cell carcinoma, sarcoma, amelanotic melanoma, or nodular basal cell carcinoma.
The resection of the lesion was carried out and, at the histological examination, specific details were observed that led to the diagnosis of pilomatricoma.
Pilomatricoma should be suspected in the differential diagnosis of other cutaneous tumors.
2.Introduction
3.Case Report
4.Discussion
5.Conclusion
6.References
Keywords
Pilomatricoma; Tumor; Skin.
Introduction
The Pilomatricoma, previously calcified epithelioma of Malherbe, first described by Malherbe and Chenantais in 1880, is a benign appendageal tumor derived from hair follicle matrix cells. The Pilomatricoma occurs during the first two decades of life and is usually localized to the upper body. In its typical form, it translates clinically by a small subcutaneous nodule, solitary, sometimes with painful symptoms. The usual size is less than 3 cm. However, some cases of giant pilomatricoma have been reported. We present
a case of giant pilomatricoma on the scalp.
Case Report
We report the case of a 60 year old woman with no medical history, who consults for a tumor of the scalp, increasing progressively by size and becoming bloody in the contact.
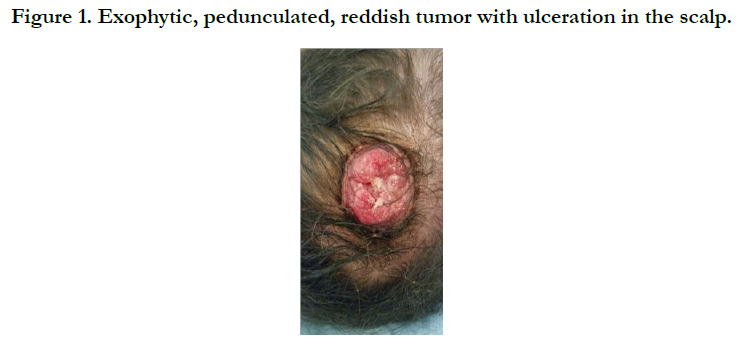
The physical examination revealed a solid tumoral lesion of about 3 x 3.5 cm in size in the scalp, adhered to deep planes, painful on palpation and ulcerated in the center [Figure 1].
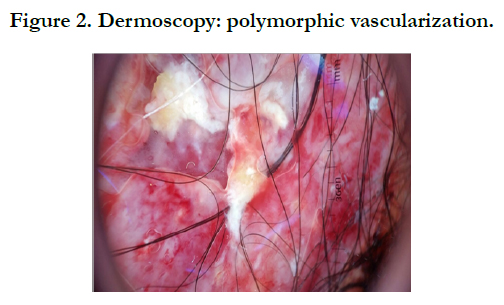
The dermoscopic examination had objectified polymorphic vascularization. It was thought to be sarcoma, amelanotic melanome, spinocellular carcinoma, lymphoma or nodular basal cell carcinoma [Figure 2].
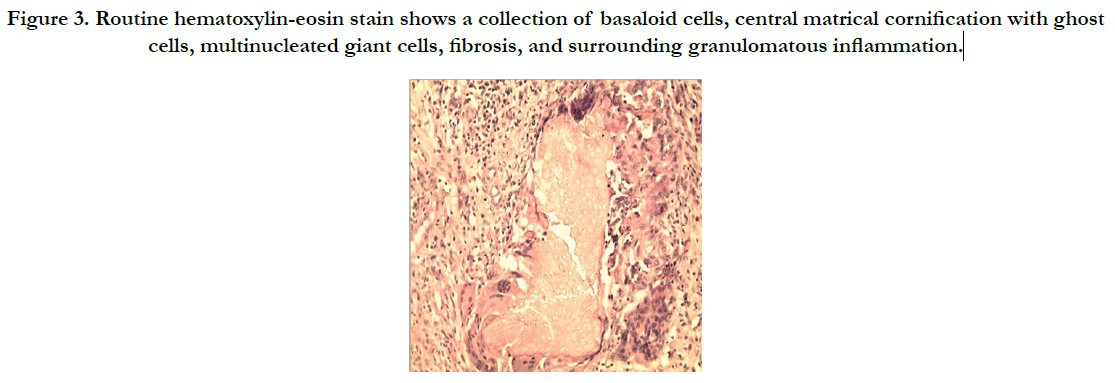
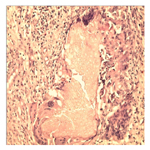
Histopathologic examination revealed a well-circumscribed tumor involving the whole dermis and the subcutis and composed of partially confluent aggregates of matrical cells admixed with eosinophilic cornified material containing shadow cells. In addition, multinucleated giant cells, areas of calcification. On the basis of histopathologic features, the diagnosis of pilomatricoma was made [Figure 3].
Figure 3. Routine hematoxylin-eosin stain shows a collection of basaloid cells, central matrical cornification with ghost cells, multinucleated giant cells, fibrosis, and surrounding granulomatous inflammation.
The patient underwent resection of the lesion with safety margins of 1.0 cm with good evolution without recurrence after 1 year.
Discussion
Pilomatricoma which is also known as Malharbe’s calcified epithelioma currently was mentioned in 1861 in Wilcken’s doctoral thesis and Malharbe and Chenantais defined the lesion as calcified epithelioma in 1880 [1-3], It is a benign appendageal tumor derived from hair follicle matrix cells [4].
It is a slow-growing, firm, dermal or subcutaneous neoplasm, usually measuring fewer than 3 cm in diameter. Pilomatricomas are considered benign and rarely recur after surgical excision [5, 6]. However, cases of CEM with a tendency for focal invasiveness and local recurrence have been reported and designated firstly as aggressive pilomatricomas [7-9].
Less common morphologic variants include perforating, lymphagiectatic, keratoacanthoma-like, pigmented, and anetoderma-like surface changes [4, 10]. Inflammation and erosion through the skin surface are observed in the rare perforating variant, as seen in our patient.
The tumors predominantly occur on the head, neck, and upper extremities, with only 9.5% on the scalp as in our case. It may occur at any age, though it has a bimodal distribution with peaks in childhood and in adults older than 60 years. A slight preponderance in females has been observed with a female to male ratio of 1.5 to 1 [4].
Recent investigations have shown that recurrent mutations in the beta-catenin gene are responsible [1, 11]. It has been reported to be related with myotronic dystrophy gene, polyoma virus, Gardner syndrome, xeroderma pigmentosum, Turner syndrome, sarcoidosis and basal cell nevus syndrome [1, 11,12]. No sign which might be related with these conditions was found in our patients. Because pilomatricomas may resemble other skin tumors such as epidermoid cysts, dermatofibrosarcoma protuberans, calcinosis cutis, cutaneous metastases, calcified hemangioma, giant dermatofibroma or nodular basal cell carcinoma, histopathological examination is crucial for definitive diagnosis [13, 14].
The histopathology of pilomatricoma shows a well-circumscribed, deep dermal or dermal subcutaneous tumor formed by basaloid cells that gradually lose their nuclei and mingle with the eosinophilic shadow cells that show ghosts of epithelial cells. Calcification may be seen in shadow cell regions along with foreign body giant cell reaction to keratin [15]. Malignant transformation with cell necrosis and mitotic figures have been documented in pilomatricoma [14]. In this case pilomatrical carcinoma was excluded because of absence of high mitotic activity and nuclear atypia.
Transformation into malignancy, known as pilomatrical carcinoma, is rare. These malignant neoplasms are characterized by aggressive biologic behavior such as recurrence, diffuse spread, or metastasis, or by cytologic abnormalities such as poor cellular organization, squamous differentiation, and conspicuous mitotic activity [16]. The recent growth of the long-standing lesion in our patient might be interpreted as a sign of malignant transformation.
Pilomatricomas are not associated with mortality. Pilomatrical carcinomas are uncommon but are locally invasive and can cause visceral metastases and death. Spontaneous regression has never been observed and medical treatment is ineffective. The treatment of choice is incision and curettage or surgical excision [17]. Although recurrence has only been reported in 2.6% of cases from a large case series (N=228), patients sokhould be monitored after surgical excision [4].
Conclusion
Our patient’s tumor was relatively atypical for PM, because it occurred on the scalp of a 60-year old female, grew rapidly, presented with ulceration, and had a diameter of 3.5cm. In addition, the clinical diagnoses were wrong.
Although pilomatricoma is a commonly seen tumor, there are no clinical criteria for diagnosis. Since it may be confused with other tumors of the skin such as sarcomas and cutaneous metastases, histopathological examination is critical.
References
- Nevzat Dabak, Alper Çıraklı, Bedri Kandemir, Sevgi Çıraklı, Sabit Numan Kuyubaşı (2014) Pilomatrixoma localized in the arm and forearm. Türk Ped Ar. 49(4): 340-3.
- Jallouli M, Yengui H, Khabir A, Mhiri R (2009) Pilomatrixoma of earlobe. J Cutan Aesthet Surg. 2(1): 36-7.
- Malherbe A, Chenantais J (1880) Note sure l’epithelioma calci¬fie des glandes sebacees prog. Med. 8: 826-8.
- Imadojemu S, Pugliese DJ, Kovarik CL (2014) Solitary nodular lesion on the scalp. Cutis. 93(3): E1-3.
- Kaddu S, Kerl H (2003) Appendage tumors of the skin. Fitzpatrick’s Dermatology in General Medicine. (6th edn), New York, NY: McGraw-Hill Co, 785-808.
- Hernández-Núñez A, Nájera Botello L, Romero Maté A, Martínez-Sánchez C, Utrera Busquets M, et al., (2014) Retrospective study of pilomatricoma : 261 tumors in 239 patients . Actas Dermosifiliogr. 105(7): 699-705.
- Kondo RN, Pontello Junior R, Belinetti FM, Cilião C, Vasconcellos VR, et al., (2015) Proliferating pilomatricoma - Case report. An Bras Dermatol. 90(3): 94-96.
- Satoh M, Ookouchi M, Yamamoto T (2012) Photoletter to the editor: Proliferating pilomatricoma with no recurrence during a 3-year follow-up. J Dermatol Case Rep. 6: 127-9.
- Sakai A, Maruyama Y, Hayashi A (2008) Proliferating pilomatricoma: a subset of pilomatricoma. J Plast Reconstr Aesthet Surg. 61(7): 811-4.
- Julian CG, Bowers PW (1998) A clinical review of 209 pilomatri¬comas. J Am Acad Dermatol. 39(2): 191-195.
- Kumar S (2008) Rapidly growing pilomatrixoma on eyebrow. Indian J Ophthalmol. 56(1): 83-4.
- Yamauchi M, Yotsuyanagi T, Saito T, Ikeda K, Hiquma Y, et al., (2010) Three cases of giant pilomatrixoma-considerations for diagnosis and treatment of giant skin tumours with abundantınner calcification present on the upper body. J Plast Reconstr Aesthet Surg. 63(6): 519-24.
- Topal IO, Singer R, Kocaturk Goncu OE, Topal Y, Yarıkkaya E, et al., (2015) An ulcerated giant pilomatricoma mimicking malignancy. J Dtsch Dermatol Ges. 13(4): 329-30.
- Turhan-Haktanir N, Demir Y, Sahin O, Bukulmez A, Tuzuner M (2009) Pilomatricoma: a review of six pediatric cases with nine lesions. Turk J Pediatr. 51(1): 44–8.
- Nadershah M, Alshadwi A, Salama A (2012) Recurrent giant piloma¬trixoma of the face: a case report and review of the literature. Case Rep Dent. 2012: 197–273.
- Wood MG, Parhizgar B, Beerman H (1984) Malignant pilomatri¬coma. Arch Dermatol. 120(6): 770-773.
- Thomas RW, Perkins JA, Ruegemer JL, Munaretto JA (1997) Surgical exci¬sion of pilomatrixoma of the head and neck: a retrospec¬tive review of 26 cases. Ear Nose Throat J. 78(8): 541, 544-546, 548.