Study On Effect Of Exercise On Fasting Blood Glucose Levels
GN Shashi Rekha1*, Asra Anjum2, Supriya Garapati3
1 Associate Professor, Department of Physiology, Mamata Academy of Medical Sciences, Bachupally, Hyderabad, Telangana State, India.
2 Tutor, Department of Anatomy, Mamata Academy of Medical Sciences, Bachupally, Hyderabad, Telangana State, India.
3 Professor and HOD, Department of Anatomy, Mamata Academy of Medical Sciences, Bachupally, Hyderabad, Telangana State, India.
*Corresponding Author
Dr. G N ShashiRekha,
Associate Professor, Department of Physiology, Mamata Academy of Medical Sciences, Bachupally, Hyderabad, Telangana State, India.
Tel: 7799572266
E-mail: drgnsrekha@gmail.com
Received: June 26, 2020; Accepted: July 20, 2020; Published: July 24, 2020
Citation: GN Shashi Rekha, Asra Anjum, Supriya Garapati. Study On Effect Of Exercise On Fasting Blood Glucose Levels. Int J Anat Appl Physiol. 2020;6(1):130-134. doi: dx.doi.org/10.19070/2572-7451-2000024
Copyright: GN Shashi Rekha©2020. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Diabetes mellitus (DM) is a group of metabolic diseases characterized by high blood sugar levels over a prolonged
period that further produces symptoms like frequent urination, increased thirst and increased hunger. Management of
Type 2 Diabetes Mellitus includes Medication or insulin therapy, regular exercise and healthy eating.
Objective: To study the effect of exercise on fasting blood glucose level in non-diabetics at the age of 22-25 years.
Materials and Methods: The study was conducted on 50 medical students. All the volunteers were male students of same
age group ranging from 20 to 25 years; they were carefully screened for any significant deviation of health from the normal
basal findings. The subjects were made to exercise for 30 minutes and the following observations were recorded.
Results: The mean age of the subject is 22 ± 2 years, mean height is 171 ± 11, mean weight is 67 ± 13 and mean body surface
area is 1.8 ± 0.2. The mean fasting blood glucose levels before and after exercise is 89 ± 5 and 85 ± 5 respectively and the p
value is 0.000,1 which is highly significant.
Conclusion: All forms of exercise produce small benefits in controlling the level of blood glucose. The effects are similar to
those of dietary, medication and insulin treatments.
2.Introduction
3.Materials and Methods
4.Results
5.Discussion
6.Acknowledgement
7.Conclusion
8.References
Keywords
Diabetes Mellitus; Insulin Therapy; Exercise; Body Surface Area.
Introduction
Man is living on the planet earth for over 2,000,000 years. The
earlier humans lived a nomadic existence of survival by hunting
and gathering food. Their way of life was entirely different from
the way people live today in developed countries, and this has profound
implications for pattern of disease and associated between
living habits and health.
Observation of few remaining nomadic groups in the world indicates
that they are relatively free of chronic diseases and are
comparatively leaner and have a higher level of physical fitness
with higher caloric expenditures per unit of body weight than do
modern individuals.
Due to limited active life much progress in the field of exercise and
physical condition is taking place. Exercise today has a scientific legitimacy due to research in physical education, exercise physiology
and medicine. Muscular exercise is the highest expression of
activities of the body and almost all the resources of the body are
mobilized in order to bring about the greatest efficiency of Neuromuscular
system. With urbanization and fast moving pattern of
life, the human being are dependent on vehicular transport and
the physical exertion has come to limited level; with the introduction
of home appliances, physical exertion of domestic life is also
limited. Due to these factors human beings are engaged in fast
activities but with limited physical exertion. The main problem of
urbanization is a desire or longing for physical exertion. This has
led to the concept of centers for tailored or programmed physical
activity where subjects are prescribed physical activity based on
their age, sex and health status and requirements.
Need for exercise is now a conscious desire of every human being
because of increase awareness of hazards of inactive life, like the occurrence of diseases such as Diabetes Mellitus, hypertension,
obesity and cardiovascular accidents. These are the chain of
diseases with a common base of less active and a more sedentary
life which leads to more accumulation and less expenditure of
calories. Going by saying “ use or loose” either one should use
his/her all the body mechanics or loose all and end as a handicap.
Mother of diseases, obesity predisposes the individual to increase
demands of insulin, which if not available will lead to diabetes
mellitus. Diabetes mellitus is a disease which damages all the organs
of the body, if not controlled properly and in proper time.
Diabetes is characteristically of two types. Type 1 Diabetes Mellitus,
is due to the body’s failure to produce sufficient insulin due to
an autoimmune condition that causes destruction of the insulin
producing beta cells in the pancreas. Type 2 Diabetes Mellitus is
characterized by a combination of peripheral insulin resistance
and inadequate insulin secretion by pancreatic beta cells. Insulin
resistance, which has been attributed to elevated levels of free
fatty acids and pro-inflammatory cytokines in plasma, leads to decreased
glucose transport into muscle cells, elevated hepatic glucose
production, and increased breakdown of fat [1].
Management of Type 2 Diabetes Mellitus includes Medication or
insulin therapy, regular exercise and healthy eating. Medications
are chosen based on factors such as blood glucose levels and the
health problems faced by the patient [2]. Physical activity or structured
exercise training used alone or in combination with diet,
insulin injections, or oral hypoglycemic drugs are the foundations
of therapy for type 2 diabetes [3].
Skeletal muscle is responsible for most of the uptake of glucose
after a meal, and transport of glucose into the muscle is considered
the limiting step in glucose disposal [4, 5]. Glucose transport
occurs primarily by diffusion utilizing glucose transporter carrier
proteins (GLUT). Both exercise and insulin regulate glucose
transport mainly by the translocation of the GLUT4 isoform
from an intracellular compartment to the plasma membrane and
transverse tubules [6, 7] GLUT4 levels are considered an important
determinant of insulin sensitivity [4, 5].
Continuous glucose monitoring (CGM) systems provide continuous,
dynamic blood glucose testing, contributing to the discovery
of hyperglycemia and hypoglycemia that are not easily detected by
traditional monitoring methods [8].
Many people do not exercise despite the proven benefit of endurance
exercise. An exercise program requiring less time commitment
may appeal to some people. The aim of this paper is to
review the impact of high-intensity exercise of short duration on
blood glucose levels in diabetic and nondiabetic people.
Materials and Methods
The study was conducted on 50 medical students. All the volunteers
were male students of same age group ranging from 20 to
25 years, they were carefully screened for any significant deviation
of health from the normal basal findings. The subjects were made
to exercise for 30 minutes and the following observations were
recorded.
Age, Height, weight and Body Surface Area were measured using standard methods.
Measuring the height: The subject was asked to stand on a flat
surface and take of his shoes, head bands or anything else from
the head that may get in the way of an accurate measurement. The
subject was asked to stand against a wall making sure his head,
shoulders and buttocks are touching the wall. Line of sight and
chin should be parallel to the floor. Using a wall mounted metallic
tape measure, the height of the subject is measured.
Measuring the weight: Digital weighing balance was used to
measure the weight of the students. Before starting the measurement
the scale was adjusted to zero. The students were asked
to take off heavy clothings (such as coats, jackets ± and vests),
purses, shoes and heavy accessories such as belts with heavy belt
buckles. They should also remove everything from their pockets
including money (coins), pens, pencils, wallets, and papers. Each
student was asked to step on the scale and stand motionless in
the middle of the scale platform with the feet slightly apart and
the body weight distributed equally on both feet. Arms should be
relaxed and hanging down loosely at the sides of the body. Digital
scales are very sensitive to movement and any movement will
change the weight measurement, so students must stand very still
and the readings were recorded.
Measuring the Body Surface Area: Body Surface Area (BSA)
measures the total surface area of the body. The Mosteller formula
is most commonly used formula in practice and in clinical
trials. The Mosteller formula takes the square root of the height
(cm) multiplied by the weight (kg) divided by 3600.
BSA (m)2 = √(Height (cm) X Weight (kg)/3600
Estimation of blood glucose is by King & ASA Toor Method.
Principle: First depolarization is done by using sodium tungstate
and enodiols of sugars reduces cupric to cuprous ions, which react
with Arsenomolybdic acid and forms molybdenum blue. The
blue colored complex formed is measured by colorimeter.
Reagent used: Isotonic reagent, it consists of Na2SO4 and CUSO4.
1) Na2SO4 - prevents hemolysis and eliminates non reducing sugars
and non carbohydrate reducing acid.
CUSO4 - provides cupric (CU++) ions
2) Sodium Tungstate – it precipitates the proteins
3) Alkaline Tartrate – Provides alkaline medium and protects cupric
ions by complex formation.
4) Arsenomolybdic acid – For color development.
5) Stock – Standard of glucose : It is prepared by adding 100mg
of glucose in 100ml of Benzoic acid.
6) Working standard of glucose: It is prepared by dissolving 2.5ml
of spot glucose standard in 100ml of Isotonic reagent.
7) Distilled water:
Procedure:
Depolarization: A solution is made in a test tube by taking 3.8ml
of isotonic reagent, 0.1ml of blood and 0.1 ml of sodium tungstate.
Centrifuge the test tube and the superlated layer is protein
free filtrate which is kept aside.
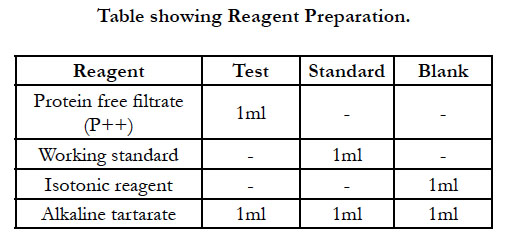
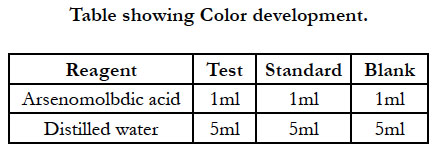
Reduction: Take 3 test tubes, label them as test standard and
blank. Boil all the test tubes for 10 minutes and cool it for 5 minutes.
Adjust the colorimeter to zero by using blank take O.D. value
of test and standard at 548 nm (green filter).
Results
The study was conducted on 50 medical students. All the volunteers
were male students of same age group ranging from 20 to
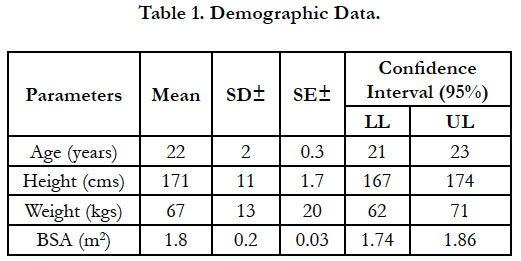
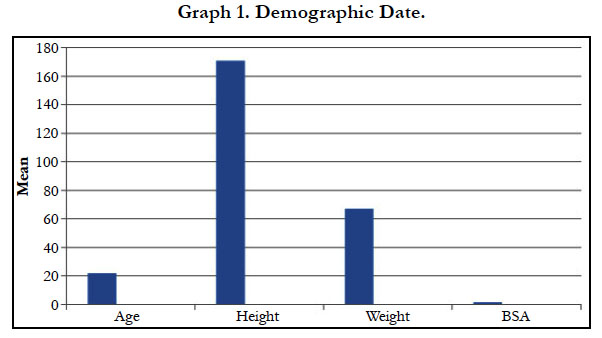
25 years. The mean age and Standard deviation of the students is
22 ± 2 years and standard error of mean is 0.3. The lower limit
of the confidence interval (95%) is 21 years and upper limit is 23
years (Table 1 and Graph 1).
The mean height is 171 ± 11 years with standard error of mean
1.7. The lower limit of the confidence interval (95%) is 167 cms
and upper limit is 174 cms (Table 1 and Graph 1).
The mean weight of the students is 67 ± 13 kgs with standard error
of 20. The lower limit of confidence interval (95%) is 62 kgs
and upper limit is 71 kgs (Table 1 and Graph 1).
The mean Body Surface Area (BSA) is 1.80 ± 0.2 m2 with standard
error of mean 0.03. The lower limit of confidence interval is
1.74 m2 and upper limit is 1.86 m2 (Table 1 and Graph 1).
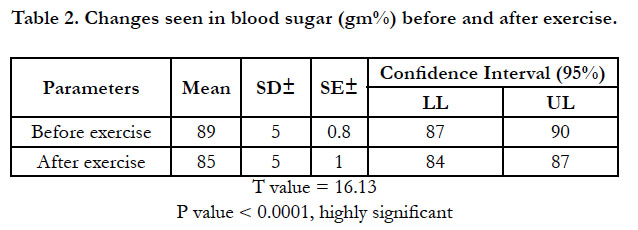
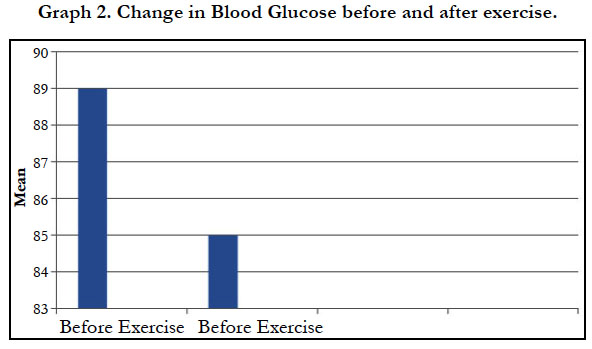
The mean blood sugar level before and after exercise is 89 ± 5 gm% and 85 ± 5 gm% respectively with standard error of mean 0.8 and 1.0 respectively. The lower limit of confidence interval (95%) of blood sugar before and after exercise is 87 gm% and 84 gm% respectively. The upper limit of confidence interval (95%) of blood sugar before and after exercise is 90 gm% and 87 gm% respectively. The t value is 16.13 and p value is <0.0001 which is highly significant (Table 2 and Graph 2).
Discussion
This study was conducted on 50 students of same age group
ranging from 20 – 25 years, carefully screened for any significant
deviation of health from normal basal findings. The subjects were
made to exercise for 30 min and changes in blood sugar levels are
observed.
Changes seen in blood glucose level was significantly decrease
with mean value of 89 to 85 gm% with t value of 16.3 and p value
< 0.0001 which is significant.
This fall of blood glucose level is seen in all subjects who were
made to exercise hence it can be stated that physical exercise decreases
blood glucose level. With the knowledge that during exercise
there occurs increase release of catecholamine and ACTH
both of which cause glycogenolysis and rise in blood glucose levels.
The very fact that instead of rise in blood sugar in exercise
there occurs fall in blood sugars, indicate that more and more blood glucose is being utilized by exercising muscle. This supported
by study on adreno-receptors present on beta cells of pancreas.
These receptors increase insulin secretion.
There is also evidence to show that exercise increases insulin sensitivity
of cells, so that blood sugar can more readily be taken
within the cells and is utilized. The effect of exercise on blood
glucose levels is utilized in prescribing exercise as a part of treatment
of diabetes mellitus.
Larsson et al., (1962) noted a lower PWC (physical working capacity)
in diabetic adolescent girls compared with normal girls of the
same age. They also found a regular decrease in blood sugar of the
diabetic girls during work; this effect was especially conspicuous
on those girls with a high blood sugar level. After training, PWC
increased in most subjects but there was no increase in the insulin
requirement in spite of a 50% increase in caloric consumption [9].
Decreased PWC in diabetic girls was confirmed by Sterky (1963)
and in diabetic boys by Larsson et al., (1964) [10, 11]. In the former
study, this reduction did not seem to be directly connected
with the diabetic state but may have been the result of inadequate
training since these diabetic girls were less active than normal
girls. Conflicting results on diabetic girls and boys were reported
by Elo et al., (1965) who also noted that duration of disease and
insulin requirement had a low correlation with PWC [12].
Dangiashwini et al., has compared the fasting blood glucose
levels both before and after yoga and aerobics exercise. In both
the groups the blood glucose levels decreased and the p value
is 0.0001 which is found to be significant. This author also suggests
that both Yoga and aerobic exercise are effective in reducing
blood glucose levels in patients with Type 2 Diabetes Mellitus
[13].
Management of Type 2 Diabetes Mellitus includes medication or insulin therapy, regular exercise and healthy eating. Medications
are chosen based on factors such as blood glucose levels
and the health problems faced by the patient. Common medications
include Metformin, which improves the sensitivity of the
body tissues to insulin and lowers glucose production in the liver.
Sulfonylureas are also used and these help the body secrete more
insulin. Meglitinides work similar to sulfonylureas except that they
are faster acting and do not stay active in the body for long [2].
Yoga, the traditional exercise form, offers a largely unexplored,
widely available resource for the management of stress-related
ailments. There is evidence that Yoga can benefit patients with
Type 2 Diabetes Mellitus. A randomized, controlled trial of Yoga
for patients with Type 2 Diabetes Mellitus showed that both Fasting
Blood Glucose and Hb1Ac improved significantly along with
patients reporting that they felt better, less anxious and more in
control of themselves [14].
Type 2 Diabetes Mellitus is characterized by a combination of peripheral
insulin resistance and inadequate insulin secretion by pancreatic
beta cells. Insulin resistance, which has been attributed to
elevated levels of free fatty acids and pro-inflammatory cytokines
in plasma, leads to decreased glucose transport into muscle cells,
elevated hepatic glucose production, and increased breakdown of
fat [1].
These studies suggest that exercise is a useful adjunct to other
forms of diabetes management. Unfortunately, most have focused
on only one segment of the diabetic population, those taking
insulin. This reviewer has found no research on the effects of
exercise on the larger number of adult-onset diabetics who are
able to control their diabetes by oral hypoglycemic drugs and/ or
proper diet. Much more information is needed on the acute and
long-term effects of regular exercise and training on the course
and severity of the entire spectrum of diabetes mellitus. Again,
many factors must be controlled before definitive information on exercise can be brought to the attention of the physician and his
diabetic patient.
Acknoldegements
I most humbly acknowledge the students who co-operated me
to take the data for the article. I also acknowledge the authors,
editors and publishers of all those articles, journals and books
from where the literature for this article has been reviewed and
discussed.
Conclusion
Studies on the effect of high-intensity exercise on blood glucose
have been few and of short duration, and have involved a small
number of patients who were probably not representative of the
general diabetic population. With diabetics, it is therefore uncertain
if any improvements in blood glucose achieved by a brief
intervention would be sustained over a longer period, reduce
HbA1c levels, improve health outcomes, and can be replicated
in the general dia¬betic population. Similarly, in the nondiabetic
population it is not known whether improvements in insulin sensitiv-
ity would be sustained and results in a clinically important
endpoint such as diabetes prevention.
References
- Khardori R. Type 2 Diabetes Mellitus. American Association of Clinical Endocrinologists, American Diabetes Association. The Endocrine Society. 2014; 18(6): 745-749.
- Nathan DM. Initial Management of Glycemia in Type 2 Diabetes Mellitus. NEJM. 2002 Oct; 347(17): 1342-1349.
- Meltzer S, Leiter L, Daneman D, Gerstein HC, Lau D, Ludwig S, et al. Clinical practice guidelines for the management of diabetes in Canada. Can Med Assoc J. 1998; 159 (Suppl. 8):S1– S29.
- Hughes VA, Fiatarone MA, Fielding RA, BB Kahn, CM Ferrara, P Shepherd. Exercise increases muscle GLUT-4 levels and insulin action in subjects with impaired glucose tolerance. Am J Physiol. 1993; 264(6 Pt 1): E855– E862. PMID: 8333511.
- Houmard JA, Egan PC, Neufer PD, JE Friedman, WS Wheeler, RG Israel. Elevated skeletal muscle glucose transporter levels in exercise-trained middleaged men. Am J Physiol. 1991; 261(4 Pt 1): E437–E443. PMID: 1928336.
- Colberg SR, Sigal RJ, Fernhall B, Judith G Regensteiner, Bryan J Blissmer, Richard R, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement executive summary. Diabetes Care. 2010; 33(12): 2692–2696. PMID: 21115771.
- Goodyear LJ, Kahn BB. Exercise, glucose transport, and insulin sensitivity. Annu Rev Med. 1998; 49: 235–261. PMID: 9509261.
- Fonseca VA, Grunberger G, Anhalt H, Timothy S Bailey, Thomas Blevins, Satish K Garg, et al. Continuous glucose monitoring: a consensus conference of the American Association of Clinical Endocrinologists and American College of Endocrinology. Endocrine Practice. 2016; 22(8): 1008–1021. PMID: 27214060.
- Larsson Y, Sterky G, Ekengren K, Moller T. Physical fitness and the influence of training in diabetic adolescent girls. Diabetes. 1962; 11: 109-117. PMID: 14462559.
- Sterky G. physical work capacity in diabetic school children. Acta Pediatr. 1963; 52: 1-10. PMID: 13983920.
- Larsson Y, Persson B, Sterky G, Thoren C. Functional adaptation to vigorous training and exercise in diabetic and non-diabetic adolescents. J. Appl Physiol. 1964; 19: 629-635.
- Elo O, Hirvonen B, Peltonen T, Valimaki I. Physical working capacity of normal and diabetic children. Ann Paediatr fenn. 1965; 11: 25-31. PMID: 14292771.
- Ashwini D, Dhwani R, Medha D. A comparative study of the effect of yoga versus aerobic exercise on blood glucose level and quality of life in patients with type 2 diabetes mellitus. Int J Health Sci Res. 2017; 7(1):146-152.
- Viveka P, Ansumali J, Smita Ambekar, Neeta Kumar, Anju Dhawan, Vishnubhatla Sreenivas. Comprehensive yogic program improves quality of life in patients with NIDDM. Indian J Endocrinol Metab. 2012; 16(3): 423– 428. PMID: 22629512.