Recession Coverage using Coronally Repositioned Flap with Bioresorbable Collagen Membrane: A Case Report
Kirti Pal1, Priyanka Aggarwal2*, Shweta Bali3, Aruna Nautiyal4
1 Post Graduate Student, Dept. of Periodontics and Oral Implantology, Santosh Dental College, Santosh Deemed to be university, Ghaziabad, India.
2 Professor, Department of Periodontics and Oral Implantology, Santosh Dental College, Santosh Deemed to be university, Ghaziabad, India.
3 Professor and head of department, Department of Periodontics and Oral Implantology, Santosh Dental College, Santosh Deemed to be university,
Ghaziabad, India.
4 Senior Lecturer, Department of Periodontics and Oral Implantology, Santosh Dental College, Santosh Deemed to be university, Ghaziabad, India.
*Corresponding Author
Priyanka Aggarwal,
Professor, Department of Periodontics and Oral Implantology, Santosh Dental College, Santosh Deemed to be university, Ghaziabad, India.
Tel: 09990502323
E-mail:
Received: December 15, 2022; Accepted: April 10, 2023; Published: April 15, 2023
Citation: Kirti Pal, Priyanka Aggarwal, Shweta Bali, Aruna Nautiyal. Recession Coverage using Coronally Repositioned Flap with Bioresorbable Collagen Membrane: A Case Report.
Int J Dentistry Oral Sci. 2023;10(3):5333-5335.
Copyright: Priyanka Aggarwal©2023. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
2.Case Report
3.Discussion
4.Conclusion
5.References
Introduction
In recent years, periodontal therapy, has been increasingly focused
on aesthetic benefits for patients that includes the soft tissue component
in addition to tooth replacement and colour.
According to the description of " It is "surgical modality used to
treat anatomic, developmental, or traumatic defects of the gingiva
and alveolar mucosa." The goal of periodontal plastic surgery is
to replace missing tissue up to the cementoenamel junction and to
restore a natural, healthy gingival sulcus.
The apical displacement of soft tissues from the cementoenamel
junction is known as gingival recession (CEJ). Laterally positioned
flaps, double papillae flaps with or without guided tissue regeneration
(GTR), free gingival autografts, and autogenous subepithelial
connective tissue grafts are among the therapies available. Coronally
advanced flap ( CAF) is one of them.
Miller's Class I and Class II gingival recessions can be treated using
the Coronally Advanced Flap (CAF). It is a predictable mucogingival
surgical technique that achieves root coverage. The
best clinical results in terms of root coverage have been observed
when the gingival edge is positioned at the cementoenamel junction
(CEJ) and the flap is passively fitted to the exposed root surface.
Root prominence, presence of frena, type of periodontium, recession
depth, and vestibular depth are some of the anatomical
factors that may impact the movement of the coronally & advanced
flap towards the CEJ. Norberg [1] was the first to introduce
the coronally Advanced flap, which was later described by
Mutschelknauss and Restrepo1,and other researchers used surgical
techniques to cover denuded roots in cases of marginal periodontitis
by coronal repositioning of mucoperiosteal flaps [1].
GTR-based methods produced comparable clinical results as previous
root covering treatments and resulted in the development
of new attachments. To avoid a second surgical procedure to remove
non-resorbable membranes, resorbable membranes were
chosen over them.
Gingival recession is treated with a range of non-resorbable and
resorbable membranes.
In this case report, root coverage has been done in Class I Miller’s
gingival recession by coronally advanced flap along with collagen
membrane.[2]
Case Report
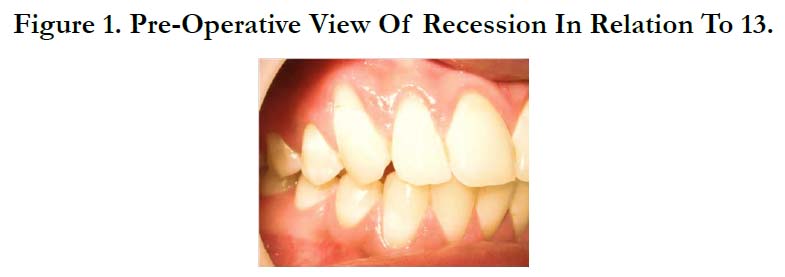
A male patient aged 40-years patient reported to the DEPARTMENT
OF PERIODONTICS AND ORAL IMPLANTOLOGY,
SANTOSH DEEMED TO BE UNIVERSITY GHAZIABAD
with a complaint of receding gums and localised
sensitivity to hot and cold in the upper left anterior tooth region
. The patient was in good health, with no systemic diseases or
bad habits like smoking. The patient was identified with Class I
gingival recession in relation to 13 on clinical examination. In 1st
visit Phase-I therapy was SRP done with Gracey curettes on the
exposed root surface (Hu-Friedy) and recalled after 15 days. The
following surgical operation was carried out after the signing of the informed consent form.[2]
Clinical Procedure
On patient scheduled visit after SRP the Recession depth (RD),
sulcus depth (PD), breadth of keratinized gingiva (KG), and gingival
thickness (GT) were clinical parameters that were collected
to assess the outcome of the patients Keratinized tissue had a
width of 3 mm and a thickness of 1.5 mm. At the interdental papillae
of teeth with the recession, split-thickness horizontal incisions
were made. To measure the thickness of keratinized gingiva
apical to the recession reamer with stopper was used, after the application
of local anesthetic (2 percent lignocaine with adrenaline
(1:2,00,000). On the line angle of distal teeth, two oblique vertical
releasing incisions with beveled edges that extend into the alveolar
mucosa were provided without engaging the neighboring papilla.
The flap was raised in the coronally apical direction using a
split-full-split -thickness technique. At the interdental papilla and
3–4 mm apical to the recession defect partial thickness flap was
reflected . To generate vascular beds for the CAF surgical papilla,
the facial interdental papilla was de-epithelized coronal to the horizontal
incisions. Curettes were used to instrument the root surface,
root conditioning was done using tetracycline solution (125
mg tetracycline/mL saline). To removes the smear layer, provide
antibiotic coating, inhibit collagenase and promotes the formation
of type I collagen. After conditioning, root surfaces were
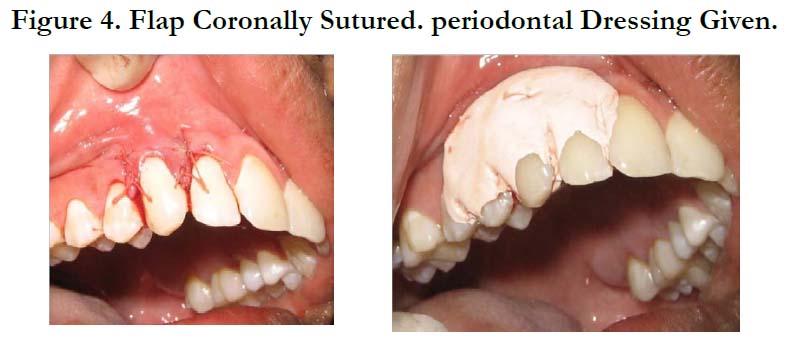
washed with normal saline and air-dried. The collagen membrane
was sutured to the root surface and surrounding. the reflected
flap was coronally reposition 1 mm coronal to the CEJ. vertical
incisions were closed with interrupted sutures using 3-0 Vicryl
sutures and sling sutures were used at the interdental papillae. Because
the superficial releasing incision retains enough blood supply,
it was used to relieve the lip pull on the gingiva. After the Coe
pack was placed on the surgical site. [4, 5]
Post-Operative Care
Post op patients was adviced to use mouth rinse containing 0.12 percent chlorhexidine gluconate for two weeks. Patients were administered
systemic antibiotics (Augmentin 625 twice daily for
three days) and told to follow normal postoperative periodontal
mucogingival guidelines, including not tugging on their lips to inspect
the surgery site. At baseline, one month, and three months,
clinical data such as recession length and width were recorded.[3]
Clinical Observation
The result showed a significant reduction in length and width of
recession with the use of the collagen membrane 3 months postoperatively,
there was a reduction in recession length, recession
width, and clinical attachment level gain. The width of keratinized
gingiva was also found to be increased, the patient was extremely
satisfied with the final clinical outcome and appearance.[2]
Discussion
The collagen membrane closely resembles the foundation membrane
of human mucosa, which aids gingival cell attachment.
It offers numerous therapeutic benefits, including good handling
qualities, reduced operatory time since it does not require a second
surgical site, the availability of an endless amount of uniformly
thick barrier material, and postoperative maintenance. As compare
to healing by long junctional epithelium more stable the natural
attachment is produce by GTR-based root covering.4.Collagen is
the most abundant structural protein in the connective tissues of
the body. Collagen helixes are made up of amino acids linked together
to create a triple helix of elongated fibrils that are primarily
seen in fibrous tissue. The coronally advanced flap can treat Miller
Class I and II recession with excellent consistency and stability.
The findings of this technique demonstrate that collagen membrane
can be used along with coronally advanced flap to treated
gingival recession and further increasing the thickness of keratinized
gingiva also.
Conclusion
The current findings indicate that combination of CAF and collagen
membrane is a predictable therapeutic option for treating
gingival recessions.[4]
References
-
[1]. Sharma A, Wadhawan A, Joshi CS, Kaushik M. Coronally advanced flap
design in management of isolated gingival recession: A case series. Int J
Appl Dent Sci.2021;7:382-7.
[2]. Mishra P, Dhruvakumar D. Recession coverage using coronally advanced flap with Pericardium® membrane (collagen Type I)-A case report. JAdv- ClinRes Insights. 2018 Nov 1;5(6):203-6.
[3]. Singh P, Thakral R, Kaur M, Narula T. Combination of platelet rich fibrin membrane with coronally advanced flap in treatment of gingival recession: A case report. Int J Res Health Allied Sci. 2016;2:35-9.
[4]. Mahajan R. Prucalopride: A Recently Approved Drug by the Food and Drug Administration for Chronic Idiopathic Constipation. Int J Appl Basic Med Res. 2019 Jan-Mar;9(1):1-2. PubMed PMID: 30820411.
[5]. Mishra D, Kalapurakkal VB, Misra SR. Improving Gingival Aesthetics Using Platelet Rich Fibrin and Synthetic Collagen Membrane: A Report of Two Cases. J ClinDiagn Res. 2015 Oct;9(10):ZD01-4. PubMed PMID: 26557624.