Variations of Sciatic Nerve Bifurcation: A Study
Sangeetha V, Divya Shanthi D'Sa*
Assistant Professor, Subbaiah Institute of Medical Sciences, Shimoga, Karnataka, India.
*Corresponding Author
Dr. Divya shanthi D’Sa
Assistant Professor, Department of Anatomy,
Subbaiah Institute of Medical Sciences, NH-13,
Purle, HH Road, Shimoga: 577222, Karnataka, India.
Tel: 9448579590
E-mail: drdivyadsa17@gmail.com
Received: November 13, 2017; Accepted: November 29, 2017; Published: November 30, 2017
Citation: Sangeetha V, Divya Shanthi D'Sa. Variations of Sciatic Nerve Bifurcation: A Study. Int J Anat Appl Physiol. 2017;3(3):80-83. doi: dx.doi.org/10.19070/2572-7451-1700013
Copyright:Divya Shanthi D'Sa© 2017. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: The sciatic nerve (SN) is the thickest nerve in the body. It is formed in the pelvis from the ventral rami of the fourth lumbar to the third sacral spinal nerves and leaves the pelvis via the greater sciatic foramen below pyriformis and divides into Common Peroneal nerve (CPN) and Tibial nerve (TN) at the superior angle of popliteal fossa. High division of the sciatic nerve is the most common variation wherein the TN and the CPN may leave the pelvis through different routes. Such variations may lead to compression of the nerve, non discogenic sciatica, pyriform syndrome and also to incomplete sciatic nerve block. Knowledge regarding this may help the surgeon to plan for various surgical intervention pertaining to the gluteal region.
AimTo study the course and division of sciatic nerve.
Methodology: The study was conducted in the department of Anatomy, Subbaiah Institute of Medical Sciences over a period of 5 years. 70 lower extremities of 35 cadavers of both sexes were studied to see the variations in sciatic nerve bifurcation. Beaton and Anson classification has been followed for the classification of division of Sciatic nerve.
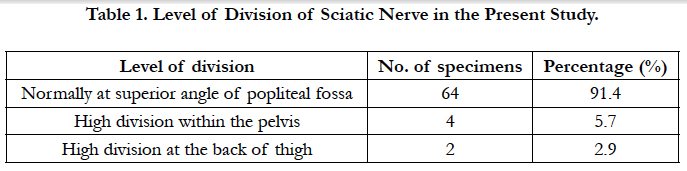
Results: In our study on 70 lower extremities of 35 cadavers, we observed 6 (8.6%) high division of SN. Among these, 2 (2.9%) lower extremities showed high division in the back of thigh and 4 (5.7%) showed within the pelvis. The remaining 64 (91.4%) lower extremities showed the division outside the pelvis
Conclusion: Knowledge regarding the variation in the level of division of the sciatic nerve and its pelvic exit is of utmost importance in order to prevent inadvertent injury to the nerve during various surgical interventions in the gluteal region.
2.Introduction
3.Materials and Methods
4.Observation and Results
5.Discussion
6.Conclusion
7.References
KeyWords
Sciatic Nerve; Pyriformis; Tibial Nerve; Common Peroneal Nerve.
Introduction
Sciatic is a Greek word derived from ‘ischiadicus’. Sciatic nerve is also known as ischiadic nerve or ischiatic nerve, is a large nerve in humans and other animals [1]. The sciatic nerve is the thickest nerve in the human body formed in the pelvis by the ventral rami of L4-S3 spinal nerve roots. It is about 2cm wide and leaves the pelvis through the greater sciatic foramen below the pyriformis and descends between the greater trochanter and ischial tuberosity in the gluteal region. The nerve divides subsequently into two terminal branches, Tibial and common peronial nerve usually at the superior angle of popliteal fossa. It is a mixed nerve with the motor branches supplying the posterior group of thigh muscles as well as hip and knee joint. Its sensory component supplies the whole tibial and foot areas with the exception of the anteromedial tibial region and the medial margin of the foot [2].
Sciatic nerve presents a significant variation in its topography and division. Higher level of division of the sciatic nerve anywhere in the thigh or in the pelvis is commonly seen. In the pelvis, the whole nerve or its branches may emerge either below, above, or through the pyriformis. High division of the sciatic nerve may be unilateral or bilateral usually leading to compression of nerve resulting in pyriformis syndrome and also incomplete block of sciatic nerve during popliteal block anaesthesia.
Variant course of sciatic nerve may lead to injury during operations in the gluteal region, non discogenic sciatica, coccygodynia. This causes paralysis or paresis of the thigh muscles with sensory disturbances. Hence present study was undertaken to know the level of sciatic nerve exit in relation to pyriformis and the level of division of the nerve.
Materials and Methods
The study was conducted in the department of anatomy, Subbaiah Institute of Medical Sciences, Shimoga on 70 lower extremities of 35 cadavers. The course and division of the sciatic nerve was observed and variations were minutely noted. The gluteal region, back of the thigh and popliteal fossa were exposed by dissection. The gluteus maximus muscle was cut from it insertion and reflected towards its origin. The biceps fermoris muscle was retracted and the nerve was then exposed in the popliteal fossa. The exit of the nerve from pelvis, its relation to pyriformis and level of division of the nerve were noted. In most of the specimens the sciatic nerve had a normal course. However in six cadavers, high division of sciatic nerve was observed and grouped according to Beaton and Anson classification [3, 4].
Observation and Results
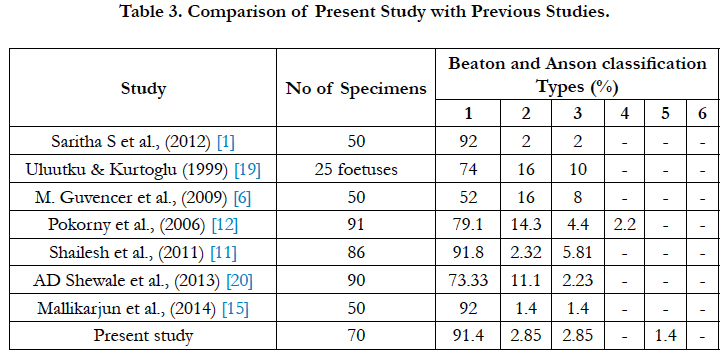
In our study on 70 lower extremities of 35 cadavers, we observed that the sciatic nerve emerged as a single trunk below the pyriformis in 64 lower extremities (Type 1- 91.4%). In two lower extremities, sciatic nerve emerged below the pyriformis and had divided, the divisions later united with each other in the middle one third of the thigh and finally dividing into Tibial Nerve and Common Peroneal Nerve at superior angle of popliteal fossa (Type 2- 2.85 %). In two other lower extremities, the two components of sciatic nerve emerging above and below the pyriformis (Type 3-2.85%).
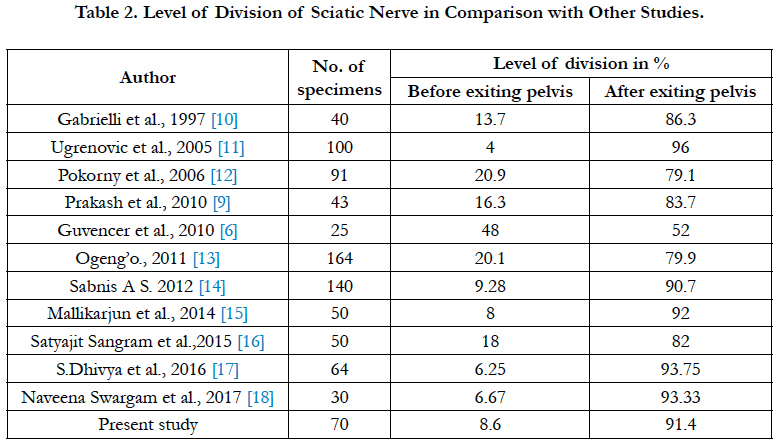
In another specimen, Tibial nerve emerged below the pyriformis and Common Peroneal Nerve emerged through the pyriformis muscle (Type 5-1.4%). In one case we observed high division of SN in pelvis & the TN passing beneath the muscle and CPN passed through the pyriformis muscle was noted (1.4%). The results of the study are tabulated in Table 1-3 and shown in Figure 1-4.
Discussion
During embryological development at the base of the limb bud, the nerves contributing to the lower limb form two plexuses (lumbar and sacral). Later, as the elements from each of these plexuses grow out into the limb, they are subdivided into dorsal and ventral components, for the dorsal and ventral musculatures. The sciatic nerve is formed when the large dorsal component of the sacral plexus (common peroneal nerve) and the ventral component (tibial nerve) move downward close together [5]. Hence, based on their developmental formation, it is possible that the common peroneal and the tibial divisions of the sciatic nerve separate from each other at different levels from their origins: within pelvis, in the gluteal region, the posterior compartment of the thigh or the popliteal fossa.
High division of Sciatic nerve has been classified into different types by various authors. Beaton & Anson [3, 4] classified variations of the pyriformis and SN in 120 specimens in 1937, and in 240 specimens in 1938. Their classification, known as the Beaton & Anson classification, is as follows:
Type 1: Undivided nerve below undivided muscle
Type 2: Divisions of nerve between and below undivided muscle
Type 3: Divisions above and below undivided muscle
Type 4: Undivided nerve between heads
Type 5: Divisions between and above heads
Type 6: Undivided nerve above undivided muscle
In the present study, high division of SN in the back of thigh was noted in two specimen (2.9%) and high division of sciatic nerve in the pelvis was noted in 4 specimens (5.7%). These variations corresponded with type 1, type 2, type 3 and type 5 of above classification. In one case we observed high division of SN in pelvis & the TN passing beneath the muscle and CPN passed through the pyriformis muscle (1.4%). This type of variations has been termed as Beaton and Anson type 6 [6, 7]. The variations in the course, division and distribution of SN have been reported in earlier literatures. The present study was compared with these studies and is depicted in Table 2, 3.
The level of division of the SN greatly influences the extent of neurological deficit in sciatic neuropathy. It may account for failure of SN block while performing popliteal block anesthesia. Pyriformis syndrome is caused by an entrapment of SN as it exits the greater sciatic notch [7, 8]. Reunion of CPN and TN in the back of thigh, after dividing in the pelvis as seen in the present study may complicate the evaluation and interpretation of sciatic, common peroneal, tibial neuropathy and nerve block. It also provides the anatomical basis for spontaneous re-innervation of muscles following nerve injury [9]. Hence these variations have to be kept in mind during various operative procedures in the gluteal region.
Conclusion
High division of nerve can lead to nerve injury during deep intramuscular injections, failure of sciatic nerve block anesthesia during various surgical procedures, pyriformis syndrome and damage to sciatic nerve during varicose vein stripping. Variations in the course of the nerve may complicate surgery and in the interpretation of sciatic neuropathy. Thus the knowledge of anatomical variation in the level of division of the sciatic nerve and its exit from the pelvis plays important clinical significance in preventing injury to the nerve and its subsequent complications during various surgical procedures.
References
- Saritha S, Praveen Kumar M, Supriya G. Anatomical variations in the bifurcation of the sciatic nerve, a cadaveric study and its clinical implications. Anat Physiol. 2012;2(5):111.
- Standring S, Mahadevan V, Collins P, Healy JC, Lee J, Niranjan NS. Gray’s Anatomy. The Anatomical Basis of Clinical Practice. 40th ed. Spain, Philadelphia-Churchill Livingstone Elsevier. 2008;1368-1371.
- Beaton LE, Anson BJ. The relation of sciatic nerve and its sub divisions to the piriformis muscle. Anat Rec. 1937;70(1):1-5.
- Beaton LE. The sciatic nerve and piriform muscle: Their interrelation possible cause of coccgodynia. J Bone Joint Surgery Am 1938;20(3):686-688.
- Moore KL, Persaud TV. The Developing Human: clinically oriented embryology. 8th ed. Elsevier:2008;368-371.
- Guvencer M, Iyem C, Akyer P, Tetik S, Naderi S. Variations in the high division of the sciatic nerve and relationship betwen the sciatic nerve and the piriformis. Turk Neurosurg. 2009 Apr;19(2):139-44. PubMed PMID: 194331123.
- Guvencer M, Iyem C, Aleyer P, Tetik S, Naderi S. Anatomic considerations and the relationship between the piriformis muscle and the sciatic nerve. Surg Radiol Anat. 2008;30(6):467–74. PubMed PMID: 18458807.
- Satheesh Nayak. An unusual case of trifurcation of the sciatic nerve. Neuroanatomy. 2006;5:6-7.
- Prakash, Bhardwaj AK, Devi MN, Sridevi NS, Rao PK, Singh G. Sciatic nerve division: a cadaver study in the Indian population and review of literature. Singapore Med J. 2010;51(9): 721–23. PubMed PMID: 20938613.
- Gabrielli C, Olave E, Mandiola E. Inferior gluteal nerve course associated to the high division of sciatic nerve. Rev Clin Anat. 1997;15:79-83.
- Ugrenović S, Jovanović I, Krstić V, Stojanović V, Vasović L, Antić S, et al. The level of the sciatic nerve division and its relations to the piriform muscle. Vojnosanit Pregl. 2005;62(1):45-9. PubMed PMID: 15715349.
- Pokorny D, Jahoda D, Veigl D, Pinskerova V, Sosna A. Topographic variations of the relationship of the sciatic nerve and the piriformis muscle and its relevance to palsy after total hip arthroplasty. Surg Radiol Anat. 2006; 28(1):88–91. PubMed PMID: 16311716.
- Ogeng'o JA, El-Busaidy H, Mwika PM, Khanbhai MM, Munguti J. Variant anatomy of Sciatic nerve in a black Kenyan population. Folia Morphol. 2011 Aug;70(3):175–79. PubMed P MID: 21866528.
- Sabnis AS. Anatomical Variations of Sciatic Nerve Bifurcation in Human Cadavers. Journal of Clinical Research Letters. 3(2):46-48.
- Mallikarjun Adibatti, Sangeetha V. Study on Variant Anatomy of Sciatic Nerve. J Clin Diagn Res. 2014 Aug; 8(8):07-09. PubMed Central PMCID: PMC4190700.
- Satyajit S, Samanta C, Paul M, Biswas S, Reshma G, Saktipada P, et al. A Study on the bifurcation of sciatic nerve with its clinical significance. Ind J Basic Appl Med Res. 2015 Jun; 4(3):34-44.
- Dhivya S, Anbusudar K. A study of the bifurcation of sciatic nerve and its clinical importance. Int J Anat Res. 2016 Mar;4(1):1828-1832.
- Naveena S, Shabana S. Patterns of sciatic nerve bifurcation and their clinical relevance. Int J Anat Res. 2017;5(1):3622-3624. DOI: 10.16965/ ijar.2017.123.
- Uluutku M, Kurtoglu Z. Variations of nerves located in deep gluteal region. Okajimas Folia Anat Jpn. 1999 Dec;76(5):273–76.
- Shewale AD, Karambelkar RR, Umarji BN. Study of variations in the divisions, course and termination of the sciatic nerve. JKIMSU. 2013 Jun;2(1): 62-68.