Retrospective Assessment Of Postoperative Pain Control With Intravenous Or Epidural Patient-Controlled Analgesia After Orthopedic, General And Plastic Surgery
Çakir E1, Doğan G2*, Akdur F1, Kılıç I1, Örnek D1, Gökçinar D1, Göğüş N1
1 Ankara Numune training and research hospital, anesthesiology and reanimation clinic, Ankara, Turkey.
2 Hitit University Corum education and research hospital anesthesiology and reanimation clinic, Çorum, Turkey.
*Corresponding Author
Güvenç Dogan,
Hitit University Corum education and research hospital anesthesiology and reanimation clinic, Çorum, 19000, Turkey.
Tel: 05324025208
E-mail: guvencdogan@gmail.com
Received: February 02, 2017; Accepted: February 16, 2017; Published: February 18, 2017
Citation: Çakir E, Doğan G, Akdur F, Kılıç I, Örnek D, et al., (2017) Retrospective Assessment Of Postoperative Pain Control With Intravenous Or Epidural Patient-Controlled Analgesia After Orthopedic, General And Plastic Surgery. Int J Anesth Res. 5(2), 401-408. doi: http://dx.doi.org/10.19070/2332-2780-1700083
Copyright: Doğan G© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Aim: Patient-controlled analgesia methods are more effective than conventional analgesia methods for the management of postoperative pain. Patient-controlled analgesia is often preferred as it has less sedative effect, minimum complications, high patient satisfaction and has positive effects on the healing process of patients. The aim of this study was to research patientcontrolled analgesia methods that were used for postoperative pain control in a training and research hospital.
Material And Methods: Retrospectively we reviewed the records of patients who were ASA physical status I-II-III, older than 18 years and underwent procedures for orthopedic surgery, general surgery, neurosurgery, ear, nose and throat surgery, chest surgery, urology, hand surgery or plastic surgery in Numune Training and Research Hospital.
Results: A total of 449 patients were administered patient-controlled analgesia in Numune Training and Research Hospital. 67% of patients were administered patient controlled analgesia via epidural vs. 33% of patients administered patient controlled analgesia via intravenous route. Patients' age gender, ASA class, primary disease requiring surgery, method of surgery, duration of surgery, anesthetic technique, drugs used for postoperative analgesia, the amount of analgesic drug consumption, the time to administration of analgesic drug, VAS scores at bolus time, the postoperative analgesic consumption in the first 24 hours blood pressure, heart rate, respiratory rate, side effects, and patient satisfaction level were evaluated.
Conclusions: As a result of the study on 449 patients administered patient-controlled analgesia in Numune Training and Research Hospital between April 2011 and December 2011, the administration of patient controlled analgesia via epidural was preferred over than the administration of patient controlled analgesia via intravenous route.
2.Material and Method
3.Statistical Analysis
4.Results
5.Discussion
6.References
Introduction
Currently, though effective postoperative pain control is an important part of postoperative care, nearly 30-80 % of patients complain of moderate-severe degrees of pain [1, 2]. The result of insufficient postoperative pain control activates the sympaticoneural and neuroendocrine systems, and causes harmful effects like tachycardia, hypertension, hyperglycemia, immunosuppression and reduced regional blood perfusion [2]. Delays in improving this situation may cause lengthened hospital stays and increased medical costs [3].
Patient-controlled analgesia (PCA) administration for postoperative pain treatment is more efficient than conventional analgesia methods (intra muscular (IM), IV, oral administration, on demand) and is commonly chosen today due to higher rates of patient satisfaction, less sedation, less postoperative complications and positive contribution to patient recovery durations [4, 5]. PCA methods may be defined as methods that allow patients to decide for themselves when and how much analgesic to use. In a sense, patients are responsible for their own pain control. PCA methods may use a programmed infusion pump if required by the patient, with previously programmed dose limits and lock duration with bolus injections which are activated by using a button linked to the pump so patients administer their own analgesic medications [6, 7]. The most commonly used method with PCA is IV PCA. Additionally, in the literature there are many alternative administration methods defined. Among these are PCA administrations through catheters inserted in the epidural region or peripheral nerves. Again less common are subcutaneous, IM, rectal and oral PCA administrations [8]. In recent years, non-invasive PCA modalities like transdermal PCA methods have been developed [9].
In Turkey, there are insufficient studies on which operations are followed by PCA use for postoperative analgesia in Training and Research Hospitals and content of PCA protocols encountered in the literature. The aim of this study is to investigate PCA methods used for postoperative pain control in the 1150-bed Ankara Numune Training and Research Hospital.
Material and Method
This study retrospectively investigated the anesthesia records of Ankara Numune Training and Research Hospital. The PCA (patient- controlled analgesia) records of a total of 449 patients above the age of 18 in ASA groups I-II-III who underwent orthopedic, general, neurosurgery, ear, nose and throat, chest, urology, hand or plastic surgery operations were investigated.
The age, gender, ASA class, primary disease requiring surgery, surgery type and duration, anesthesia method, medication used for postoperative analgesia, amount of medication consumed, time administered, bolus VAS values, additional analgesia requirements in the postoperative first 24 hours, blood pressure, heart rate, respiratory rate, side effects and patient satisfaction were recorded.
There are two separate applications of postoperative PCA in the Anesthesiology and Reanimation clinic at Ankara Numune Training and Research Hospital:
1. Intravenous PCA (HOSPIRA/MEDITERA Pain Management Provider): Prepared with 300 ml tramadol (Contramal ampule, Abdi İbrahim, İlaç AŞ, İstanbul, Turkey) within 150 ml physiologic serum. After administering a 3 ml loading dose, the PCA device is set to hourly infusion rate of 3 ml/ hour with PCA bolus dose of 3 ml and lock duration of 20 min.
2. Epidural PCA (HOSPIRA/MEDITERA Pain Management Provider): Prepared with 150 mg chirocaine (Chirocaine® 50 mg/10 ml polypropylene levobupivacaine Ampule ABBOTT Laboratories) and 350 mcg fentanyl (Fentanyl-Janssen, Janssen- Cilag İlaç AŞ, Belgium) within 150 ml physiologic serum. After 3 ml loading dose is administered, the hourly infusion rate of the PCA device is set to 3 ml/hour with PCA bolus dose of 3 ml and lock duration of 20 minutes.
In our clinic, postoperative pain treatment begins in the intraoperative period. With this aim, IV NSAID, IV paracetemol and IV tramadol are used alone or in combination. The patient’s pain complaints are assessed with a verbal descriptor scale (VSD) in the Post Anesthesia Care Unit (PACU). This scale divides pain into 4 categories from severe to mild (severe, moderate, mild and none) [10]. For patients with severe and moderate pain complaints, the anesthesia expert from the operation room is consulted and taking account of the patient’s clinical tableau and previously administered analgesics, additional analgesia (IV NSAID, IV paracetemol and IV tramadol) is administered.
To reduce postoperative nausea-vomiting complaints in our clinic, patients begin antiemetic treatment in the intraoperative period and this continues during treatment of patients with IV PCA method for postoperative pain treatment. For antiemetic treatment primarily metaclopramide HCl is used, with ondansetron preparations used for cases resistant to treatment. The dose and administration frequency of antiemetic treatment is determined by taking account of the patient’s complaints.
All patients administered PCA methods are recorded in the PCA notebook in the Pain Unit and visited by the anesthesia technician on duty at least twice a day. During these visits, side effects (nausea-vomiting, sedation, motor block in epidural PCA patients, hypotension, urine retention) and analgesic sufficiency is assessed and reported to the doctor on duty in the Pain Unit and appropriate treatment arranged. In the wards, the patient’s pain is assessed with the visual analog scale (VAS) (1-10) different to the VSD used in the PACU and patients with VAS ≥ 4 in spite of PCA analgesia method are administered additional analgesia.
Statistical Analysis
Data analysis was completed in SPSS 15 for Windows program. Descriptive statistics for variables with normal distribution are given as mean ± standard deviation, as median (min-max) for variables with non-normal distribution, and categorical variables are given as case number and %. Significance of differences between groups of categorical variables was assessed with the chi-square test. Results with p<0.05 were accepted as statistically significant.
Results
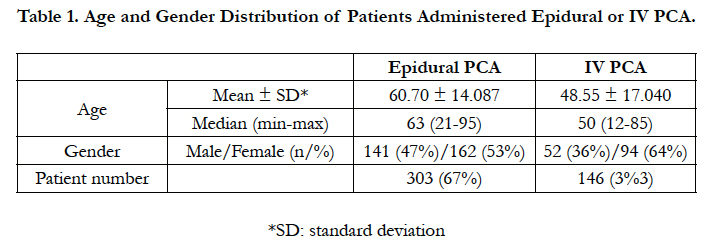
Within the 9 month duration, a total of 449 patients were identified to have received postoperative PCA treatment. Epidural PCA was administered to 303 (67%) patients with IV PCA administered to 146 (33%) patients (Table 1).
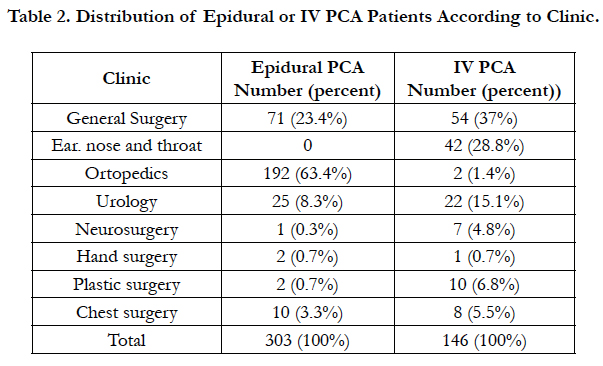
Of the total of 194 patients in the orthopedic clinic, 192 (63.4% of total) had epidural PCA method administered and in the other surgical clinics, the epidural PCA method was chosen at proportionally higher rates (Table 2).
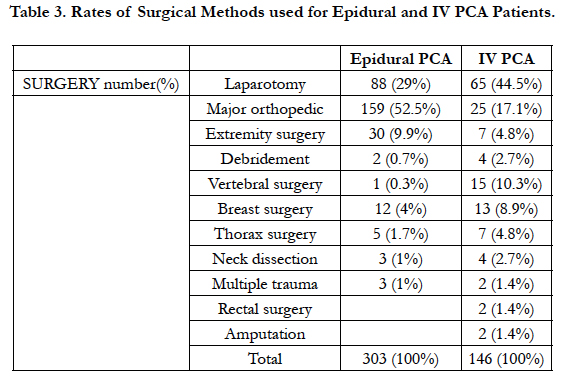
When the chosen PCA method is assessed in terms of surgical method used, major orthopedic surgery interventions by the orthopedic clinic had higher rates of epidural PCA use compared to other surgical operations (Table 3).
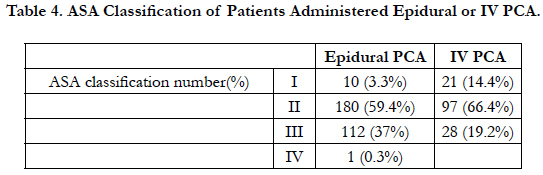
When the ASA classification of epidural and IV PCA patients is investigated, there was a high rate of patients in ASA II operated on. Again it was determined that the patient population administered epidural PCA comprised the ASA II patient group (Table 4).
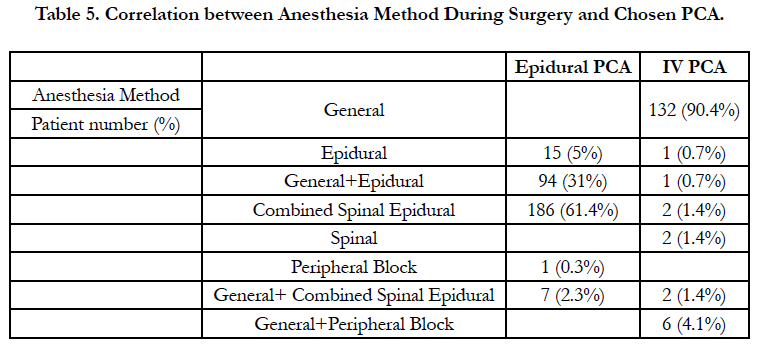
When the anesthesia method used during surgery and chosen PCA method are investigated, all patients with general anesthesia administered were given the IV PCA method. Of patients given regional anesthesia with the epidural method, 0.7% again had IV PCA method chosen (Table 5).
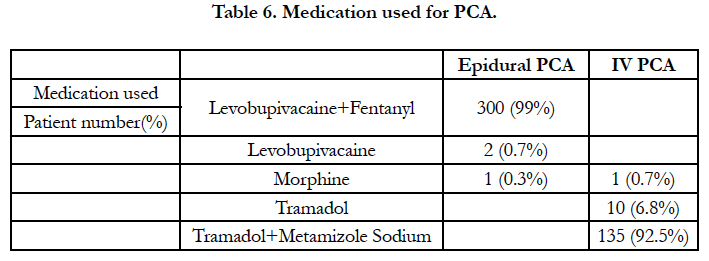
When the distribution of levobupivacaine+fentanyl, only levobupivacaine or only morphine administration for epidural PCA patients are investigated, patients administered levobupivacaine + fentanyl comprised 99% of patients administered epidural PCA method (Table 6).
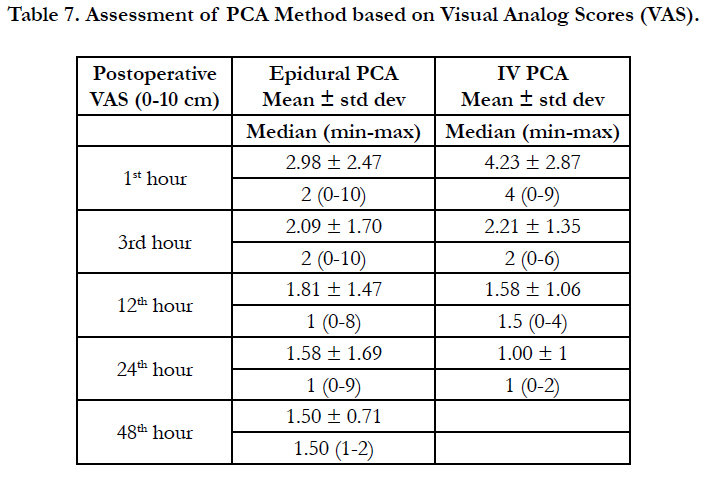
The 10 cm visual pain scale (visual analog score-VAS) in the first hour was 2.98 ± 2.47 (mean ± standard deviation) for epidural PCA patients and 4.23 ± 2.87 for IV PCA patients. In the 3rd hour, it was 2.09 ± 1.70 for epidural PCA patients and 2.21 ± 1.35 for IV PCA patients. By the 12th hour, VAS was 1.81 ± 1.47 for epidural PCA patients and 1.58 ± 1.06 for IV PCA patients (Table 7).
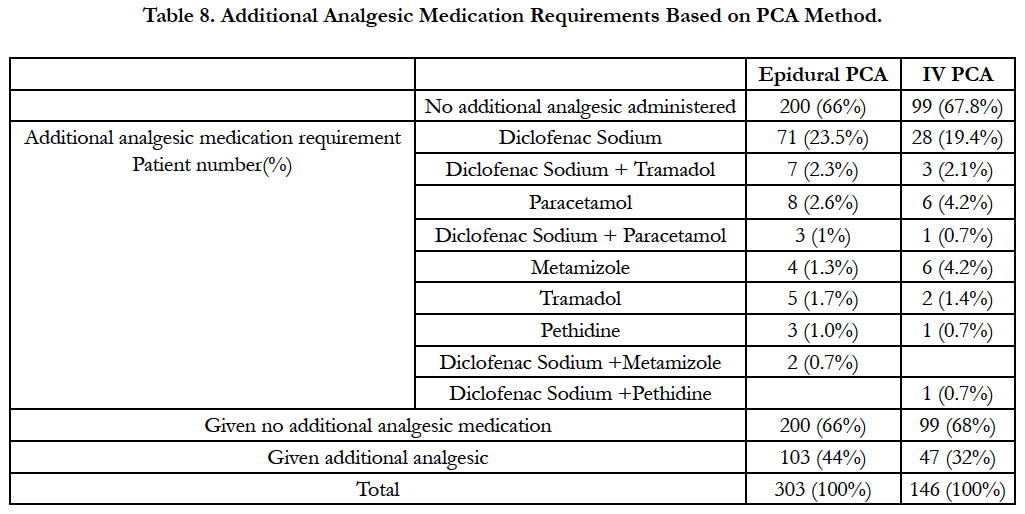
While 103 (44%) patients administered epidural PCA required additional medication within the first 24 hours, 47 (32%) patients administered IV PCA required additional analgesia in the first 24 hours (Table 8).
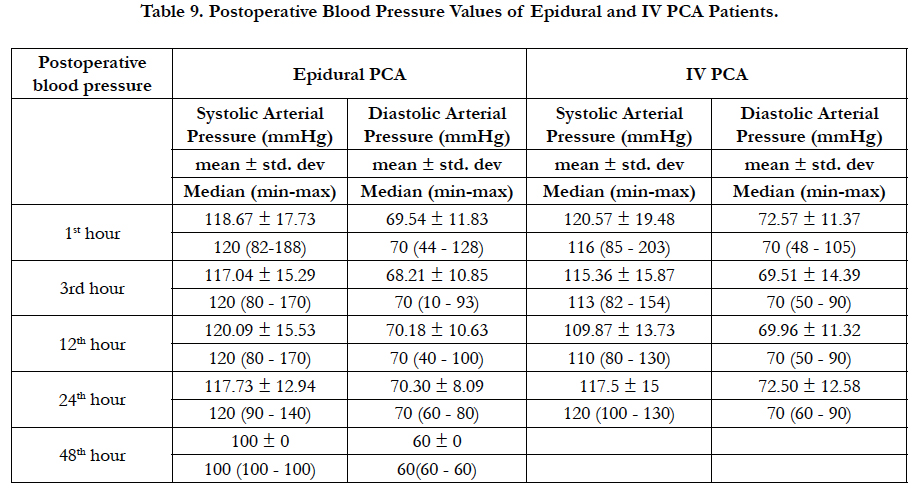
When blood pressure is evaluated, in the 1st hour patients given epidural PCA had systolic arterial pressure of 118.67 ± 17.73, while IV PCA patients had systolic arterial pressure of 120.57 ± 19.48. In the 1st hour, epidural PCA patients had diastolic arterial pressure of 69.54 ± 11.83 while IV PCA patients had diastolic arterial pressure of 72.57 ± 11.37 (Table 9).
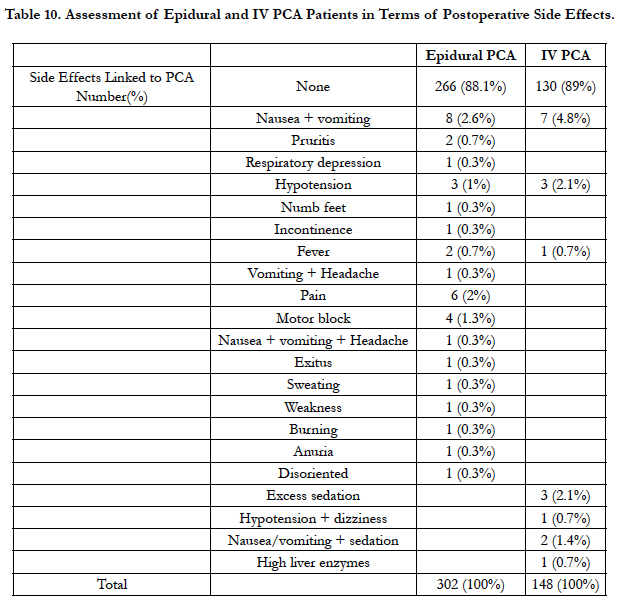
When side effects are investigated in terms of PCA method, while 266 (88.1%) epidural PCA patients had no side effects, 130 (89%) IV PCA patients had no side effects. There were 2 (0.7%) epidural PCA patients with pruritis observed with no IV PCA patients observed to have pruritis (Table 10).
In the postoperative period when the satisfaction rates of patients with PCA are assessed, 68.3% of epidural PCA patients were satisfied with the analgesia method, while 15.1% of IV PCA patients were satisfied with their analgesia method.
While 67% of patients had epidural PCA administered, 33% had IV PCA used. The age, gender, ASA class, primary disease for surgery, surgery type and duration, anesthesia method, medication used for postoperative analgesia, amount of medication consumed, time of administration, bolus VAS values, additional analgesia requirement in the postoperative 24 hours, blood pressure, heart rate, respiratory rate, side effects and patient satisfaction were evaluated. It was determined that epidural PCA was more commonly used and in spite of some side effects (nauseavomiting, pruritis, etc.) of the epidural and IV PCA protocols administered for postoperative analgesia, we believe it is a reliable, effective method increasing satisfaction.
Discussion
A total of 449 patients were administered postoperative PCA treatment. While 67% of patients were given epidural PCA, 33% were given IV PCA.
The superiority of IV PCA and epidural PCA administration for postoperative pain treatment compared to conventional requested analgesia administration is indisputable. Additionally, the effects of both PCA methods on surgical morbidity, patient quality of life, recovery quality and patient satisfaction are still being researched today. When studies comparing epidural analgesia with systemic analgesia in different surgical interventions are investigated, it appears there is still insufficient data to make a judgment on which of the two methods is superior. Additionally, epidural analgesia is stated to ensure superior analgesia for all surgery types both at rest and when mobile compared to systemic opioid use with IV PCA [10-13].
In light of this knowledge, though globally IV PCA is a commonly used postoperative analgesia administration, it appears epidural PCA administration is superior in terms of analgesia quality. As the epidural catheterization which is the basis of epidural PCA administration is a more invasive procedure it requires a more experienced administrator, and though complications and side effects are rare it may lead to life-threatening results leading to debates on its superiority [10, 11].
In our study we found that at our hospital the number of epidural PCA administrations in the Pain Unit was greater than the number of IV PCA administrations. This situation does not comply with the information that in the majority of developing countries IV PCA is routinely used [4]. Currently systemic opioid use is very common with IV PCA administration. Though the commonly chosen medication is morphine, morphine use with PCA requires that patients be monitored for 8 to 24 hours in the postoperative period for respiratory depression [13]. As surgical clinics cannot abide by this condition in our hospital, instead of classic opioids the atypical opioid of tramadol, which causes less respiratory depression, is chosen for IV PCA administration in our clinic.
Previous studies have proposed that PCA increases patient satisfaction and reduces postoperative analgesic requirements [14-16]. Combined spinal epidural anesthesia (CSEA) has advantages such as short onset of effect, and the ability to lengthen the anesthesia duration [17]. In our study of the Anesthesiology clinic of Ankara Numune Training and Research Hospital, for analgesia administration with postoperative PCA levobupivacaine was chosen most for the epidural route, with tramadol chosen for the intravenous route. While the total levobupivacaine consumption per patient with epidural PCA was 156.40 ± 106.26 mg, the total tramadol consumption by IV PCA patients was identified as 2688.70 ± 791.35 mg. The median (min-max) consumption of levobupivacaine by epidural PCA patients was 150.30 (150-2000), while the same tramadol consumption by IV PCA patients was 2500 (50-3300). The 10 cm visual pain score (visual analog scale VAS) in the 1st hour was 2.98 ± 2.47 (mean ± standard deviation) for epidural PCA patients, while it was 4.23 ± 2.87 for IV PCA patients. For epidural PCA patients, the VAS scores in the 3rd, 12th, and 24th hours were 2.09 ± 1.70, 1.81 ± 1.47 and 1.58 ± 1.69, respectively. For IV PCA patients, the VAS scores in the 3rd, 12th and 24th hours were 2.21 ± 1.35, 1.58 ± 1.06 and 1.00 ± 1.00, respectively. In our study 103 (44%) patients administered epidural PCA required additional medication in the first 24 hours, while 47 (32%) IV PCA patients required additional analgesics in the first 24 hours.
Though tramadol used with the IV PCA method provides successful postoperative pain control, nausea and vomiting are commonly observed [18]. Additionally, the use of local anesthetics and opioids with the epidural PCA method provides better analgesia with lower opioid dose and less opioid side effects are reported compared with tramadol IV PCA administration [14 - 16, 19]. In our study, when the administered PCA method is assessed in terms of side effects, 266 (88.1%) patients administered epidural PCA had no side effects observed, while 130 (89%) IV PCA patients had no side effects identified. The number of epidural PCA patients with nausea + vomiting was 8 (2.6%), while 7 (4.8%) IV PCA patients had nausea + vomiting. Complications such as pruritis, respiratory depression, hypotension, numb feet, incontinence, fever, headache, sweating, weakness, continuation of motor block, discomfort and pain from urinary catheter, anuria, disorientation and cardiac arrest were observed more rarely in the postoperative period.
In our study there were 2 (0.7%) epidural PCA patients with pruritis observed, while no IV PCA patient had pruritis. The lifethreatening respiratory depression linked to medications used during PCA administration has a special importance within the list of side effects and complications [11]. The fact that no case developed respiratory depression leads to the opinion that our protocols are reliable. Operations with PCA used most commonly in our hospital were identified as knee and hip prosthesis, cesarean, lower extremity trauma surgery, pain-free birth, GIS surgery, multiple trauma surgery, thoracotomy, hysterectomy, laminectomy and urogenital surgery. In light of this knowledge, patients in the orthopedic, gynecology and obstetrics and general surgery clinics had PCA treatment applied more often compared to other clinics. We believe that basic determinants of the differences in PCA administration between clinics are the surgical procedure undergone and the expectation that postoperative pain severity will be high and last longer. We found that PCA administration was not chosen for operations under the other heading (shoulder surgery, extremity amputation, etc.). We believe the reason for this is that pain relief with peripheral nerve blockage techniques and single-dose epidural analgesia, not included in the study, may be chosen. The study did not separately research and discuss operations followed by PCA administration because we believe that it is appropriate for the anesthesiologist to plan the treatment method and protocol based on the patient and conditions and that it is necessary for choices to be made in this way. However, we can say that epidural PCA administration was mainly chosen in the orthopedic, gynecology and obstetrics and plastic reconstructive and esthetic surgery clinics. Nausea-vomiting requiring an end to postoperative PCA administration was first place among all side effects and complications with a rate of 42%. Additionally, other side effects and complications identified were pruritis, numbness, urine retention, constipation, confusion and hemorrhage. In conclusion, we believe that the epidural and IV PCA protocols applied for postoperative analgesia by our clinic are reliable and effective [20, 21] methods in spite of some side effects.
It is proposed that sufficient postoperative pain control is an important determining factor of patient satisfaction. There are results in the literature indicating a correlation between patient satisfaction and pain levels [22, 23]. Kouki et al., surveyed 345 patients (125 male and 220 female) who underwent elective surgery in a three month period. Of these patients, 237 had surgical procedures that create moderate and high levels of severe pain (major orthopedic and gynecological operations, laparotomies and intestinal surgery), and 176 of these patients had general anesthesia ± epidural while 61 had only regional anesthesia administered. Of patients administered anesthesia ± epidural 77 (44%) had IV PCA, 48 (27%) had epidural bolus at intervals and 51 (29%) had epidural PCA. This study by Kouki et al. found that when patients given PCA are generally examined, they had high satisfaction scores. Ninety six percent of patients given general anesthesia with epidural PCA or IV PCA stated that if they required an operation in the future they would want to administer the same pain treatment technique and 31% of these patients defined their pain treatment as “good” with 65% defining it as “perfect” [22]. A study by Gottschalk et al., of 150 adult patients identified that 95 underwent general surgery, 32 orthopedic surgery and 23 gynecology surgery. All patients were given 0.2% ropivacaine + 0.5 mcg/ ml sufentanil with epidural PCA pump with basal rate 6-8 ml/ hour, bolus of 2 ml and lock time of 5 minutes. The satisfaction of 88% of patients was “good” and “very good” when assessed by the postoperative pain service. Of patients 89% reported they would choose the same treatment again. This study by Gottschalk et al., proposed that there was no correlation between postoperative epidural pain treatment and patient satisfaction and that side effects and some problems occurring during pain treatment may ensure motivation in postoperative pain care [23]. Similarly in our study, high satisfaction rates were found for patients administered epidural or IV PCA.
In our study, 162 (53%) patients administered epidural PCA were female while 141 (47%) were male. The knowledge that women define and describe pain better than men may be explained by their earlier introduction to pain due to varying physiological reasons (menstruation, birth, etc.), learning coping techniques for pain earlier and tendency to accept pain treatment methods offered to them [24-26]. Additionally due to the higher number of women they may be better able to clearly describe their pain and have more positive expectations of preoperative pain [26, 27].
Insufficient postoperative analgesia may be linked to variations in analgesic medication requirements, variations in serum medication levels and delays in administering medication. Traditional analgesic regimes may be insufficient to compensate for these factors. IV PCA makes administration of opioids optimal and minimizes the effects of pharmacokinetic and pharmacodynamic variations due to personal differences in patients. IV PCA allows the administration of analgesic medication when in pain, and as pain reduces more medication is not required. If excess medication is given unnecessarily it may cause excess sedation or respiratory depression [21]. While insufficient dose with IV PCA may cause insufficient analgesia, when excessive doses are requested the incidence of unwanted side effects like respiratory depression increases [28].
The majority of IV PCA devices provide continuous infusion in addition to the PCA requested dose. In situations with continuous infusion in routine use, continuous analgesia is provided. The use of continuous infusion increases the total analgesic consumption and the incidence of side effects like respiratory depression [29]. When IV PCA is compared with traditional analgesic regimes, though IV PCA is shown to provide superior postoperative analgesia and increase patient satisfaction, there is insufficient data on whether IV PCA provides any economic benefit [5]. A meta-analysis (including 55 studies and 2023 patients) found that IV PCA provided better analgesia and better patient satisfaction compared to traditional methods, but that the IV PCA group consumed more opioids and had greater incidence of pruritis [5]. Though there is no evidence that IV PCA use reduces hospital stays, it reduces nursing time compared to intramuscular injections and thus it is reported that less capable personnel can work in surgical and internal medicine clinics [30].
When the results of correlations of IV PCA with patient satisfaction are assessed, it provides important advantages, with patients more likely to choose IV PCA compared to other traditional methods of analgesic administration (intravenous, intramuscular or subcutaneous). IV PCA provides patient satisfaction with analgesia at the highest level and ensures patient control without requesting analgesics from nurses [32].
Compared with opioid administration with traditional methods (intravenous, intramuscular or subcutaneous), there is no difference in the incidence of unwanted effects due to opioids administered with IV PCA. The rates of respiratory depression related to IV PCA are low (<0.5%) and are not greater when compared with traditional methods or neuraxial opioids [33]. The factors related to respiratory depression with IV PCA are reported to include continuous infusion, advanced age, administration with sedative or hypnotic agents and accompanying pulmonary disease (like sleep apnea) [29, 33].
Tramadol is a synthetic opioid with weak μ-agonist activity and is a re-uptake inhibitor of serotonin and norepinephrine. Though the analgesic effect of tramadol is mainly through central mechanisms, it has peripheral local anesthetic properties [34]. Tramadol is effective to resolve moderate levels of postoperative pain and the analgesic efficacy is equivalent to 650 mg aspirin + 60 mg codeine or 400 mg ibuprofen [35]. The advantages of tramadol for postoperative analgesia is that it does not cause respiratory depression, major organ toxicity, does not reduce gastrointestinal motility and has less potential for abuse [36]. Side effects of tramadol (incidence 1.6-6.1%) are dizziness, numbness, sweating, nausea, vomiting, dry mouth and headache [35].
A variety of neuraxial and peripheral analgesic techniques can be used for effective treatment of postoperative pain. Generally analgesia with epidural techniques provides better results than systemic opioids [37]. The use of these techniques may reduce morbidity and mortality [38, 39]. However, there are risks involved in these techniques and the harm-benefit ratio should be assessed on an individual basis.
Analgesia administered by epidural catheter is a reliable and effective method for treatment of acute postoperative pain [40]. Postoperative epidural analgesia provides superior analgesia than systemic opioids [40, 41]. Compared with systemic opioids, combined epidural as a part of the general anesthetic technique with intraoperative epidural use ensures less pain and more rapid patient recovery in the period immediately after surgery [42]. In conclusion, this retrospective study of the anesthesiology and reanimation clinic at Ankara Numune Training and Research Hospital determined that epidural PCA was more commonly used and that in spite of some side effects (nausea-vomiting, pruritis, etc.) of epidural and IV PCA protocols used for postoperative analgesia, we believe they are reliable and effective methods that increase satisfaction.
References
- Apfelbaum JL, Chen C, Mehta SS, Gan TJ (2003) Postopera¬tive pain experience: results from a national survey suggest postoperative pain continues to be under¬managed. Anesth Analg. 97(2): 534–540.
- Wu CL, Raja SN (2011) Treatment of acute postoperative pain. Lancet. 377(9784): 2215-2225.
- Kehlet H, Holte K (2001) Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 87(1): 62–72.
- Liu SS, Wu CL (2007) The effect of analgesic technique on postoperative patient-reported outcomes includ¬ing analgesia: a systematic review. Anesth Analg. 105(3): 789–808.
- Hudcova J, McNicol E, Quah C, Lau J, Carr DB (2006) Patient controlled opioid analgesia versus conventional opioid analgesia for postoperative pain. Cochrane Database Syst Rev. 18(4): CD003348.
- Yücel A (1997) Patient Controlled An¬algesia. PCA, 1st (Edn), İstanbul: Turkey. 3.
- Viscusi ER (2008) Patient-controlled drug delivery for acute postoperative pain management: a review of current and emerging technologies. Reg Anesth Pain Med. 33(2): 146-158.
- Yucel A (1997) Alternative Pathways in PCA. Patient Controlled Analgesia PCA, 1st (Edn), Istanbul: Turkey. 82.
- Miaskowski C (2005) Patient-controlled modalities for acute postoperative pain management. J Perianesth Nurs. 20(4): 255-267.
- Herr KA, Spratt K, Mobily PR, Richardson G (2004) Pain intensity assessment in older adults: use of experi¬mental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clin J Pain. 20(4): 207-219.
- Yucel A (1998) Patient Controlled Analgesia (PCA). 2nd (Edn), Istanbul: Turkey. 31-3, 101-102.
- Pöpping DM, Zahn PK, Van Aken HK, Dasch B, Boche R, et al., (2005) Effectiveness and safety of postoperative pain management: a survey of 18 925 consecutive patients between 1998 and 2006 (2nd revision): a database analysis of prospectively raised data. Br J Anesth. 101(6): 832-840.
- Sam WJ, MacKey SC, Lötsch J, Drover DR (2011) Morphine and its metabolites after patient-controlled analge¬sia: considerations for respiratory depression. J Clin Anesth. 23(2): 102-106.
- Lebovits AH, Zenetos P, O’Neill DK, Cox D, Dubois MY, et al., (2001) Satisfaction with epidural and intravenous patientcontrolled analgesia. Pain Med. 2(4): 280-6.
- Thomas V, Heath M, Rose D, Flory P (1995) Psychological characteristics and the eff ectiveness of patient-controlled analgesia. Br J Anaesth. 74(3): 271-6.
- Baykara N, Karabey F, Özdamar D, Toker K (2003) Combined spinalepidural lower bottom performed by anesthesia method after operation tramadol or morphine epidural patient controlled analgesia. Cumhuriyet University. 25:111-6.
- Gültekin S (1998) Evaluation of two different techniques in combined spinal-epidural anesthesia. Anest Rean Cem Mecmuası. 26: 64-71.
- Pang WW, Mok MS, Lin CH, Yang TF, Huang MH (1999) Comparison of patient-controlled analgesia (PCA) with tramadol or morphine. Can J Anaesth. 46(11): 1030-5.
- Cousins MJ, Mather LE (1984) Intrathecal and epidural administration of opioids. Anesthesiology. 61(3): 276-310.
- Grass JA (2005) Patient-controlled analgesia. Anesth Analg. 101(5): S44-61.
- Macintyre PE (2001) Safety and effi cacy of patient-controlled analgesia. Br J Anaesth. 87(1): 36-46.
- Kouki P, Matsota P ,Christodoulaki K, Kompoti M, Loizou M, et al., (2012) Greek surgical patients’ satisfaction related to perioperative anesthetic services in an academic institute. Patient prefer adherence. 6: 6569-578.
- Gottschalk A, Freitag M, Liehr K, Domke A, Schuster M, et al., (2004) Does patient satisfaction correlate with pain level during patient-monitored epidural analgesia. Evaluation of data from postoperative pain service. Schmerz. 18(2): 145-50.
- Myles PS, Hunt JO, Moloney JT (1997) Postoperative ‘minor’ complications, comparison between men and women. 52(4): 300-6.
- Puntillo K, Weiss SJ (1994) Pain: its mediators and associated morbidity in critically ill cardiovascular surgical patients. Nurs Res. 43(1): 31-6.
- İşler D (2006) Effect of preoperative detailed information on postoperative analgesic requirement and patient satisfaction.[specialization thesis]. Ankara: turkey.
- Wilson-Burnett J (1979) Stress in hospital: Patients’ Psychological Reactions to Illness and Care. New York: Churchill Livingstone. 33-4.
- Camu F, Van Aken H, Bovill JG (1998) Postoperative analgesic effects of three demand-dose sizes of fentanyl administered by patient-controlled analgesia. Anesth Analg. 87(4): 890.
- Looi-Lyons LC, Chung FF, Chan VW, McQuestion M (1996) Respiratory depression: An adverse outcome during patient-controlled analgesia therapy. J Clin Anesth. 8(2): 151.
- Chan VW, Chung F, McQuestion M, Gomez M (1995) Impact of patientcontrolled analgesia on required nursing time and duration of postoperative recovery. Reg Anesth 20(6): 506-14.
- Thomas V, Heath M, Rose D, Flory P (1995) Psychological characteristics and the effectiveness of patient-controlled analgesia. Br J Anaesth. 74(3): 271-6.
- Pellino TA, Ward SE (1998) Perceived control mediates the relationship between pain severity and patient satisfaction. J Pain Symptom Manage. 15(2): 110-6.
- Etches RC (1994) Respiratory depression associated with patient-controlled analgesia: A review of eight cases. Can J Anaesth. 41(2): 125-32.
- Pang WW, Huang PY, Chang DP, Huang MH (1999) The peripheral analgesic effect of tramadol in reducing propofol injection: A comparison with lidocaine. Reg Anesth Pain Med. 24(3): 246.
- Edwards JE, McQuay HJ, Moore RA (2002) Combination analgesic efficacy: Individual patient data metaanalysis of single-dose oral tramadol plus acetaminophen in acute postoperative pain. J Pain Symptom Manage. 23(2): 121-30.
- Budd K, Langford R (1999) Tramadol revisited. Br J Anaesth. 82(4): 493-5.
- Dolin SJ, Cashman JN, Bland JM (2002) Effectiveness of acute postoperative pain management: I. Evidence from published data. Br J Anaesth. 89(3): 409-23.
- Liu S, Carpenter RL, Neal JM (1995) Epidural anesthesia and analgesia. Their role in postoperative outcome. Anesthesiology. 82(6): 1474-506.
- Wu CL, Fleisher LA (2000) Outcomes research in regional anesthesia and analgesia. Anesth Analg. 91(5): 1232.
- Wheatley RG, Schug SA, Watson D (2001) Safety and efficacy of postoperative epidural analgesia. Br J Anaesth. 87(1): 47-61.
- Wu CL, Cohen SR, Richman JM, Courpas GE, Lin EE, et al., (2005) Efficacy of postoperative patient-controlled and continuous infusion epidural analgesia versus intravenous patient-controlled analgesia with opioids: A metaanalysis. Anesthesiology. 103(5): 1079.
- Block BM, Liu SS, Rowlingson AJ, Cowan AR, Wu CL, et al., (2003) Efficacy of postoperative epidural analgesia: A meta-analysis. JAMA. 290(18): 2455.