Comparative Study of Isobaric Ropivacaine with and without Morphine in Spinal Anaesthesia for Perineal Surgeries
Dayananda V. P1*, Ramesh R1, Priyanka V2
1 Assistant Professor, Department of Anaesthesiology, BMC and RI, Bangalore, Karnataka, India.
2 Resident Department of Anaesthesia, B M C & R I, Banglore, India.
*Corresponding Author
Dr. Dayananda V. P.,
Assistant Professor,
Department of Anaesthesiology,
BMC and RI,
Bangalore, Karnataka, India.
E-mail: vpd921@yahoo.com
Received: January 05, 2016; Accepted: January 27, 2016; Published: February 01, 2016
Citation: Dayananda V. P, Ramesh R, Priyanka V (2016) Comparative Study if Isobaric Ropivacaine with and without Morphine in Spinal Anaesthesia for Perineal Surgeries. Int J Anesth Res. 4(2), 208-212.DOI : dx.doi.org/10.19070/2332-2780-1600048
Copyright: Dayananda V. P© 2016. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objectives: The comparative study is under taken to evaluate use of intrathecal isobaric ropivacaine with and without
adjuvant morphine in perineal surgeries.
Aims: The aim of this study is to evaluate sensory block, motor block and other clinical effects with 3 ml of isobaric 0.5%
ropivacaine along with 100μ morphine and without mophine intrathecally in Perineal surgeries.
Methods: This study was conducted in 100 patients scheduled for elective Perineal surgeries. The patients were grouped as
study and control group with 50 patients in each group. The study group received 3ml of 0.5% isobaric ropivacaine with
100μ morphine intrathecally and control group received only 3ml of 0.5% isobaric ropivacaine. Onset and duration of
sensory block, motor block, quality of anaesthesia, time of request for analgesia, time for ambulation, VAS score, hemodynamic
parameters and adverse effects if any were studied.
Results: In present study faster in onset of sensory block with normal duration sensory block was observed in study group. In addition short duration of motor block, with early ambulation was noted in study group. Requirement of rescue analgesia was prolonged with duration of 5.92 hrs in study group in comparison to control group which was 4.00 hrs and this was statically significant.
Conclusion: Intrathecal administration of Isobaric ropivacaine with 100μ morphine provides better quality of sensory block, faster onset sensory block with shorter duration of motor block, enabling early ambulation and significantly prolonged analgesia.
2.Introduction
3.Materials and Methods
3.1. Inclusion criteria
3.2. Exclusion criteria
3.3 Pre anaesthetic examination and preparation
3.4. Modified Bromage Scale
3.5. Post operative period
4.Statistical Analysis
5.Results
6.Discussion
7.Conclusion
8.References
Keywords
Ropicaine; Subarachonid Block; Perineal Surgery; Morphine; Intrathecal.
Introduction
For perineal surgeries intrathecal anaesthesia is a technique of choice. For this type of surgeries requires shorter duration of anaesthesia and prolonged analgesia is preferred. Hyperbaric lidocaine was drug of choice till the documenting the neurotoxicity of this drug prompting search for alternatives [1].The newer drug ropivacaine being comparatively less cardio toxic, produces minimal motor blockade of shorter duration, relieves the psychological distress of being immobile for a longer period of time after perineal surgeries. Ropivacaine is relatively new aminoamide, long acting enantiomerically pure local anesthetic with high pka and low lipid solubility. It is considered to block sensory nerves to greater degree than motor nerves and has similar local anesthetic properties and chemical structure to that of bupivacaine. Lack of post operative analgesic property due to short duration of motor block is the draw back with ropivacaine. Morphine as adjuvant intrathecally promotes the well know phenomena for post operative analgesia known since ages [2]. In this background the study is taken to assess the duration of sensory and motor block, time of ambulation, request for analgesia and also to asses any side effects when isobaric Ropivacaine is administered along with 100µ morphine given intrathecally in perineal surgeries.
Materials and Methods
The prospective study was conducted on 100 patients admitted at Bowring and lady Curzon hospital and Victoria hospital attached to BMC & RI, undergoing elective perineal surgeries from 2014 aug to 2015 nov. Institutional ethical committee approval was taken. Informed consent was obtained after explaining to patients /relatives in their vernacular language.
Hundred patients who fulfilled the inclusion and exclusion criteria were considered for the study. Patients were randomly divided into two group; study group and control group each comprising 50 patients.
Inclusion criteria
Patients in age group of 18-60 with ASA physical status I and II patients, were studied.
Exclusion criteria
Patients with history of allergy to amide local anaesthetics, any contra indications for spinal anaesthesia like bleeding or coagulation abnormalities, spinal deformities and local infection at the site of injection and if patients refusal were excluded from the study.
Pre anaesthetic examination and preparation
Pre anaesthetic check up was done a day prior to surgery. Patients were evaluated for any systemic diseases and laboratory investigations recorded. The procedure of spinal anaesthesia was explained to the patients and written consent was obtained. Patients posted for elective surgery were kept nil orally 10 hrs before the day of surgery and premedicated with 10 mg tab Dizepam 10 mg on previous night of surgery. Patients were pre loaded with ringer lactate 8 ml/per/kg body wt and Inj Ranitidine 150 mg and ondansetron 4mg was given before surgery in both the groups. Spinal anaesthesia was administered either in L3-L4 or L4-L5 space. All patient of study group received ropivacaine 3ml of 0.5% with 100µ morphine and without morphine in control group.
After administering the spinal anaesthesia HR, SBP, DBP, MAP, SPO2 and RR were measured in following order ie every 2 min for the first 10 min, every 5 min in the next 80 min and every 10 min till the end of surgery. Hypotension and bradycardia as defined as 20% decrease from base line values if developed was treated with IV bolus ephedrine 6mg and 1mg of atropine IV respectively. The level of sensory anaesthesia defined as the loss of pin prick sensation with 23G hypodermic needle at midclavicular level, was measured every min till it reached L1, T10 and maximum height of sensory block was also recorded. Two segment regression upto to S1 was recorded. The motor component was assessed for onset of motor block and duration of motor block. The motor block was assessed every minute using modified bromage scale of lower limb and then every 10 min until the return of normal motor function [3]. The time taken for complete motor block, complete recovery were recorded and ambulation time were recorded. Time when patient first complains of pain and request for rescue analgesia was also recorded.
Modified Bromage Scale
Grade 0 – No motor block.
Grade 1 – Can flex knee, move foot, but cannot raise leg.
Grade 2 – Can move foot only.
Grade 3 – cannot move foot or knee.
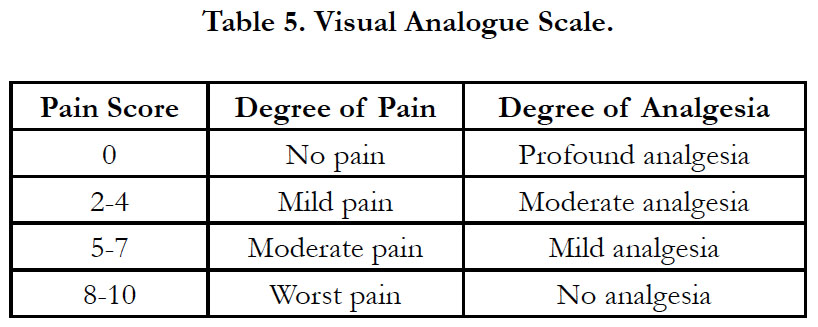
The intensity of pain was assessed using 10 point visual analogue
scale as no pain, mild, moderate and severe pain [Table 5].
Supplemental analgesia was given when the patient had moderated pain score of 5-6.
Post operative period
All the patients were observed in the post anaesthesia recovery room and then inward. The parameters such as SPO2, HR, SBP, DBP, MAP, and RR, sedation, pain and side effects like nausea, vomiting, pruritus and urinary retention were observed. All these were recorded every 30 min till 3 hrs, every hourly till 12 hrs and then every 4th hourly till 24 hrs.
Statistical Analysis
Descriptive and inferential statistical analysis has been carried out in the present study. Results on continuous measurements are presented on Mean SD [Min-Max] and results on categorical measurements are presented in Number (%). Significance is assessed at 5% level of significance. Student t-test (two tailed, independent) has been used to find the significance of study parameters on continuous scale between two groups (Inter group analysis) on metric parameters.
Significant figures: * Moderately significant (P value: 0.01<P 0.05) ** Strongly significant (P value <0.0001)
Statistical software: The Statistical software namely SAS 9.2, SPSS 15.0, Stata 10.1, MedCalc 9.0.1, Systat 12.0 and R environment ver.2.11.1 were used for the analysis of the data and Microsoft word and Excel have been used to generate graphs, tables etc.
Results
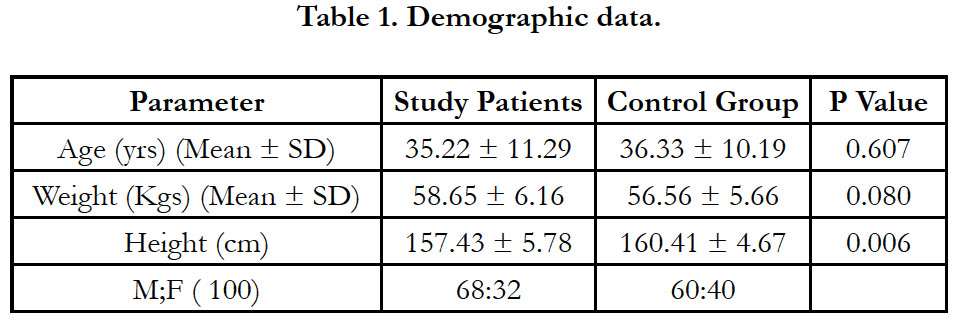
In this study hemodynamic parameter like HR, SPO2, SBP, DBP, RR were analysed.
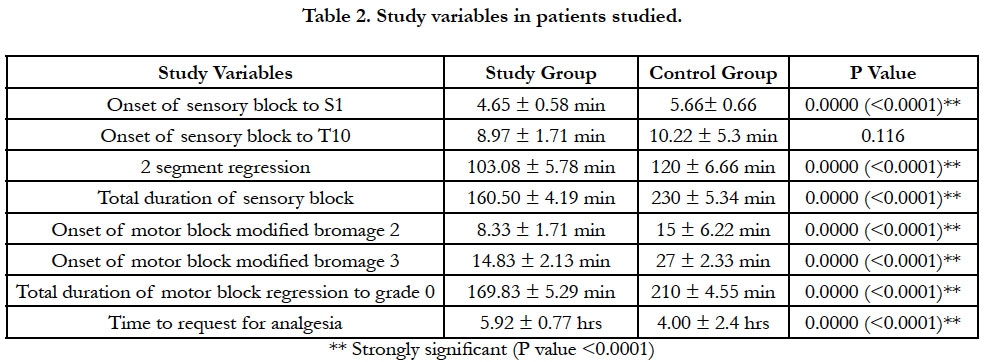
The mean time onset of sensory block at S1 level was 4.65 ± 0.58 and the same at T10 level was 8.97 ± 1.71 min with slower onset of block in study group. The mean time taken for two segment regression was 103.08 min and this was not statically significant. In the study group the mean duration of sensory block was 160.50 min which is significant with p value of 0.0000 (<0.0001).
In the study group mean time of onset of motor block modified bromage scale 3 was 14.83 ± 2.13, and the mean duration of motor block modified bromage zero was 169.83 ± 5.29 min and is significant (p < 0.0001) [Table 2]. The mean time to request for rescue analgesia was 5.92 hrs, and is statistically and clinically very significant in study group comparison to control group.
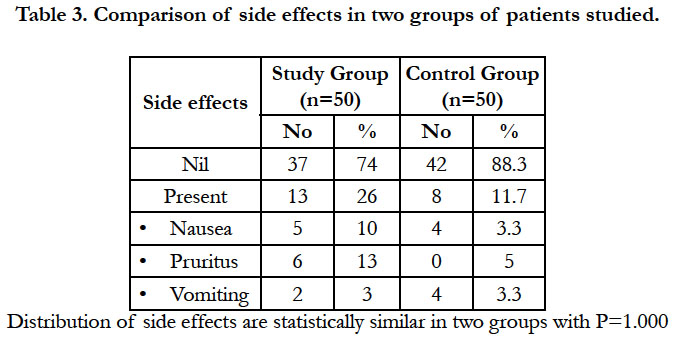
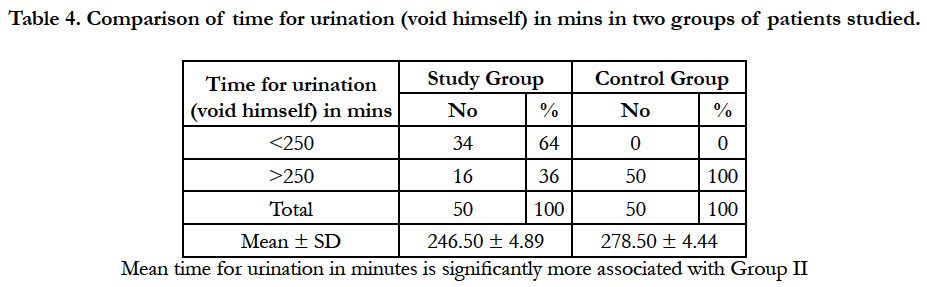
The post operative complication was seen in 13 % of patients, the most common complication being purities, while urine retention was observed in few patients in study group of patients [Table 3 & 4].
Discussion
Intrathecal procedure is definitive, easy to perform, less expensive with high success rate and is being practiced for longer of period time. The invention of opioid receptors in spinal cord introduced narcotic opioids as adjuvant for sub arachniod block along with local anaesthetic drugs. Neuraxial opioids provided excellent analgesia intraoperatively and postoperatively.
Perineal surgeries are pain full procedures requiring excellent analgesia intraoperatively and postoperatively [4]. Anesthesia is achieved with short acting sub arachanoid local anaesthetic agent with prolonged postoperative analgesia. Lidocaine has all the properties but is neurotoxic. Bupivacaine a long acting intrathecal local anaesthetic agent unfortunately has cardio toxicity [5]. Ropivacaine short acting local anaesthetic agent is free from all these complications but is devoid of analgesic effect [6]. Hence in the present study morphine was used as intrathecal adjuvant to achieve postoperative analgesia, along with ropivacaine.
Fettes p.d.w. et al in their study with isobaric and hyperbaric ropivacaine at dose of 15 mg they opined that isobaric ropivacaine are not suitable for surgeries above a dermatome level of L1 [7]. Gautier et al studied role of ropivacaine for ambulatory surgery and opined that 14mg of isobaric ropivacaine enables good intrathecal anaesthesia [6]. In present study we used 3ml of isobaric Ropivacaine with morphine in study group.
Mean time of onset of sensory block at T10 was 8.97 min in study group which is similar to Kumkum et al but they used fentanyl as adjuvant [8]. In control group onset of sensory block at T10 was 10.22 min which is similar to Fettes et al study [7]. We opine that ropivacaine with morphine adjuvant enables faster onset of sensory block.
Khaw et al. in their study with isobaric ropivacaine dose of 25mg documented 2 segment regression of 189 min. In our study 2 segment regression was 103.08 in study group and is lesser than their study with possible higher dose of isobaric ropivacaine used by Khaw et al. [9].
It also explains the fact that isobaric ropivacaine 15 mg with morphine has short duration of action and is stable for the surgeries of dermatome level less L1 as documented by Fettes [7].
Ogunal et al. studied effects of isobaric ropivacaine with dose of 15mg with morphine of 150 ug intrathecally and noted total duration of sensory block of 165.2min. In our study we observed total duration of 160.5 min, which is similar to their study [10].
Fettes et al. in his study conducted with only ropivacaine Observed total duration of sensory block was 240 min which is similar to that noted in control group [7]. This explains that addition of intrathecal narcotic adjuvant shorter the duration of sensory block as documented in our study group.
Kumkum G et al conducted study with isobaric ropivacaine 30 mg and fentanyl and the onset of motor block (min) modified bromage 3 was 14.2 min. While in our study it was 13.8 min similar to their study [8].
Total duration of block regression to grade zero was 169.8 min and 210.4 min in study group and control group respectively similar to Sangeeta varun et al who adopted adjuvant fentenyl [11]. But total duration of block is slightly prolonged to 200 min in Ogunal et al study with same drug and dosage. In control group total duration of motor block was 210 min similar to Kallio et al [12].
Kallio H et al concluded that total duration of motor block was 210 min when intrathecal adjuvant not used along with isobaric ropivacaine which is similar to our control [12]. so isobaric ropivacaine with morphine causes shorter duration of motor block which is beneficial in perineal surgeries.
Malinovsky et al. in their study in isobaric ropivacaine dose of 10 mg observed that total duration of block regression to grade 0 was 135 min, in present study it was 159.8 which was comparable [1].
Khaw et al study with isobaric ropivacaine dose of 25 mg with out intrathecal adjuvant they concluded that total motor block was 144.8 min which is similar to our study, but study conducted by Gupta et al with dose of 30 mg isobaric ropivacaine with fentanyl cause prolonged motor block was 267.0 min so higher the dose produces long duration of block [8, 9].
Erturk E, and Malinovsky JM conducted study with isobaric ropivacaine dose of 15mg with and without intra spinal adjuvant and concluded that isobaric ropivacaine produces less motor block, stable haemodynamics and minimal side effects [1, 2]. We also observed slow onset and prolongation of sensory block, shorter motor block and stable hemodynamic with no drop in BP and pulse rate less than 20% base line. In our study we observed less hemodynamic variation due to lower dermatome spinal block.
Fettes et al. studied with isobaric ropivacaine with dose of 15 mg with intra spinal adjuvant fentanyl opined that early ambulation with time duration of 218 min. In present study we absorbed time for ambulation was shorter that is 269.7 min in study group, which is similar to Fettes et al. study [7]. In control group time of ambulation was 245 min which is similar to study done by Gautier p h. et al which is 182 min with isobaric ropivacaine dose of 12 mg [6].
In our study group total duration of analgesia was 6.92 hrs which is comparable with Wahedi w et al and Ronald bathari et al studies who administered other opioid intrathecally along with isobaric ropivacaine [13,14].
Morphine 100 ug along with isobaric ropivacaine suitable requirement of short duration of anaesthesia in perineal surgeries with good analgesia and early ambulation.
The other side effects like nausea, vomiting and pruritis were seen in 13 patients only in which vomiting was highest seen in 8 patients. Study conducted by Chney MA observed nausea in 18% and vomiting in 7% patients [15].
Also we observed no neurological compilation with isobaric ropivacaine as reported by Kristensen et al [16].
Conclusion
Isobaric ropivacaine with dose of 15 mg along with intra spinal adjuvant morphine 100 ug results in faster onset and prolonged sensory block, shorter duration of motor block with prolonged postoperative analgesia and early ambulation with minimal side effects. We found this combination is excellent for perieneal surgeries.
References
- Malinovsky JM, Charles F, Kick O, Lepage JY, Malinge M, et al. (2000) Intrathecal anaesthesia: Ropivacaine verus bupivacaine. Anesth Analg 91(6):1457-1460.
- Erturk E, Tutuncu C, Eroglu A, Gokben M (2010) Clinical Comparison of 12 mg Ropivacaine and 8 mg Bupivacaine, both with 20 microg fentanyl, in spinal anaesthesia for major orthopaedic surgery in geriatric patients. Med Princ Pract 19(2): 142-147.
- Bromage PR (1978) Epidural analgesia. WB Saunders, Philadelphia. 144.
- Ipe S, Korula S, Varma S, George GM, Abraham SP, et al. (2010) A comparative study of intrathecal and epidural buprenorphine using combined spinal epidural technique for caesarean section. Indian J Anaesth 54(3): 205-209.
- Boztug N, Bigat Z, Karsli B, Saykal N, Ertok E (2006) Comparison of Ropivacaine and Bupivacaine for intrathecal anaesthesia during outpatient arthoscopic surgery. J Clin Anesth 18(7): 521-525.
- Gautier PE, De Kock M, Van Steenberge A, Poth N, Lahaye-Goffart B, et al. (1999) Intrathecal Ropivacaine for Ambulatory Surgery. Anesthesiology 91(5): 1239-1245.
- Fettes PDW, Hocking G, Peterson MK, Luck JF, Wildsmith JAW (2005) Comparison of plain and hyperbaric solutions of ropivacaine for spinal anaesthesia. Br J Anaesth 94(1): 107-111.
- Gupta K, Singhal AB, Gupta PK, Sharma D, Pandey MN, et al. (2013) Ropivacaine: Anesthetic consideration in elderly patients for transurethral resection of prostrate a clinical trial. Anesth Essays Res 7(2): 178-182.
- Khaw KS, Ngan Kee WD, Wong M, Ng F, Lee A (2002) Spinal ropivacaine for Cesarean delivery: a comparison of hyperbaric and plain solutions. Anesth Analg 94(3): 680-685.
- Ogun CO, Kirgiz EN, Duman A, Okesli S, Akyurek C (2003) Comparison of Intrathecal isobaric bupicacaine-morphine and ropivacaine-morphine for Caesarean delivery. Br J Anaesth 90(5): 659-664.
- Varun S, Srivastava M, Maurya I, Garg R, Dhama V, et al. (2012) A clinical prospective, randomized study to compare intrathecal isobaric bupivacaine – fentanyl and isobaric ropivacaine – fentanyl for lower abdominal and lower limb surgeries. Anaesth Pain & Intensive Care 16(3): 237-242.
- target="_blank">Kallio H, Snall EV, Kero MP, Rosenberg PH (2004) A comparison of intrathecal plain solution containing Ropivacaine 20 or 15 mg versus Bupivacaine 10 mg. Anesth Analg 99(3): 713-717.
- Wahedi W, Nolte H, Klein P (1996) Ropivacaine for spinal anesthesia. A dose-finding study. Anaesthesist 45(8): 737-744.
- Bathari R, Bhalotra AR, Anand R, Kumar V (2015) A randomised trial to compare the effect of addition of clonidine or fentanyl to hyperbaric ropivacaine for spinal anaesthesia for knee arthroscopy. Southern African J Anaesth Analg 21(5): 138-142.
- Chaney MA (1995) Side effects of intrathecal and epidural opioids. Can J Anaesth 42(10): 891-903.
- Kristensen JD, Karlsten R, Gordh T (1998) Spinal cord blood flow after intrathecal injection of ropivacaine and bupivacaine with or without epinephrine in rats. Acta Anaesthesiol Scand 42(6): 685-690.
- Kokki H, Ylönen P, Laisalmi M, Heikkinen M, Reinikainen M (2005) Isobaric Ropivacaine 5 mg/ml for Spinal Anesthesia in Children. Anesth Analg 100(1): 66-70.
- van Kleef JW, Veering BT, Burm AG (1994) Spinal Anesthesia with Ropivacaine: A Double-Blind Study on the Efficacy and Safety of 0.5% and 0.75% Solutions in Patients Undergoing Minor Lower Limb Surgery. Anesth Analg 78(6): 1125-1130.
- Jean-Marc M, Florence C, Ottmar K, Jean-Yves L, Myriam M, et al. (2000) Intrathecal Anesthesia: Ropivacaine Versus Bupivacaine. Anesth Analg 91(6): 1457-1460.
- McNamee DA, McClelland AM, Scott S, Milligan KR, Westman L, et al. (2002) Spinal Anaesthesia: Comparison of plain Ropivacaine 5 mg/ml with Bupivacaine 5 mg/ml for major Orthopaedic Surgery. Br J Anaesth 89(5):702-706.