Towards a Paramedical Interdisciplinary Definition of Fascia Supporting Practitioners Offering Fascia-Focused Therapies (Part 1)
John Sharkey1*, Mark Flannigan2
1 Clinical Anatomist, National Training Centre (NTC), 15-16a St Joseph’s Parade, Dorset St, Dublin DO7 FR6C, Ireland.
2 Neuromuscular Therapist, National Training Centre (NTC), 15-16a St Joseph’s Parade, Dorset St, Dublin DO7 FR6C, Ireland
*Corresponding Author
John Sharkey,
Clinical Anatomist, National Training Centre (NTC), 15-16a St Joseph’s Parade, Dorset St, Dublin DO7 FR6C, Ireland.
E-mail: john.sharkey@ntc.ie
Received: October 16, 2023; Accepted: November 28, 2023; Published: December 06, 2023
Citation: John Sharkey, Mark Flannigan. Towards a Paramedical Interdisciplinary Definition of Fascia Supporting Practitioners Offering Fascia-Focused Therapies (Part 1). Int J
Anat Appl Physiol. 2023;9(1):218-222.
Copyright: John Sharkey@2023. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Defining fascia in a manner that serves the needs of diverse allied professionals has proved elusive, leading to a cursory,
incomplete view of the tissue. The continuity of fascia is its defining characteristic but not its sole feature. Rather than a
definition that describes a passive dissectible tissue, an expanded meaning, informed by several years of dissections of Theilembalmed
and fresh from frozen cadavers, and up-to-date fascia-focused research is encouraged. This paper is not an attempt
to define fascia exclusively. Still, it is instead a proposal aimed at the Federative International Programme for Anatomical
Terminology to consider developing a new definition of fascia that emphasizes its pre-tensioned, highly sensory, omnipresent,
active, and functional role in the body.
Fascia is a continuous, penetrating, interconnected web that orchestrates and fine-tunes the body’s structure and functions.
Any tensional change in one location can affect the fascial network via mechanotransductive processes. In addition, fascial
tissues are richly innervated with sensory nerves that can stimulate the production of various neuropeptides and neurotransmitters
that influence emotions, stress response, and pain perception. Such a broad range of activity highlights the importance
of understanding the role of fascia in movement and manual therapies. Our proposal is offered to provide a satisfactory
interdisciplinary account and explanation concerning fascia, specifically for fascia-focused therapists. A more nuanced description
would be required for medical professionals, including surgeons and specialists involved in providing neural blocks;
the authors will provide this description in our second paper (i.e., part 2). A two-part wholistic description of fascia supports
communication among manual and movement practitioners and medical specialists.
In recent years, there has been an increased focus on the intricate role of fascia within the human body and its potential significance
in various therapeutic modalities. Paramedical therapists, who work closely with individuals seeking rehabilitation
and relief from so-called musculoskeletal issues, are vested in understanding the complexities of fascia. However, the current,
widely accepted definition of fascia must fully capture its multifaceted nature and therapeutic implications. This article proposes
a revised description of fascia tailored specifically for paramedical therapists, aiming to encompass the comprehensive
functions of fascia and provide a more nuanced understanding of its relevance in clinical practice.
The sixth International Fascia Research Congress [IFRC], organized by the Fascia Research Society, occurred in Montreal,
Canada, in September 2022. The IFRC seeks to share fascia research to inform better and unite medical, paramedical, and
nonmedical specialists. The ongoing and increasing success of the IFRC reflects continuous growth in interest in the broad
range of topics based on fascia science. This interest is not limited to medical experts but also involves a vast, disparate group,
including movement and manual therapists, bio-scientists, veterinarians, and other paramedical specialists—and therein lies
the problem.
With interest among practitioners offering fascia-focused therapies, including myofascial release, European neuromuscular
therapy, fascia integrated technique, osteopathy and myofascial induction, a definition of fascia is needed that is specific to the
requirements of all paramedical practitioners. A revised and expanded definition of fascia would give paramedical therapists a
more holistic understanding of its properties and functions, enabling them to provide more targeted and effective treatments.
2.Introduction
3.Conclusion
4.References
Keywords
Fascia; Connective Tissue; Anatomy; Nomenclature; Embryology; Manual Therapy; Movement Therapy; International
Federation of Associations of Anatomists (IFAA); Anatomy pedagogy; Dissection.
Introduction
Fascia is commonly described as a connective tissue matrix that
surrounds and supports the body's muscles, organs, and other
structures [1]. However, this traditional definition overlooks the
intricate web-like nature of fascia, which extends beyond mere
physical containment [2]. Research has increasingly revealed the
role of fascia as a dynamic and interconnected system affecting
movement, proprioception, interoception, pain perception, and
myofascial pain [3].
Paramedical therapists, including massage therapists, osteopaths,
and movement and neuromuscular therapists, must recognize the
crucial role of fascia in their practice [4]. However, the current
definition fails to convey the complex interactions and continuity
of fascia, muscles, and other physiological systems, thus limiting
their understanding [5]. According to Neumann et al., changes
to international standard anatomical terminology are necessary to
"correct errors in existing terms: names should not be changed
unless they are wrong; corrections of perceived errors should not
be pedantic; and inclusion of every minor structure should not be
attempted" [6].
Such changes are indeed necessary for the term fascia. An online
search using Google Scholar, Medline, PubMed, and other
databases such as that of the Fascia Research Society (https://
fasciaresearchsociety.org) reveals a wealth of words and phrases
for defining fascia: three-dimensional continuity [7], permeates
[8], ubiquitous [9], unified [10], structural matrix [11], and omnipresent
[12].
Currently, the term "fascia" (to tie, to bind, or a bandage) does not
have a set meaning across various scientific and clinical paramedical
disciplines, and numerous authorities agree that a scientifically
precise definition is lacking [7]. Furthermore, multiple sources
have highlighted the need for consensus on a modern definition
rather than the continued use of the 15th-century characterization
and description of fascia as a "band that ties" [8]. Beyond
the fact that there is no agreement concerning the definition of
fascia, evidence suggests that confusion and contradiction exist
regarding what fascia is, what it is not and what it can and cannot
do [9]. Recent commentary by Neumann et al. highlights that
the orthodoxy and relevance of the term "fascia" should be open
for further discussion [6]. This call is neither trivial nor pedantic.
Fascia has been the focus of much research and interest in recent
years, with a growing range of practitioners offering fasciafocused
therapies such as myofascial release, European neuromuscular
therapy, structural integration, myofascial manipulation,
fascia integrated technique, and myofascial induction, which are
all becoming increasingly popular. Despite this growing interest,
there needs to be an accepted definition of fascia specific to the
needs of practitioners offering fascia-focused therapies, underscoring
the need for a more inclusive definition of fascia [11].
Many terms used as an integral part of the language of anatomy
indicate very little about the physiology or metabolic role of a
named structure.
As a case in point, the term fascia, being of Latin origin with Indo-
European influences, describes a ribbon or a band (Figure 1).
The term was first proposed in the 15th century, likely as a reflection
of the resemblance of fascia to a bandage [7]. One of
the earliest recorded uses of the term "fascia" in its modern anatomical
sense was by the Italian anatomist Andreas Vesalius (also
known as Vesal) in the 16th century. Vesalius used the term to describe
the connective tissue layers surrounding muscles [22]. This
approach raises a question concerning the precise use of words in
anatomy, specifically pertaining to the topic of so-called layers in
human morphology. A question open to discussion is, "Do layers
exist in human anatomy, or do anatomists cut layers into existence?"
The word layer is convenient, referring to layers in human
connective tissue; however, it reflects a 17th-century model of
"parts" rather than a more realistic view of continuity [4]. The
term layer is undoubtedly suitable in geology, in which it refers to
strata of rock, sediment, and soil that can be visually identified as
distinct horizontal bands or sheets [23].
These layers can provide valuable information about the geological
history of an area, including the types of materials that were
present and the environmental conditions over time. Although
anatomists use layers as a convenient term to describe the organization
of tissues, they are not discrete strata like those described
in geology [23]. Instead, they are continuous sheets or planes that
are interconnected and not easily separated unless by dissection
[24].
Geological layers are often formed through external processes
such as erosion, sedimentation, and tectonic activity. In contrast,
the structures of the human body are shaped through internal,
tensegrity-informed embryonic processes, including cell differentiation,
tissue growth, and organ development [25]. As a result,
the organization of the human body is more complex and interconnected
than the relatively simple layering seen in geology [23,
25]. A prominent argument against the possibility of layers in the
human body is the study of stratigraphy [23]. Stratigraphy studies
layered materials [strata] that were deposited over time. The
fundamental law of stratigraphy, the law of superposition, states
that lower layers are older than upper layers unless the sequence
has been overturned [23].
Because this article relates to definitions, it is essential to mention
the use of the term fascia and the associated term "fascism."
Both terms have a common root in the Latin word "fascis," which
refers to a bandage or bundle of rods tied together with a band or
"wrapped around" [26].
In ancient Rome, such a bundle of rods represented the crushing
weight of the authority of magistrates. Over time, the word fascis
became associated with the idea of strength through unity, as the
rods were stronger when bound together than when separated, a
concept that induced respect and fear [26].
While the words "fascia" and "fascist" have a common Latin
root, they are not related in meaning, especially as the classical
Latin term specifically meant a band of material [26]. However,
some people could take offence to the word "fascia" due to its
shared etymology, and, therefore, it should be emphasized that
their meanings and contexts are distinct [26, 27]. Fascia reflects
strength through unity and the binding of disparate elements,
suggesting that ligaments are fascia. Anatomists adopted the
term "fascia" due to its function as a band binding together or
wrapping around so-called individual components into a stronger
whole [27]. As such, it is essential that the term "fascia" continues
to be used appropriately in the context of anatomy and paramedical
fields, where it is relevant and to avoid using it in a way that might be construed as insensitive or offensive.
It has been proposed that while avoiding synonyms and eponyms,
a proposal to identify location-specific fascia by using modifiers
such as "osseofascial" (bone), "neurofascial" (nerve), or "hemafascial"
(blood) could resolve the problem of developing an appropriate
definition [28]. Historically, each local fascia was named
after the anatomist who provided the first accurate anatomical
description; for example, Scarpa's fascia, located in the abdomen,
was named after Antonio Scarpa, an Italian anatomist [13]. Colle's
fascia was named after Irish surgeon Abraham Colle from Dublin
[14]. Camper's fascia was named after Petrus Camper, a Dutch
physician and anatomist [15]. Denonvilliers' fascia was named after
Paul Denonvilliers, a French surgeon [16]. Luschka's fascia was
named after Hubert von Luschka, a German anatomist [17] and
Gallaudet's fascia, the superficial investing fascia of the perineum,
was named after American anatomist Bern Budd Gallaudet. In contrast,
Gallaudet and Waldeyer's fascia is located between the pelvic diaphragm's
mesorectal parietal and presacral fasciae [18].
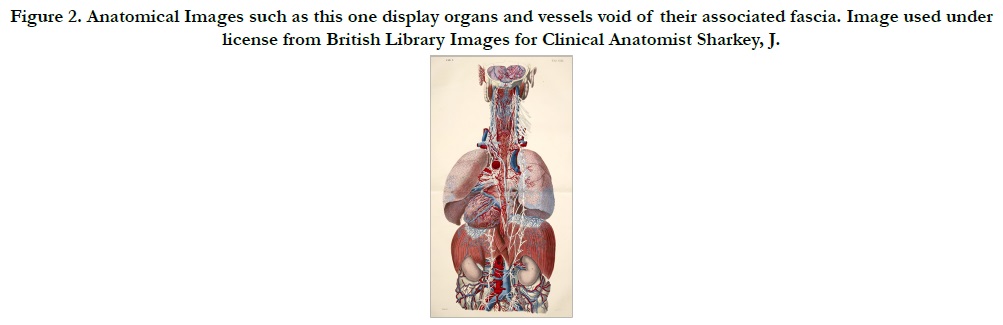
Most literary anatomical textbooks from the 15th century to the
modern era are littered with artistically embellished, antiseptic,
isolated body parts void of their fascia (See Fig. 2).
Good reasons existed for the focus on isolated parts and the
epistemological and subsequent metaphorical descriptions that
unfolded because this approach was an essential and fundamental
way for artists and anatomists, such as Leonardo da Vinci, to
appreciate, view, and investigate discreet structures or body parts;
omitting the integrated unifying role of fascia allowed a better
view of each part [19, 20]. Nevertheless, body parts need the neural
and vascular-rich fascia “body” to survive, although modern
techniques, including cryopreservation, can prolong the survival
of organ parts outside the body. Without the possibility of unification
with the body, a part cannot exist [21].
The topic of parts is complex and integrated into religion, art, science,
and politics. Having been associated with the arts for many
years, anatomy is recognized as the oldest of the medical sciences
[19]. Once perceived as simply a fragment of the whole, fascia has
come to be viewed as the tissue that connects the whole [7]. Further,
instead of local, individually separated fasciae set apart and
distinct from one another, a whole unified system has come to
light [2]. Thus, the need arises to negotiate a diplomatic solution
informed by a syntax that does justice to the actual reality of form
yet respects the honest efforts of pantheons of anatomy past [4].
To quote da Vinci “You will become acquainted with every part
and every whole by means of a demonstration of each part”.
In the modern era, anatomists are more informed regarding the
unified nature of this omnipresent connective tissue sculpted and
morphed from the embryonic origami, the mesenchyme [11].
Tensegrity construction principles provide a unified systems conception
of living form and function from micro to macro [24].
The tensegrity model offers a novel substitute for the established
biomechanical view of one muscle, one action, origins, and insertions
while combining fascia science with tensegrity research has
been referred to as “Fasciategrity” [10]. Fasciategrity provides a
new image of living constructs as self-developed, self-constructed,
self-emerging, self-stressed, unified systems within systems.
The Fasciategrity model encourages a move away from a “musculoskeletal
system” with muscles described as being “attached
to” bone and moves us towards a unified system, continuous,
soft matter construct that naturally expresses nonlinear behaviour
where disruption to one location can impact locally and globally
[10].
Fascia is a complex and dynamic contractile tissue playing a crucial
role in posture, pain perception, and motion; however, a more
detailed understanding of fascia is needed to support the development
of effective fascia-focused therapies [9].
For consideration, we propose not a definition per se but rather
two paramedical interdisciplinary descriptions of fascia, a short
and long version, informed by the latest clinical anatomy and
physiology research.
We present these descriptions for consideration by the Federative
International Programme for Anatomical Terminology, the
authority charged with defining fascia.
Our proposed short version is "Fascia is a pre-tensioned, dynamic,
unified, uninterrupted, complex, body-wide network of fibrous,
cellular, and adipose tissues surrounding, penetrating, supporting,
and compartmentalizing all structures from the cellular level to
the organ and organ systems level of the body."
Our proposed extended version is "Fascia constitutes a variety
of morphologically specialist tissues from liquid to osseous
composed of a variety of collagen and elastin fibres embedded
in a ground substance constituted by bound water, glycosaminoglycans,
and other extracellular matrix molecules on a spectrum
of softness (e.g., leptomeninges) to stiffness (e.g., bone). Fascia
is crucial in transmitting forces, maintaining posture, regulating
fluid balance, and providing sensory feedback. Human Fascia is
a continuous and ubiquitous three-dimensional web of pre-tensioned
connective tissue permeating and supporting every cell,
tissue, and organ of the body, providing structural integrity and
tensional balance. Fascia is composed of collagen, elastin, and
ground substance and is richly innervated and vascularized. Fascia
is not a passive container but a dynamic complex tissue constantly
remodelling in response to mechanical and biochemical stimuli,
modulating muscle function, bone health, fluidic dynamics, joint
stability, posture, pain, interoception and proprioception. Moreover,
Fascia plays a crucial role in intercellular communication,
emotions, immune defence, and inflammation regulation."
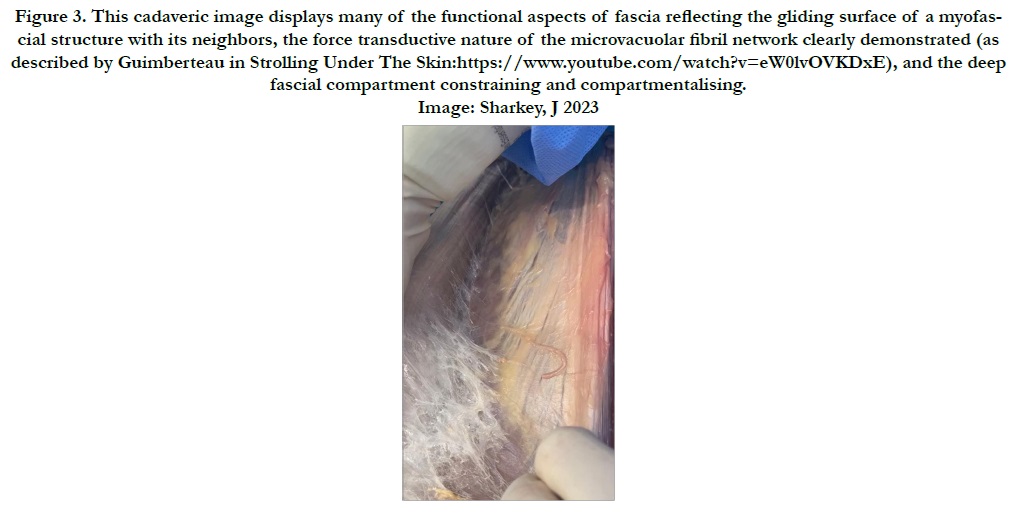
These short and long descriptions consider the recent advances in
fascia research, emphasizing the dynamic, unified nature of Fascia
[29]. In addition, a new classification of Fascia into functional hierarchical
categories supports these newly proposed descriptions
[30]. The new functional classification includes gliding, restraining,
containing, force transductive, communicative, septal, invaginating,
and osseofascial [30] [see Fig. 3].
Figure 1. Postcard, 1937, showing fasces-like decorative element [60cm in length with double-headed axe jointed to rods, all in iron] found in 1898 in “Tomb of the Lictor” at the Etruscan site of Vetulonia]. Courtesy T. C. Brennan.
Figure 2. Anatomical Images such as this one display organs and vessels void of their associated fascia. Image used under license from British Library Images for Clinical Anatomist Sharkey, J.
Figure 3. This cadaveric image displays many of the functional aspects of fascia reflecting the gliding surface of a myofascial structure with its neighbors, the force transductive nature of the microvacuolar fibril network clearly demonstrated (as described by Guimberteau in Strolling Under The Skin:https://www.youtube.com/watch?v=eW0lvOVKDxE), and the deep fascial compartment constraining and compartmentalising. Image: Sharkey, J 2023
Conclusion
The science of human anatomy is fluidic and constantly changing
as we learn to appreciate better this ubiquitous tissue we call
fascia. The call for recognizing the continuity of fascia is not new,
as evidenced by the writings of Dr. John D. Goodman, M.D.,
published in 1923. It is well-recognized and accepted that anatomists
and scientists have made efforts over many years to refine
anatomical knowledge, including accurately defining specific anatomical
terms and structures. It is our responsibility to continue to
do so. The proposed descriptions in this short paper, supported
by the new functional classification of fascia, provide a platform
for interdisciplinary communication. Fascia is a seamless process
giving continuity to the body, from the superficial to the deepest
organs, in a continuous network of tensional and compressional
forces called mechanotransduction. This means that a dysfunction
in one part of the fascial system can affect distant regions
or disrupt the whole-body balance, resulting in pain some distance
from the true source of the insult. This proposal highlights
the importance of fascia in homeostasis and providing sensory
feedback and interoception, an essential aspect of fascia-focused
therapies.
The authors hope this paper, and the proposals contained within,
will help the move toward a more inclusive definition of fascia
within the paramedical interdisciplinary communities of manual
and movement therapists.
References
- Bagley CA, Pindrik JA, Bookland MJ, Camara-Quintana JQ, Carson BS. Cervicomedullary decompression for foramen magnum stenosis in achondroplasia. J Neurosurg. 2006 Mar;104(3 Suppl):166-72. PubMed PMID: 16572633.,/
- Dickman CA, Spetzler RF, Sonntag VK, editors. Surgery of the craniovertebral junction. New York: Thieme; 1998 Jun.
- Wang Y, Xiao R, Yang F, Karim BO, Iacovelli AJ, Cai J, et al. Abnormalities in cartilage and bone development in the Apert syndrome FGFR2(+/ S252W) mouse. Development. 2005 Aug;132(15):3537-48. PubMed PMID: 15975938.
- Gardner WJ, Goodall RJ. The surgical treatment of Arnold-Chiari malformation in adults; an explanation of its mechanism and importance of encephalography in diagnosis. J Neurosurg. 1950 May;7(3):199-206. PubMed PMID: 15415776.
- Rogers TL. Determining the sex of human remains through cranial morphology. J Forensic Sci. 2005 May;50(3):493-500. PubMed PMID: 15932077.
- Hamilton ME. Sexual dimorphism in skeletal samples. Sexual dimorphism in Homo sapiens: a question of size. 1982:107-63.
- Giles E, Elliot O. Sex determination by discriminant function analysis of crania. Am J Phys Anthropol. 1963 Mar;21(1):53-68. PubMed PMID: 13947858.
- Franklin D, Freedman L, Milne N. Sexual dimorphism and discriminant function sexing in indigenous South African crania. Homo. 2005;55(3):213- 28. PubMed PMID: 15803767.
- FrancesquiniJúnior L, Francesquini MA, De La Cruz BM, Pereira SD, Ambrosano GM, Barbosa CM, et al. Identification of sex using cranial base measurements. J Forensic Odontostomatol. 2007 Jun;25(1):7-11. PubMed PMID: 17577972.
- Saini V, Srivastava R, Shamal SN, Singh TB, Kumar V, Kumar P, et al. Temporal variations in basicranium dimorphism of North Indians. Int J Legal Med. 2014 Jul;128(4):699-707. PubMed PMID: 24374986.
- Rösing FW, Graw M, Marré B, Ritz-Timme S, Rothschild MA, Rötzscher K, et al. Recommendations for the forensic diagnosis of sex and age from skeletons. Homo. 2007;58(1):75-89. PubMed PMID: 17306261.
- White TD, Black MT, Folkens PA. Human osteology. Academic press; 2011 Jan 21.
- Gruber P, Henneberg M, Böni T, Rühli FJ. Variability of human foramen magnum size. Anat Rec (Hoboken). 2009 Nov;292(11):1713-9. PubMed PMID: 19777568.
- Olivier G. Biometry of the human occipital bone. J Anat. 1975 Dec;120(Pt 3):507-18. PubMed PMID: 1213952.
- Routal RR, Pal GP, Bhagwat SS, Tamankar BP. Metrical studies with sexual dimorphism in foramen magnum of human crania. J AnatSoc India. 1984;33(2):85-9.
- Sayee R, Janakiram S, Thomas IM. Foramen magnum measurements of Crania from Karnataka. J AnatSoc India. 1987;36(2):87-9.
- RaghavendraBabu YP, Kanchan T, Attiku Y, Dixit PN, Kotian MS. Sex estimation from foramen magnum dimensions in an Indian population. J Forensic Leg Med. 2012 Apr;19(3):162-7. PubMed PMID: 22391003.
- Murshed KA, Çiçekcibasi AE, Tuncer I. Morphometric evaluation of the foramen magnum and variations in its shape: a study on computerized tomographic images of normal adults. Turk J Med Sci. 2003;33(5):301-6.
- Catalina-Herrera CJ. Study of the anatomic metric values of the foramen magnum and its relation to sex. ActaAnat (Basel). 1987;130(4):344-7. Pub- Med PMID: 3434189.
- Gapert R, Black S, Last J. Sex determination from the foramen magnum: discriminant function analysis in an eighteenth and nineteenth century British sample. Int J Legal Med. 2009 Jan;123(1):25-33. PubMed PMID: 18553095.
- Kamath V, Asif M, Shetty R, Avadhani R. Binary logistic regression analysis of hard palate dimensions for sexing human crania. Anat Cell Biol. 2016 Jun;49(2):151-9. PubMed PMID: 27382518.
- Kanchan T, Gupta A, Krishan K. Craniometric analysis of foramen magnum for estimation of sex. Int J Med Health Biomed Pharm Eng. 2013 Jul 29;7:111-3.
- Edwards K, Viner MD, Schweitzer W, Thali MJ. Sex determination from the foramen magnum. Journal of forensic radiology and imaging. 2013 Oct 1;1(4):186-92.
- Singh G, Talwar I. Morphometric analysis of foramen magnum in human skull for sex determination. Human biology review. 2013;2(1):29-41.
- Catalina-Herrera CJ. Study of the anatomic metric values of the foramen magnum and its relation to sex. ActaAnat (Basel). 1987;130(4):344-7. Pub- Med PMID: 3434189.
- Holland TD. Use of the cranial base in the identification of fire victims. J Forensic Sci. 1989 Mar;34(2):458-60. PubMed PMID: 2708959.
- Uysal S, Gokharman D, Kacar M, Tuncbilek I, Kosa U. Estimation of sex by 3D CT measurements of the foramen magnum. J Forensic Sci. 2005 Nov;50(6):1310-4. PubMed PMID: 16382824.
- Ukoha U, Egwu OA, Okafor IJ, Anyabolu AE, Ndukwe GU, Okpala I. Sexual dimorphism in the foramen magnum of Nigerian adult. Int J Biol Med Res. 2011;2(4):878-81.
- Uthman AT, Al-Rawi NH, Al-Timimi JF. Evaluation of foramen magnum in gender determination using helical CT scanning. DentomaxillofacRadiol. 2012 Mar;41(3):197-202. PubMed PMID: 22116135.
- Madadin M, Menezes RG, Al Saif HS, Abu Alola H, Al Muhanna A, Gullenpet AH, et al. Morphometric evaluation of the foramen magnum for sex determination: A study from Saudi Arabia. J Forensic Leg Med. 2017 Feb;46:66-71. PubMed PMID: 28157592.
- Kumar A, Dave M, Anwar S. Morphometric evaluation of foramen magnum in dry human skulls. Int J Anat Res. 2015;3(2):1015-23.
- Shanthi CH, Lokanadham S. Morphometric study on foramen magnum of human skulls. Med Sci. 2013;2(4):792-8.
- Kanodia G, Parihar V, Yadav YR, Bhatele PR, Sharma D. Morphometric analysis of posterior fossa and foramen magnum. J Neurosci Rural Pract. 2012 Sep;3(3):261-6. PubMed PMID: 23188974.
- Shepur MP, Magi M, Nanjundappa B, Havaldar PP, Gogi P, Saheb SH. Morphometric analysis of foramen magnum. Int J Anat Res. 2014;2(1):249-55.
- Patel R, Mehta CD. Morphometric study of Foramen Magnum at the base of human skull in South Gujarat. IOSR-JDMS. 2014 Jun;13(6):23-5.
- Loyal P, Ongeti K, Pulei A, Mandela P, Ogeng’o J. Gender related patterns in the shape and dimensions of the foramen magnum in an adult Kenyan population. Anatomy Journal of Africa. 2013;2(2):138-41.