Effect of Teaching Strategies on Academic Performance of Junior Medical Students
AlShaikh G1, Ibrahim G2,3, Shahzad S2, Fayed A2, Al Mussaed E2, Syed S2*, Elmorshedy H2,4
1 King Khalid Hospital, King Saud University, Riyadh.
2 College of Medicine, Princes Nourah bint Abdulrahman University, Riyadh.
3 Department of Biochemistry, Suez Canal University, Egypt.
4 Department of Tropical Health, High Institute of Public Health, University of Alexandria, Egypt.
*Corresponding Author
Dr. Sadiqa Badar Syed,
Professor of Physiology, College of Medicine,
Princess Nourah bint Abdulrahman University, Saudi Arabia.
E-mail: sasyed@pnu.edu.sa
Received: September 18, 2019; Accepted: October 25, 2019; Published: October 28, 2019
Citation: AlShaikh G, Ibrahim G, Shahzad S, Fayed A, Al Mussaed E, Syed S, et al., Effect of Teaching Strategies on Academic Performance of Junior Medical Students. Int J Anat Appl Physiol. 2019;5(4):124-129. doi: dx.doi.org/10.19070/2572-7451-1900023
Copyright: Syed S©2019. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: To evaluates the effectiveness of problem-based learning (PBL) versus lecture based learning (LBL) as a learning tool in terms of retention, recall and reproducibility of knowledge among junior medical students.
Methodology: This Post-test experimental study was conducted on 2nd year medical students (n=54) of College of Medicine, Princess Nourah bint Abdul rahman University, Riyadh, KSA. Ten topics taught each by PBL and lectures with comparable scientific content and complexity levels, selectedfrom the five blocks of first year. Two multiple choice questions exams were developed, comprising 50 scenario-based questions each, covering concepts in Physiology, Biochemistry, Pathology and Microbiology.
Results: The average score for PBL questions was 25.46 out of 50 compared to 20.26 for LBL (P <0.001). The percentage of students with scores >60% were 22.2% and 5.5% for PBL and LBL exams, respectively. Linear regression analysis between students’ scores in PBL and LBL exams showed a moderate positive correlation (r = 0.6358; P ≤ 0.001). Stratification according to GPA demonstrated that both the high achievers and the rest of students performed better on PBL taught topics. In addition, difference in scores between the two strategies were reproducible (P<0.001)
Conclusion: The study confirms that PBL is an effective teaching tool in terms of retention and recall of knowledge after a period of 6 to 8 months as compared to interactive lectures for undergraduate medical students.
2.Introduction
3.Methodology
3.1 Statistical Analysis
4.Results
5.Discussion
6.Conclusion
7.Acknowledgement
8.Authors’ Contribution
9.References
Keywords
Problem-based Learning; Lecture-based Learning; Junior Medical Students; Knowledge Retention.
Introduction
Medical educationist and researchers have long been working to develop strategies to enhance students’ competencies and skills and to promote retention of knowledge for longer duration, critical thinking and lifelong learning [1]. Determination of the best pedagogy to teach medical students with current complexity and expansion of knowledge, advanced technology and specialization is still a debatable matter [2].
Two major learning strategies problem-based learning (PBL) and traditional lecture-based learning (LBL) are the foundations of the hybrid curriculum. PBL is a student-centered, collaborative learning involving student actively in determining their prior knowledge, their learning objectives and the sources to access new information [3]. Moreover, PBL prepares students to face real life problems as it integrates different disciplines and subdisciplines and serves to bridge the gap in the knowledge [4].
The multidisciplinary integrated problem-based curriculum being practiced in majority of medical schools has well defined, interrelated learning objectives and provides evidence-based education (EBE) which relies on real life clinical scenarios [5]. Practice of PBL provides a systematic approach starting with analyzing the problem, acquiring related data, suggesting appropriate investigations based on rationale and figuring out answers to predetermined objectives [6]. Thus, students develop effective problem solving skills by facilitating brain storming among small groups of students (self-directed learning) [7].
Compared to PBL, a didactic lecture in LBL is an oral presentation of facts with organized thoughts and ideas prepared by a qualified teacher specialized in the subject. However, the major disadvantage of LBL is the passive role of students where they are merely listeners and are not actively engaged in education. In addition, they are encouraged to learn facts without understanding the background, as the emphasis is on examination-oriented learning of details [8]. However, though teacher centered, LBL has its own advantages such as the quality of lectures have been much improved with proper integration and sequencing of learning objectives along with addition of selected and animated pictures of the mechanisms and disease processes. Also, information is usually updated, resources are valid and reliable and difficult concepts can be addressed clearly [9].
A study documented that students preferred PBL because of motivation boost, quality learning, knowledge retention and practical usefulness of contents, however in the case of answering the exams questions, lecture method was considered more effective presumably because of teacher’s emphasis on important key points [10]. Another study reported that combining PBL and LBL produce better outcomes for learning rather than either method alone in a clinical setting [11]. On the contrary a study demonstrated that traditional method (LBL) prepare better doctors for internship as compared to PBL [12].
Since the paradigm has completely shifted from teacher-centered to learner-centered education, an ideal curriculum should comprise most appropriate and effective instructional strategies with long term retention [13]. Different modes of learning are documented to have different impacts on level of retention after two months period. Level of retention is directly related to the degree of active participation and involvement of students in the education process being 20% for lectures, 30% for audiovisual, 50% for group discussion and 85% for practice by doing. Accordingly, a combination of instructional strategies including lectures, tutorials, case studies, group projects, practical sessions and demonstrations are preferred [14].
College of Medicine in Princess Nourah bint Abdul rahman University (CM-PNU) for women Riyadh, Saudi Arabia was established in 2012 as an undergraduate program. The teaching strategies follow an integrated hybrid Problem-based curriculum with weekly PBLs incorporated with lectures. Because students’ performance is among the key indicators reflecting the quality of educational process, the faculty in College of Medicine is keenly interested to evaluate the impact of different teaching strategies on learning outcomes and retention of knowledge among students.
Although, literature search has shown several studies devoted to evaluate teaching strategies, yet most of them involve assessment of short term recall of information among clinical students after a rotation in a medical ward or a selected module, course or a single instructional session of short term duration, [10, 11, 15] or they encompass other health related disciplines such as physiotherapy, pharmacy, physician assistant courses etc. rather than medical students. Moreover, majority of studies relied solely on subjective opinion of students rather than on an objective valid examination. In view of these observations, there was a need to assess long term retention of knowledge for a period of more than 8 to 10 months in basic medical sciences knowledge among preclinical medical students in KSA. The main aim of study was to compare the effects of these two learning strategies PBL versus LBL on retention, and reproducibility of knowledge. The study was not meant to assess the perceptions of students as documented in most of these studies but it evaluated the performance of 2nd year medical students using objective multidisciplinary basic science exams.
Methodology
A post-test self-controlled experimental study with convenient sampling was conducted on 2nd year medical students (n=54) in CM-PNU Riyadh.
All second year medical students were invited to participate in the research after a comprehensive explanation of the study aim and objectives along with the right to withdraw at any stage. They were informed that their GPA will be used during analysis of the results and researchers confirmed the confidentiality of the results. Fifty nine students accepted to participate in the study of which only 54 students were able to complete the study. A verbal consent was obtained from all participants. The study was granted the approval from the IRB Committee of the College of Medicine, PNU.
Ten topics taught each by PBL and lectures were designated from the five blocks of first year MBBS. PBL topics with powerful scenarios have been developed by a committee comprising Heads of the departments of basic sciences subjects. Strong triggers were provided to develop effective problem solving skills. During PBL sessions, students were intrinsically motivated by working on the challenging task as a team. Interactive lectures were prepared by faculty members after attending workshops on preparation of effective power-point presentations. Lectures were scrutinized by a committee for comparable scientific content, complexity level and content validity and delivered by same faculty members who conducted the PBL sessions to minimize the intersubject variability.
One hundred multiple choice questions (MCQs) with one correct option were prepared in two papers, based on learning objectives of PBL and LBL as well as blueprint which is essential to ensure exam validity. Paper-I comprised 50 MCQs from topics taught in 10 PBL sessions in five blocks i.e. Dehydration and Anxiety in Foundation block, Myasthenia gravis and Intervertebral disc prolapse in Musculoskeletal block, Asthma and Tuberculosis in Respiratory block, Mitral stenosis and Myocardial Infarction in Cardiovascular block and Acute kidney injury and Urinary tract Infection in Renal block. Paper-II included 50 MCQs covered in lectures from the same blocks but emphasizing concepts which were taught in lectures only. This includes cell injury including inflammation and neoplasia from Foundation block, carbohydrate metabolism and arthritis from Musculoskeletal block, pulmonary circulation with zones of lungs and regulation of respiration from Respiratory block, electrocardiogram and blood pressure regulation from Cardiovascular block, tubular reabsorption plus secretion and glomerulonephritis from Renal block. MCQs were scenario based testing the concepts in Physiology, Biochemistry, Pathology and Microbiology. The inter-subject variability is minimized by careful selection of content material.
The exams questions were meant to test the comprehension level of Bloom’s cognitive domain and ability to retain information after 6 to 8 months duration and therefore taken in the 2nd week after the summer vacation of the new scholastic year 2015-2016. The two exams were held on two separate days and the duration of the exam was one hour each. Questions were approved by the exam committee as high quality MCQs.
To minimize the possible information bias, the PBL and the lectures were conducted by the same facilitators who were not aware about the aim of the study. Thus confounding factors such as knowledge of tutor, interactive delivery of lectures and emphasis on key points were omitted. Since most of the faculty members belonged to traditional teaching background, extensive faculty development programs were provided for facilitation of this curriculum to the tutors by a series of workshops. To name a few, the workshops included curriculum development, new educational technologies concerning the biology of teaching and learning strategies, effective and interactive power-point presentation, interactive lecturing in small and large groups, becoming PBL facilitators and how to develop PBL scenarios, bioinformatics, methods of assessment and evaluation etc. The continuous professional development resulted in improved teaching quality and competency of faculty members with an improvement in their ability to reflect their own teaching strategies and to promote reasoning power of students. They also developed relevant new topics of PBLs as well as prepared high quality interactive lectures on power point presentations.
Statistical analysis was performed using SPSS, version 18.0. Descriptive statistics was used in terms of means, medians and standard deviations. Continuous variables were tested for normality using Kolmogorov-Smirnov test. Wilcoxon Signed Ranks was used for paired comparison of scores and Man-Whitney test for unpaired comparison. P-value less than 0.05 was considered as statistically significant.
Results
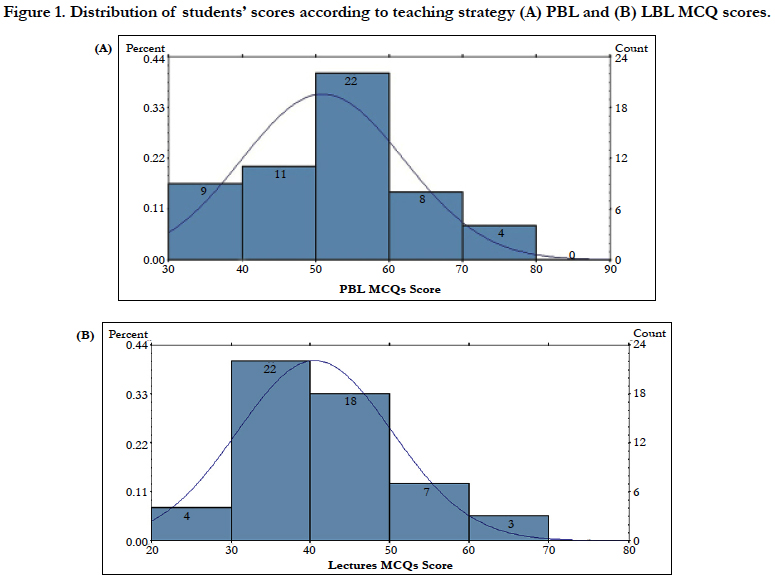
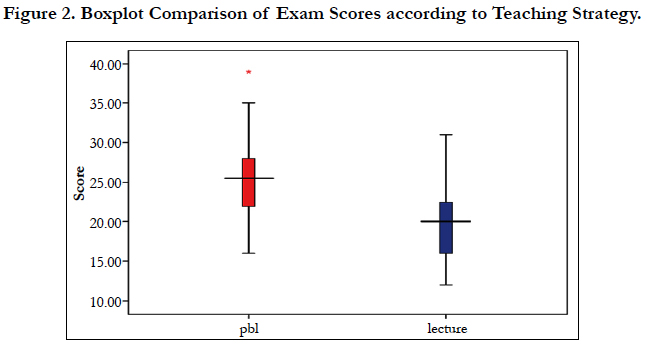
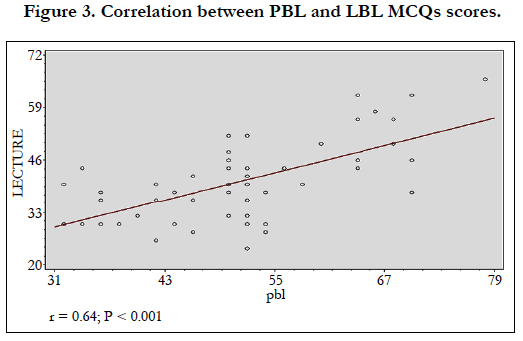
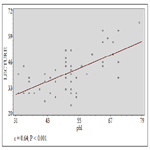
The average score achieved after the PBL session was 25.46 ± 5.51 out of 50, (median 25.5 and range: 16 – 39).12/54 (22.2%) of the students had a score above 60% (Figure 1a). On the other hand, the average score attained after the conventional lecture was 20.26 ± 4.88 (median 20.0, range: 12 to 23). Only 3/54 (5.5%) of the students had a score above 60% (Figure 1b). The 95th percentile score for the PBL was 35, whilst that of conventional lecture was 31, moreover, the 25th percentile score for the PBL was 21.75 and as for the lecture it was 16. Figure (2) displays the boxplot comparison of scores attained after PBL and lecture sessions. Statistically significant difference was detected and confirmed by the use of paired comparison using Wilcoxon Signed Ranks with a P-value <0.001.Positive moderate correlation between students’ scores in BPL and LBL was found to be statistically significant (r = 0.64; P < 0.001) (Figure 3).
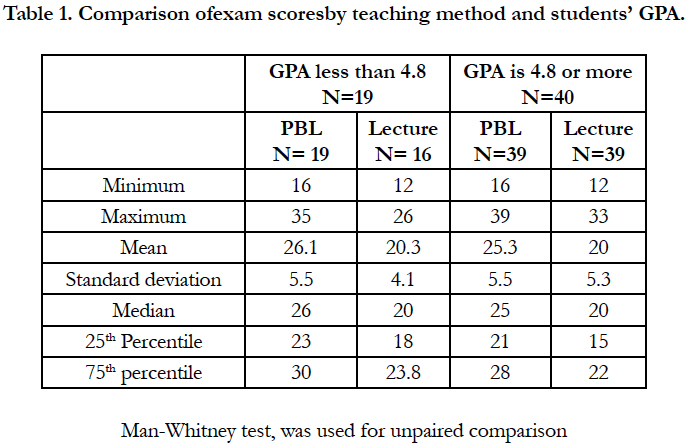
Stratification of students based on their GPA into two strata was adopted to shed more light on the achieved scores by PBL and LBL among different groups of GPA. Two strata were studied; one stratum of those who have GPA less than 4.8 (19 students) and the other group whose GPA was 4.8 or more (40 students). Table (1) shows the comparison of scored achieved by students after PBL and LBL with stratification of GPA. Students achieved significantly higher scores in BPL compared to LBL within each stratum of GPA (p value < 0.01).
Discussion
The PBL approach in medical education is considered most significant educational innovation in the past four decades. Integrating active learning in curricula enhances self-directed learning and promotes problem-solving skills, professionalism, leadership collaboration, and cultural competency [16-18]. At College of Medicine, PNU, curricula are based on blended learning approach utilizing both PBL and LBL. Because evaluation of teaching strategies is critical for newly established program as it will provide the basis for monitoring and reforms, this study was conducted to evaluate PBL versus LBL.
Most of published data rely on subjective measures to evaluate the PBL (e.g. students/tutors satisfaction, perception and beliefs). In our study, PBL was evaluated based on an objective exam prepared and validated by faculty. In addition, the evaluation was conducted after summer vacation to allow for testing knowledge retention after a relatively long duration. The exam was constructed as MCQs based on case scenarios, and the topics selected allowed for determining students’ knowledge and problem-solving skills. Along with literature highlighting the efficacy of PBL on retention of knowledge and problem-solving skills in different study settings, including medical schools and other health colleges, [19, 20] our results demonstrate that the overall mean score for PBL is significantly higher than that of LBL. To delineate further, for the PBL teaching method, the 95th percentile score, the 25th percentile and the median were evidently higher than the LBL score. Moreover, for the PBL method, 22.2% of students had a score above 60%versus 5.5% for the LBL. The assessment tool in this study was MCQs based on case scenarios which require higher thinking skills. While in PBL, students develop autonomous learning abilities for higher cognitive skills [21], it can be assumed that in LBL, students have minimal opportunities to develop higher thinking skills and to enhance their problem solving abilities. This difference in the teaching method explains the eminent difference between the two scores. Finally, our results clearly denied the claim that, for PBL students performed better on clinical examination, while they score lower on basic sciences [22].
In confirmation, results of meta-analysis including 11 intervention studies in pediatric education showed that the PBL group was superior to the LBL group in the theoretical test score, medical and case analysis score [21]. However, immediate evaluation of PBL vs LBL for a graduate pharmacology course revealed that both approaches were equally effective with no significant difference for the middle of term, final and end of course examination scores [23]. However, the sample size was small and therefore the results can’t be generalized.
In the present study, although the mean scores of PBL were significantly higher than the mean score of LBL, yet there was a moderate linear correlation between students’ scores for PBL and their scores for conventional lectures. This finding may be a reflection of students’ cognitive abilities, i.e. whoever good in PBL is predicted to be good for LBL. The observation that the correlation between the two scores is just moderate is expected in view of differences in the competencies associated with the teaching methods (PBL vs. LBL).
It is worth mentioning that for PBL, different assessment tools do not correlate. For example, the overall OSCE performance did not correlate with the written-examination scores as reported bySalinitri and colleagues [24]. The attributes of these results are related to student’s self-learning tools required for OSCE [25] where students are more engaged in practice by doing audiovisual and group discussions. These active participation tools enhance more retention of knowledge than less active ones, for example, searching information in texts and web.
Regarding our students’ satisfaction about PBL, this was published earlier where positive perception was maximum for integration of basic science into clinical knowledge and critical thinking. Also, majority valued the PBL in enhancing communication skills and promoting positive interpersonal relations [26]. Similar findings were reported from Qassim University, KSA 18. These results together with the present study clearly show that despite students were not exposed to PBL before admission to medical school, they face no problem to adapt easily with the PBL system and they score even better.
Conclusion
In the integrated multidisciplinary basic science program of the first two years at PNU Medical School, the PBL system revealed a significantly higher score than the LBL. This indicates the higher performance of the PBL for the retention of knowledge and problem solving skills. The study also demonstrated a moderate correlation between the BPL and the LBL scores. Based on the better performance in the PBL, the authors assume that junior students have accepted this system efficiently. Data provided evidence regarding 6 to 8 months duration of knowledge retention; however Interactive lectures with proper learning objectives, sequencing, animations and videos also help in long term retention of medical information.
Acknowledgement
The authors would like to thank students for their enthusiasm to participate in the study and take the test immediately after summer vacation at the inception of the new scholastic year.
Authors’ Contribution
Ghadeer Al-Shaikh, participated in the study design, reviewing the assessment tool and preparing the manuscript for publication. Hala Elmorshedy, suggested study design, wrote the discussion and revised the manuscript. Gehan Ibrahim, contributed in the construction of the assessment tool, wrote the methodology, contributed in the analysis of data and in reviewing the manuscript for publication. Amel Fayed, Contributed in the analysis of data, wrote the results and participated in reviewing the manuscript for publication. Sadiqa Syed, contributed in the construction of the assessment tool and participated in reviewing the manuscript for publication. Saira Shahzad, contributed in the construction of the assessment tool and wrote the introduction. Eman AlMussaed provided all facilities to carry out the study and reviewed manuscript.
References
- Landeen J, Jewiss t, Vajoczki S, Vine M. Exploring consistency within a problem-based learning context: perceptions of students and faculty. Nurse education in practice. 2013 Jul;13(4):277-82.
- Mellon AF, Mellon J. Logical debate on problem based learning. Bmj. 2006 Mar 2;332(7540):550-1.
- Hwang SY, Kim MJ. A comparison of problem- based learning and lecturebased learning in an adult health nursing course. Nurse Education Today. 2006 May;26(4):315-21.
- Schmidt HG, Rotgans JI, Yew EH. The process of problem‐based learning: what works and why. Medical education. 2011 Aug; 45(8):792-806.
- Harmer A, Lee K, Petty N. Global health education in the United Kingdom: a review of university undergraduate and postgraduate programmes and courses. Public Health. 2015 Jun 1;129(6):797-809.
- AlAmodi AA. Problem-based learning sessions and undergraduate research: a medical student’s perspective and experience. Perspectives on medical education. 2014 Jan 1;3(1):56-60.
- Reich S, Simon JF, Ruedinger D, Shortall A, Wichmann M, Frankenberger R. Evaluation of two different teaching concepts in dentistry using computer technology. Advances in health sciences education. 2007 Aug 1;12(3):321-9.
- Khan H, Taqui AM, Khawaja MR, Fatmi Z. Problem-based versus conventional curricula: influence on knowledge and attitudes of medical students towards health research. Plos one. 2007 Jul 18;2(7):e632.
- Lauver LS, West MM, Campbell TB, Herrold J, Wood GC. Toward evidence-based teaching: evaluating the effectiveness of two teaching strategies in an associate degree nursing program. Teaching and Learning in Nursing. 2009 Oct 1;4(4):133-8.
- Khoshnevisasl P, Sadeghzadeh M, Mazloomzadeh S, Feshareki RH, Ahmadiafshar A. Comparison of problem-based learning with lecture-based learning. Iranian Red Crescent Medical Journal. 2014 May;16(5).
- Yang LH, Jiang LY, Xu B, Liu SQ, Liang YR, Ye JH, et al. Evaluating teambased, lecture-based, and hybrid learning methods for neurology clerkship in China: a method-comparison study. BMC medical education. 2014 Dec;14(1):98.
- Millan LP, Semer B, Rodrigues JM, Gianini RJ. Traditional learning and problem-based learning: self-perception of preparedness for internship. Revista da Associação Médica Brasileira. 2012 Oct; 58(5):594-9.
- Inglis A, Ling P, Joosten V. 2002. Delivering digitally, managing the transmission to the knowledge media, Kogan Page London, p20.
- Barnett R. Knowing and becoming in the higher education curriculum. Studies in higher education. 2009 Jun 1;34(4):429-40.
- Ozuah PO, Curtis J, Stein RE. Impact of problem-based learning on residents' self-directed learning. Archives of pediatrics & adolescent medicine. 2001 Jun 1;155(6):669-72.
- Nii LJ, Chin A. Comparative trial of problem-based learning versus didactic lectures on clerkship performance. American journal of pharmaceutical education. 1996 Jun 1;60(2):162-4.
- Jungnickel PW, Kelley KW, Hammer DP, Haines ST, Marlowe KF. Addressing competencies for the future in the professional curriculum. Am J Pharm Educ. 2009 Dec 17;73(8):156.
- Shamsan B, Syed AT. Evaluation of problem based learning course at college of medicine, Qassim University, Saudi Arabia. International journal of health sciences. 2009 Jul; 3(2):249.
- Koh GC, Khoo HE, Wong ML, Koh D. The effects of problem-based learning during medical school on physician competency: a systematic review. Cmaj. 2008 Jan 1;178(1):34-41.
- Lin CF, Lu MS, Chung CC, Yang CM. A comparison of problem-based learning and conventional teaching in nursing ethics education. Nursing ethics. 2010 May;17(3):373-82.
- Gao X, Luo S, Mu D, Xiong Y, Guanjian L, Wan C. Effects of problembased learning in paediatric education in China: a meta‐analysis. Journal of Evidence‐Based Medicine. 2016 Aug;9(3):136-43.
- Seifer SD. Recent and emerging trends in undergraduate medical education. Curricular responses to a rapidly changing health care system. Western Journal of Medicine. 1998 May;168(5):400.
- Miller SK. A comparison of student outcomes following problem-based learning instruction versus traditional lecture learning in a graduate pharmacology course. J Am Acad Nurse Pract. 2003 Dec; 15(12):550-6.
- Salinitri FD, O'Connell MB, Garwood CL, Lehr VT, Abdallah K. An objective structured clinical examination to assess problem-based learning. American journal of pharmaceutical education. 2012 Apr 10;76(3):44.
- Kirton SB, Kravitz L. Objective structured clinical examinations (OSCEs) compared with traditional assessment methods. American journal of pharmaceutical education. 2011 Aug 10;75(6):111.
- Al-Shaikh G, Al Mussaed EM, Altamimi TN, Elmorshedy H, Syed S, Habib F. Perception of medical students regarding problem based learning. Kuwait Medical Journal. 2015 Jun 1; 47(2):133-8.