Exploring the Experiences of Dentists During Dental Visits of Patients with ASD
Kim Danella Erna Go Santos1*, Jasper Vincent Q.Alontaga1*
1 Educational Leadership and Management Department, DeLaSalle University, Manila, Philippines.
*Corresponding Author
Kim Danella Erna Go Santos and Jasper Vincent Q.Alontaga,
Educational Leadership and Management Department, DeLaSalle University, Manila, Philippines.
E-mail: Philippineskimdanella19@gmail.com / Philippinesjasper.alontaga@dlsu.edu.ph
Received: December 17, 2022; Accepted: January 15, 2023; Published: February 27, 2023
Citation: Kim Danella Erna Go Santos and Jasper Vincent Q.Alontaga. Exploring the Experiences of Dentists During Dental Visits of Patients with ASD. Int J Dentistry Oral Sci.
2023;10(1):5315-5323.
Copyright: Kim Danella Erna Go Santos and Jasper Vincent Q.Alontaga©2023. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Children with Autism Spectrum Disorder may manifest different behaviors during their checkups due to unusual stimuli inside the dental clinic. The dental practitioner and other staff may encounter difficulty anticipating the success of the treatment if both dentist and patient comeunprepared. This study intended to explore the undesirable behaviors of patients with ASD and the challenges encountered through the experiences of dentists. The study used aqualitative casestudy method which was participated in by five (5) dentists through interviews and five (5) patients through observation. First, it was identified that the uncooperativeness of patients withASD was one of the undesirable behaviors manifested during a checkup. Second, carrying out dentaltreatment, handling patients with ASD, communicating with patients, and making patients comfortable add to the difficulty of dentists. Third, the ideal treatment plan will not be implemented if behaviors were not properly addressed.And lastly, receiving training on handling patients with ASD, providing positive behavior support during treatment, and proper scheduling played a significant role in managing the behaviors of the said patients. Hence, it is important to identify the profile of each patient before the start of the treatment so the dentist and his team will be prepared with the necessary management needed. Moreover, preparing the patient with Autism Spectrum Disorder prior to the checkup is significant for managing the child’s expectations of the situation.
2.Case Report
3.Discussion
4.Conclusion
5.References
Keywords
Pediatric Dentistry; ASD; Dentists; Dentalcare; Dental Management.
Introduction
Healthy smiles are essential to children. Maintaining good oral
health for children in a particular group of disabilities known as
Autism Spectrum Disorder is not easy for some. The unique features
of patients with ASD have the possibility to make dental
visits demanding in different ways. The behavior manifestations
of their characteristics having difficulty tolerating changes and
adapting to a new environment can be challenging for dentists
and might affect the success of the dental treatment.
Autism Spectrum Disorder is a neuro developmental disorder and
they are characterized by qualitative impairments in social interactions,
absent or impaired language and communication skills, and
present with a wide range of stereo typed, repetitive behaviors [1].
The word Autism is derived from the Greek word “autos,” which
means self, and “ismos,” which means a state of self-absorbed to
the exclusion of everyone around them [2]. Diagnosis of ASD is
currently based on two areas: (A) persistent difficulties in social
communication and social interaction across multiple areas of
daily living, (B) restricted and repetitive behaviors and interests
[3]. The cause of ASD is still unknown even if there are numerous
research about the said condition, but there are links related to
it such as genetics, environmental factors, and medical problems.
Children with Autism have multiple medical and behavioral problems,
which make their dental treatment extremely difficult [4].
Based on the study conducted by Stein [5], stereo typical and repetitive
actions can also complicate dentists’ ability to safely and
effectively provide dental care. Children with ASD can be come
agitated by over stimulation from many people touching them,
and from loud noises and smells in their environment [6]. Children
visit their dentist equipped with a learned set of behaviors that have successfully helped them to cope with other difficul
to ranxiety- inducing situations, and they will naturally use these
coping strategies in the dental setting [7]. They pose the greatest
challenge for dentists, due to their complex and varied clinical
manifestations [8]. Another challenge to oral care practitioners
is the decreased ability of patients with ASD to communicate
and respond to others, particularly to unfamiliar persons. Lack of
communication can be a problem if the patient is in articulate to
express his fears, pain,or emotions. Certainly, if a child’s behavior
in the dental surgery/office cannot be managed then it is not easy
if not unworkable to holdout any dental care that is needed [9].
The dentist must be in control of the different stimuli that may
trigger a range of behaviors in patients with ASD during the
check-up. They should also recognize that the dental managementof
each individual with a disorder is uniquely different from
other patients, especially from thosewho are typically developing.
Among children with ASD, sensory sensitivities were associatedwith
oral care difficulties in the home and dental office, and with
behavioral difficulties in the dental office [5].
Patients with Autism Spectrum Disorder may have difficulty understanding
the people and the things happening around them especially
if the situation is unprecedented. The said disorder ischallenging
for a health careprovider to diagnose and treat. Dentists
don’t need to become experts, but being aware of the common
behaviors and challenges that may trigger during dental checkups,
and how to adapt to them will be significant in improving the
dental care to be received by patients with ASD.
Materials And Methods
This study documented the experiences of dentists with their
patients with ASD during dental visits. The researcher identified
the different behaviors manifested by patients with ASD and the
difficulties that dental practitioners experience when treating the
said patients. This study was guided by the following researchquestions:
1. What are the undesirable behaviors of patients with ASD during
a dental checkup?
2. What are the difficulties encountered by dentists to patients
with ASD during a dental checkup?
3. How do undesirable behaviors affect the success of dental
treatment?
4. How do dentists address these difficulties?
Methodology
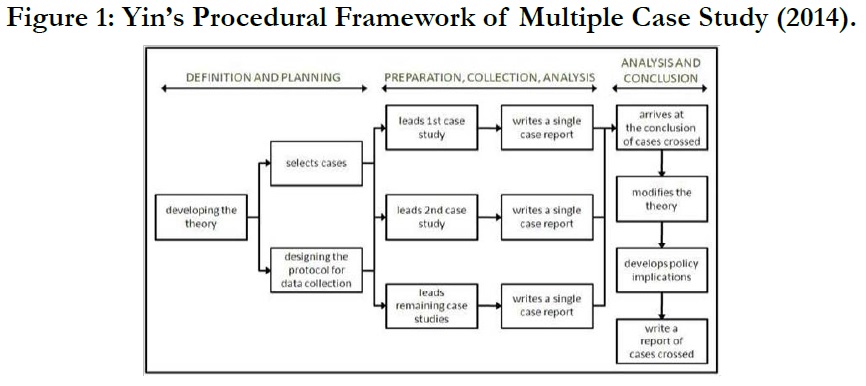
This study employed the research design based on Robert K. Yin’s
Case Study Research Design and Methods. It was used since the
researcher has little or no control over behavioral events and was
focused on the actual situation of the dentists’ experiences. The
case study methodology by Yin [10] that this study followed has
six interconnected steps; plan, design, prepare, collect, analyze,
and share. It was reiterated that the case study research is linear
and progressing, at the same time, following an iterative development.
The researcher applied in this study the method illustrated
in Figure 1 to examine the current experiences of dentists during
dental visits of their patients with ASD.
Research Respondents
This study was conducted in five (5) private dental clinics in Metro
Manila, Philippines that cater to patients with ASD. The research
respondents were composed of five (5) dentists who werecurrently
practicing and treating patients with ASD. The researcher
chose respondents who have experience in providing and receiving
dental care. The results were derived from the answers of the
dentists through a one-time interview and direct observations of
their patients.
Data Collection and Analysis
The researcher engaged in gathering information by conducting a
face-to-face interview with the dentist and doing a one-time observation
with patients with ASD in their respective clinics using
an observation guide.
The data obtained were tabulated and analyzed by going through
all of the text and labeling words, phrases, and sections of text to
search for patterns. The codes were arranged together to form
categories and to develop emerging themes percase. Each of
the themes created was then matched to the research question is
answered. It alsoincluded the related literature about the theme,
excerpts from the dentist’s interview, and the observation notes
made by the researcher to support the data gathered based on the
interview.
Results and Discussion
Research Question 1: What are the undesirable behaviors of
patients with ASD during a dental checkup?
Uncooperativeness in the Dental Clinic: Dental Clinic is an
organization that is responsible for providing health medication
and treatment for all types of dental patients [11]. One common theme that emerged for research question1 was Uncooperativeness
in the dental clinic. It was evident in all cases that being uncooperative
was observed and experienced by the interviewed dentists
themselves during dental visits of patients with ASD. These
were exhibited through non-compliance suchas refusal to enter
the clinic, refusal to sit on the dental chair, and refusal to follow
instructions.
Refusal to enter the clinic. Dentist C expressed during the interview
that some of her patients display uncooperativeness inthe
dental clinic by refusing to enter the clinic. As she said:
“Based on my experience, some of them do not want to come inside our clinic.
Their parents would report that on the way herein the clinic, their child will
complain in the car… It seems like it’s automatic for them to resist when coming
in or entering the treatment room.”
Dentist B also reiterated that “Other kids donot want to enterour clinic
or usually they comehere crying.” Most patients come with a set of
behaviors that manifest during an unlikely, unknown, orunfamiliar
situation such asgoing to the dentist. Some patients may
come prepared but on the day of the checkup, they may feel overwhelmed
or frightened by the actuals cenario. Fearful pediatric patients
often refused to sit in the dental chair or open their mouths
for oral examination [12]. Information on the origin of dental fear
and uncooperative behavior in a child patient before the treatment
procedures may help the pediatric dentist plan appropriate
behavior management and treatment strategy [13].
Dentist A cited a similar observation as to what Dentists B and C
experienced in their clinics:
“..Sometimes some patients with ASD do not want to enter the clinic just
like the patient you observed. His parents are very patient in coming here and
talking or explaining to us coz Patient A is nonverbal.”
As observed by the researcher, the parents of Patient A negotiated
with their child to enter the clinic by bribing him with the
food they bought from the latter’s favorite fast food chain. The
spaghetti should be the reward of the patient after the treatment
butthey used it as a bribe for him to come inside the room.
Refusal to sit on the dental chair. Another demonstration of a
patient being uncooperative was the refusal to sit on the dental
chair. Based on the study of Hernandez and Ikkanda [14], sitting
skills are the foundation for developing other skills required for
in-office treatments. This is one of the prerequisite skills needed
to learn by patients with ASD since dental procedures require patients
to sit on the dental chair. Dentists A and B shared that they
encountered patients who do not want to sit on the dental chair
and does not want to cooperate with them. Dentist D also cameacross
the same situation in her clinic as she recalled:
“Well I experienced patients who donot want to sit on the dental chair, donot
want to say “ah”, do not like the tools, the taste of the fluoride..”
As observed by the researcher, he did not want to sit on the dental
chair and kept hiding behindthe dentist’s back. Dentist C gave a
reminder to Patient C by saying, “last 10 counts standing and you need
to sit on the chair.” The patient eventually followed right after the
instruction and sat on the dental chair.
Johnson & Rodriguez [6] said in their study that challenging behaviors
are a child’s way of communicating their frustration when
their routine is interrupted. Aside from the refusal to enter the
clinic and sit on the dental chair, some patients with ASD exhibit
uncooperativeness in the dental clinic by not following the instructions
given bythe dentist. Dentist A disclosed:
“They may show lack of cooperation, tension, and unwillingness to accept
treatment. They don’t want to follow us or our instructions when we instruct
them to sit down or open their mouth, just like I said earlier there’s this one
patient whom I’ll really not forget,ever. That he intentionally chooses to keep
his mouthclosed.”
Refusal to follow instructions. Aside from displaying uncooperative
behaviors as a reaction due to dental stimuli factors experienced
inside the clinic, some patients also intentionally oppose
following the instructions of the dentist. Dentist As hared another
similar incident:
“One time, a patient pulled the dental suction tube because he doesn’t want to
cooperate. Another patient took the dental mirror and threw it away. Then
they will just laugh after. Very challenging right? Or sometimes they intentionally
don’t open their mouth.”
Dentist C like wise reported during her interview:
“I also experienced a kid who does not follow any of my instructions like
when I say “sitwell” or “please open your mouth”, as in he’s really not following.”
According to Johnson & Rodriguez [6], non-compliance extends
to emotional out bursts and temper tantrums or behavioral outbursts
when children with ASD are asked to comply with instructions
related to their health careand hospitalcare.
Aggressive Behaviors: The unique theme that emerged for research
question 1 was Aggressive Behaviors. This theme emerged
based on the answers of Dentist A. She stated, “There was a time
that a patient bit mythumb. Then after that, as if nothing happened.” Challenging
behaviors exhibited by children with ASD in the healthcare
setting, often a result of boredom, anxiety, or fear, may includes
creaming, crying, tantrums, aggression, apathy, and lack of
cooperation with providers [15]. A patient with ASD tends to be
aggressive when triggered by stressful or uncertain situations. It
can be their means of coping with the demanding environment
or it can be their way of communicating that they are in adifficult
situation.The cause of such behaviors is unknown, but it maybe a
source of self-stimulation for these children, and it is more commonly
seen in nonverbal children with impaired cognitive functioning
and altered sensory processing [16].
Behaviors Associated with the Past: Another unique theme was
Behaviors associated with the past. This theme emerged based on
the answers of Dentist B. She clarified that some patients exhibit
undesirable behaviors because they had a negative experience during
their past dental visits. She said, “Well some are curious, someare
excited, some are crying maybe because they have a negative experience in the
past.” Based on the study of Appukuttan [17], dental anxiety can
arise due to multiple factors such as previous negative or traumatic
experiences, vicarious learning from anxious family members
or peers, individual personality characteristics such as neuroticism
and self-consciousness, lackof understanding, exposure to frightening portrayals of dentists in the media, the coping style of the
person, perception of body image, and the vulnerable position of
lying back in a dental chair.
Research Question 2: What are the difficulties encountered
by dentists to patients with ASD during a dental checkup?
Carrying Out Dental Procedure: There was no common theme
that emerged from all the dentists for research question 2. None
the less, the theme Carrying Out Dental Procedure was evident in
4 dentists that includes DentistsA, B, C, and E.
Dentists may encounter difficulty in pushing through with the
services they need to provide their patients because they are associated
with causing pain and discomfort to them. Dentist E
somehow expects difficulties in carrying outdental treatment. As
she quoted,
“..Opening their mouth then someone will put tools inside is also not part of
their everyday life that is why we understand when they react differently during
the treatment.”
The feeling of uneasiness comes in when dentists put tools inside
a patient’s mouth. As stated by Dentist B,
“But most of them do not want tools inside their mouth. Maybe because they
are notused to it. Sometimes they complain because they can’t tolerate the tools
in their mouths. Or they are already tired of opening their mouth or they cannot
sustain opening their mouth for the whole time.”
Dentist A also shared the same thoughts during her interview.
She said:
“Some patients can’t tolerate the procedure and they don’t like the tools inside
their mouth… It is difficult on our part because we can’t force them to open
their mouth.”
During dental treatment, dentists may require not only one but
sometimes two or more tools to be put inside the patient’s mouth.
Aside from these, they are also required to sustain their mouth
open for the duration of the procedure. Dentist Badded, “It is also
difficult to let them open their mouth then sustain for the whole time so we need
to be quick in treating them.” Thus, it will be difficult for dentists to
proceed with the treatment if their patients cannot perform both
of these skills. Furthermore, a child’s dental practitioner and their
team cannot force the child to open their mouth and needs to
wait for the patient to be ready. Certainly, if a child’s behavior in
the dental surgery/office cannot be managed then it is not easy if
not unwork able to holdout any dental care that is needed [9]. As
observed with Patient B, she was able to tolerate the tools inside
her mouth with proper guidance from the dentist.
Dental instruments such as mouth mirrors, explorers, excavators,
cotton pliers, and saliva ejectors are common tools that patients
will encounter during dental treatment. As per Dentist C, even
typically developing children have a difficult time opening their
mouths and sustaining them open since they are easily tired. As
she explained:
“Some of them have difficulty opening their mouth. They easily
feel tired of opening their mouths. Those difficulties are understandable.
Some kids even those without special needs, have a
hard time tolerating the tools in their mouths. May be a factor to
consider is that their mouth is small and ofcourse they are kids.
There are things that we cannot push them to do especially if they
don’t understand yet the importance of oral health care.”
It was seen in Patient At hat he had difficulty sustaining his mouth
open. Understandably, children cannot tolerate more than one
tool because their mouth is small and some have mouth and motor
limitations.
Getting Patient Settled: The unique theme that emerged was
Getting Patient Settled. This theme emerged from the answers of
Dentist D. It was observed that Dentist D had difficulty getting
Patient D settled because of the movements he exhibited during
the treatment. Movements such as crying, kicking, and removing
the hands of the assistant dentist were noted during the treatment.
As she disclosed during the interview:
“They exhibit repetitive movements or those stimulatory behaviors, some repeat
what they just heard from the TV or echo, and they will not forget it.
Some have usual routines that cannot be interrupted. Difficulty tolerating
changes in their usual routine or schedule.”
It is possible that these behaviors were manifested due to the
change in the usual schedule of the patient. Based on the study
conducted by Stein [5], stereotypical and repetitive actions can
also complicate dentists’ ability to safely and effectively provide
dental care.
Based on observation, Patient C kept on whining and crying during
the initial part of the treatment. The intensity of his behavior
was minimized when the doctor provided continuous verbal
praise and continued talking with the patient. The dentist was explaining
what she was doing and tries to redirect the attention of
the child by constantly reminding him that he was doing great. To
wards the end of the treatment, the patient was relaxed and did
not exhibit any behaviors anymore and the medicine took effect
already.
Research Question 3: How do undesirable behaviors affect
the success of dental treatment?
Ideal Treatment Plan Not Executed: The common theme that
emerged in research question 3 was I deal Treatment Plan Not
Executed. The dentist’s failure to do the required treatment may
compromise the service that the patient needs to receive especially
if it is urgently needed. All the dentist participants identified
that undesirable behaviors of patients with ASD hinder the positive
outcome of dental treatment. Further more, it can also cause
disorders in the clinic and other patients may be affected as well.
According to Dentist B:
“If the child has a difficult behavior, there’s a possibility that it will hinder
the procedure. It may require more adjustments from the end of the dentist
and staff and it may cause disorder in the clinic.”
Dentist A also pointed out: “Sometimes it impedes the success of the
treatment. Because instead of having acontinuous treatment, we need to pause
to manage behavior or we wait for the child to calm down.”
Individuals with ASD often have problematic behavior patterns
that create challenges for dentists when delivering routine oral healthcare [14]. Therefore, effective treatment cannot be performed.
It was also quite similar to the response of Dentist D,
as she shared:
“Of course, one patient is different from the other but they have a characteristic
which may be reactive and might hinder the success of dental treatment.
Usually, these characteristics might reflect in their behaviors. Effective treatment
cannot be performed.”
Dentists might not be able to continue with the treatment plan
intended for the patient if behaviors continue to arise during the
checkup. Pushing through with the dental treatment even if the
patient with ASD is already exhibiting a tantrum might also create
a negative memory for the child and may result in a bad experience
that can affect future dental visits. Dentist C imparted:
“If a patient exhibits tantrum, there is a tendency that we’ll have difficulty
making progress with the treatment. There will be delays in providing the care
that the patient needs. I feel bad for the patient. We won’t be able to provide
the service that the child needs if there is a difficult behavior because it really
impedes theprocedure.”
When behaviors arise in the dental clinic, there is a possibility
that the dentist might not be able to progress to the treatment
plan. The treatment will be compromised since the dentist needs
to manage the behavior first. There is a risk of having a negative
experience if the dentist continues with the procedure while the
patient is not yet ready. Dentist E also revealed:
“Somehow it affects successful dental visits by not being able to carry out any
dental care that is needed. Behavior management is really a key factor in
providing dental carefor these particular patients.”
The dentist might need to take some extra effort to progress with
the treatment if the procedures are always impeded or delayed
due to the unexpected behaviors of the patient with ASD.No single
assessment method or tool is completely accurate inpredicting
a patient’s behavior, but awareness of the multiple influences on a
child’s response to care can aid in treatment planning [18].
Oral Health May Be At Risk: The unique theme in research
question 3 was Oral Health may be at risk. This theme emerged
from the answers of Dentist A. There will be delays in providing
immediate care for the patients if behaviors arise during the
checkup. Hence, the oral health of the patient might be compromised.
As Dentist A reiterated:
“Some times if treatment is rescheduled, there’s atendency that the patient will
not come back anymore. So, oral health may be at risk. Especially for kids
who need urgent care. Usually, kids with special needs, or even kids without
disabilities, comehere if there’s a teeth problem or if the conditionis already
worst. So, delays really can cause risks to children.
Although there appear to be no known autistic-specific oral manifestations,
oral problems might arise because of autism-related
behaviors such as communication limitations, personal neglect,
effects of medications, self-injurious behaviors, dietary habits,
resistance to receiving dentalcare, hyposensitivity to pain, and
possible avoidance of social contact [19]. Considering the delays
that will happen when an ideal treatment plan is not executed and
given right away, there is a possibility that the oral health of the
patient might be exposed to possible or further damage. Thus,
children with Autism Spectrum Disorder are at high risk fororal
disease [5].
Research Question 4: How do dentists address these difficulties?
The themes under research question 4 were the strategies that
were seen as effective by the interviewed dentists in their current
practice. The three common themes that emerged in this research
question were Positive Behavior Support, Scheduling, and Professional
Training and Experiences.
Positive Behavior Support: The first common theme was Positive
Behavior Support. The establishment of a good relationship
between the dentist and the child has been shown to increase the
success of treatment in terms of the child’s cooperation during
the treatment or advice for prevention [20]. In special education,
positive behavior support is a general term that refers to the application
of positive behavioral interventions and systems to achieve
socially important behavior change [21].
Positive Approach. All dentists that were observed by the researcher
used a calm and gentle tone of voice during the treatment
of their patients. Being able to do so, they were able to set
a warm and encouraging atmosphere inside their clinic. As Dentist
B cited, “I also play with them using some of our tools like the tooth
brush,sing songs.” Dentist A also expressed that she loves kids and
that using agentle tone of words minimizes their stress:
“May be because I love kids. Very helpful if the patient sees you regulated,
you co-regulate, using soft and gentle words, it will relax them. It is also
important to play withour patients eh, because it decreases their stress and
anxiety.”
Dentist Clikewise mentioned,“Talking to them and having a calming
voice also makes them feel safe, comfortable, and relaxed.” The dentist’s
attitude, body language, and communication skills are critical to
creating a positive dental visit for the child and gaining trust from
the child and parent [18]. It is significant to establish rapport to
gain the trust and confidence of the patient with his dental care
provider. Hence, creating a dentist-and-patient healthy relationship
ensures safety during the treatment. Dentist A added to herstatement:
“We need to establish rapport with the patient before doing the procedure. We
engage in small talks or we play with them. As a dentist, we need to make the
patient feel at ease or comfortable with us.”
Children who have positive interactions with their dentist will be
more likely to visit the dentist and will have better dental health
[20]. Dentist Esaid, “That is why we always strive to make everydental
visit a fun experience for them so they’ll associate us with something happy and
fun.” She also allowed the child to choose the color of the toothbrush
and the flavor of the toothpaste thatthey used (choices arebanana,
strawberry, and milk).
Positive Reinforcement. Positive reinforcement is an effective
technique to reward desired behaviors and thus strengthens the
recurrence of those behaviors [17]. It was common to all the observed
dentists that they used social reinforcers and verbal praises
such as “GoodJob” or “Verygood”. In addition to that, they also
used other reinforcers that were appropriate to the profile of their patients. As per Dentist D, she provides “..praises, rewards, and our
approach with them were just gentle.” Dentist C as well reiterated:
“At the end of the treatment, we give stickers to the child as their token or
reward for doing well. Or sometimes it’s the parents who give their child a
reward such astoy, go to the toy store or sometimes Jolli bee.”
If we reinforce a patient for keeping the mouth open then that
patient is more likely to open the mouth again, and therefore lesslikely
to refuse to open the mouth [7]. Dentist A shared during the
interview the importance of providing verbal praises:
“Continuous praises are also given ‘verygood’ or ‘good job opening mouth’.
They respond positively when they are given continuous praise. Maybe it boosts
their confidence as well. Then after the procedure, they’ ll choose their reward.
We have a canister with different items like ball, bubbles, stickers then the
child will pickone as his reward. And they’re happy. For other kids, the
thought of standing and leaving the room is already the reward for them.”
Aside from reinforcing the patient, it was also observed that
parents too prepare a reward for their child after the treatment.
The parents of Patient B gave her favorite stuffed toy after she
finished her treatment. As observed, Dentists B and E provided
continuous verbal praises to their patient for the duration of thet
reatment.
Tell-Show-Do. Dentist B mentioned another way to provide
support to her patients, “I usually present the tools that we will beusing.
Mostly, they enjoy the different colors of the brush that I use during the treatment.”
In Tell-Show-Do procedures, the provider describes and
models the procedure before treatment [14].
Scheduling: The next common theme was Scheduling. Scheduling
contributes asignificant role in providing a positive dental experience
for patients with ASD. Predictable schedules and forms
of behavior therapy are effective strategies for preventing challenging
behaviors [6]. The dental practice mustensure that the
schedule is organized to accommodate the goals and procedures
needed for each patient. Dentist E brought up:
“We are more considerate with regards to their appointment and time. We
schedule them first thing in the morning or the afternoon so thereare few people
in the clinic. Usually, we can identify the profile of the child. So, if they
confirmed their slots, we allot 1 hour for them for the treatment. Just in case
there will be a next patient, they will not wait that long.”
Early Morning Schedule. According to the study of Dougall
and Fiske [22], minimizing waiting times, by giving the first or
last appointment of the day, reduces stress. Dentist B specified
that they are lenient in providing a schedule to their clients. She
usually schedules patients that require more familiarization and
adjustments in an early morning schedule so that there will be
minimal distractions from other patients. It is also the time of the
day where in their clinic has lesser patients. Waiting can increase
anxiety, which can lead to feelings of anger and unwillingness to
cooperate [23]. As she mentioned, “We usually schedule them early in
the morning so there are few peoplein the area and they won’t be distracted
with other people or patients.” Dentist B also shared that few clients
opt to have their treatment done in the morning especially on a
weekend, just like the parents of Patient B who scheduled their
daughter as early as 8:00 am.
It was also seen during the observation of the researcher with
Dentist D, Patient D arrived around 7:30 a min the dental clinic
together with his parents. The patient was scheduled to be admin
is tered an oral sedative drug which is why they came 30 minutes
earlier than the expected schedule of the clinic. Dentist D pointed
out:
“We also schedule the matan earlier time just like with Patient D so that
there are no other patients since we need to wait for the medicine to take effect.
Usually around 15-20 minutes.”
Longer Treatment Time. Some patients were also given the
early morning schedule so that the dentist can provide a longer
treatment time with them. Getting the early morning slot allows-
Dentist B to maximize her time just in case a patient throws a fit
or any unexpected behavior. She sees to it that there is no next
patient in the queue. As she quoted, “I wait for them to relax so that
our dental treatment will be successful and she’ll recall a positive experience
here with us in theclinic.” She also added, “Plus, we can take our time
during the treatment just in case unexpectedbehaviors arise.” On the other
hand, Dentist D reiterated:
“Scheduling them super early in the morning or late in the after noon will also
give longer treatment time for the patient. We don’t need to get hurry if there
is a next patient waiting.”
Dentist A almost said the same statement as Dentist D:
“We schedule them at their convenient time and we make sure that there is
non extpatient in the cue. So we can take our time in treating them and no
next patient will be affected if we extend our time.”
For patients with special needs, it is important to accommodate
them at a certain time of the day with no next patient in the cue or
on a longer treatment time so the dentist can concentrate well and
take her time with the procedure. It will also be helpful if the said
patients will be scheduled at a time of the day where in there are
fewer patients just like what Dentist B shared so that the patient
will not be distracted by the people in the clinic and avoid unnecessary
behaviors that may arise due to waiting time. Because of
the limited attention span of ASD patients, short, well-organized
appointments should be planned and the waiting time should not
exceed 10-15 minutes to avoid upsets [8].
Pause Treatment. It is significant for patients with ASD to be
ready until they become comfortable and at ease with an unfamiliar
place. With that, they will be able to remember that the dental
environment is not as stressful as they think. Dentist B said, “If
kids are crying, I don’t normally continue with the treatment or push them to
comply.” They usually pause the treatment so it will not be stressful
for the patient and the parents and the dental practitioners as well.
Reschedule Treatment. If there are cases where in the child
throws a fit and the dentist decides to discontinue the treatment,
the patient will be scheduled for another appointment. Dentist B
discussed,
“With that, we reschedule on another day so it won’t be difficult for the child
and they won’t associate us with something negative here in the clinic. Better
if theyleaveour clinic happyright?”
She also mentioned, “And just like what I have said earlier, we are lenient,
if the child starts tothrow a fit, then, we can reschedule him on a different
day or time.” Whenever they encounter a patient that is not ready
for treatment and does not respond to the strategies that are presented,
the staff reschedules them on a different day based on the
availability of the dentist.
According to Dentist C, "So if that’s the case, we just reschedule them
and they don’t need to pay.” It will be stressful for the patient and
dentist as well to resume the treatment if the behavior is notaddressed
properly. Dentist C also added:
“Like what I mentioned earlier, we are lenient with regards to accommodation
and scheduling… That is why when we have special needs patients, we
schedule them super early in the morning or last patient in the afternoon or
any time or day withless patients.”
For Dentist C, scheduling a patient with special needs during offpeak
hours maximizes their time for the treatment and allows
them to provide all the necessary dental care needed by the patient.
As Chandrashekhar and Bommangoudar [2] cited in their
study, the dental team should be organized for changeable and a
typical responses to sensory stimuli, as these patients dislike even
minute changes in their surroundings and requireres emblance in
continuity.
Professional Training and Experiences
Another common theme was Professional Training and Experiences.
The dentists interviewed by the researcher mostly knew
about treating patients with special needs. General dental practitioners
should be aware of the criterion for the diagnosis of ASD
and the depth and complexity of the disorder [3]. They were able
to get familiarized with it from lectures during their undergraduate
course. As Dentist B quoted, “Usually it comes with pediatric dentistry,
the healthcare for special needs.” The same goes for Dentist C:
“We didn’t get a chance to have hands-on training in treating patients with
ASD inparticular. It was just a topic in one of our subjects in college.
Through the years of experience, I just learned managing behaviors from
different professionals and ofcourse from the parents.”
As per Dentist A, “I usually attend training forself-improvement andask
professionals or parents on how to handle behavior.” Moreover, she added:
“We had pediatric dentistry subjects and cases before. But practically speaking
itwas mostly concentrated on treating pediatric patients. We were taught
throughlectures on how to treat patients with special needs, but of course,
lectures are notenough. Experience is the best teacher. I really learned a lot
from my experiences.My patients are actually training me. I am also learning
a lot from parents whentheytell their stories.”
Dentist D also shared that she has a 5-year-old niece who has a
speech and language disorder which is why treating children with
special needs is somehow familiar to her. According to Roberts et
al. [7], it is important that the knowledge and practice of behavior
management should be incorporated into a continuous learning
process or education for all pediatric dentists. Among the interviewed
dentist, only Dentist E had a continuing education abroad
after her undergraduate degree where in she was taught and
trained to handle patients with special needs, particularly those
with ASD. Their clinic here in Manila concentrates on pediatric
and special needs patients andoffers a variety of services at a very
affordable cost. She also added that her team trains otherdentiststo
be knowledgeable and equipped intreating patients with
special needs.
Aside from the dentist her self being trained, it is also important
that the employees in the clinicare knowledgeable in dealing with
patients with special needs. Dentist C’s dental staff and colleagues
are receptive to training, accommodating, and treating the said
patients. As she cited, “Our staff and other dentists here inthe clinic are
also willing to learn more about them, especially those with Autism.” Based
on the study of Robertsetal.[7], the dental team as a whole, including
all auxiliary personnel, should be trained in the knowledge
and practice of the various techniques, so that all children may
becared for to the highest possible standards.
Protective Stabilization: The unique theme in research question
4 was Protective Stabilization. This theme emerged from the answers
of Dentist D. The broad definition of protective stabilization
is the restriction of apatient’s freedom of movement, with
or without the patient’s permission, to decrease the risk of injury
while allowing safe completion of treatment [18].
According to Dentist D, “For patients who have the tendency to
remove our hands from their mouth, we use papoose board so
their hands are on the side only.” Before the procedure, it was
also observed by the researcher that the dental staff used a papoose
board to wrap around Patient D to limit the patient’s body
movements and to make him steady during the dental process.
Theboard helped stabilize Patient D’s body and minimize unnecessary
movements since he started crying, kicking, and removing
the hand ofthe dentist.
Self-Regulation: Another unique theme was Self- Regulation.
This theme emerged from the answers of Dentist A.Dentists especially
those who handle pediatric cases and patients with special
needs are prone to experience undesirable behaviors suchas
whining, shouting, crying, and a variety of other inappropriate
behaviors. These manifestations of behaviors of the said patients
may cause stressto the dentist and might affect how they think,
act, and manage their emotions during dental treatment. Self-
Regulation is a dentist’s way of coping with the said difficulties
encountered in the dental clinic. Farokh-Gisour & Hatamv and
[24] discussed that these conditions cause dentists tobe irritable
or make them nervous since they have to spend energy to stop
them and adapt to such behaviors. Thus, dentists need to be careful
with their thoughts and actions to manage their unexpected
impulses or reactions to how they feel toward their patients. As
expressed by Dentist A:
“Of course, my inner self is kind of impatient and wants to get angry but
I can’t,right? Even if I love kids, of course, we also get exhausted at times.
Especially if it’s successive…Ofcourse, I just smiled. Pretending that everything
is okay.”
Dentist A also pointed out, “So sometimes, I also feel tensed because I
am not doing anything to the child.” They should practice self-control
and enhance their ability to stay regulated to manage stressful situations
when their patient starts to exhibit a tantrum. As observed
with Dentist A, she was able to keep herself relaxed and regulated
even if Patient A exhibited undesirable behaviorssuchas refusal to
follow instructions and react with stimulatory behavior. Anticipating the occurrence of unexpected behaviors of patients with
ASD also helps increase a positive dental experience for the patient
and dentist as well.
Parental Intervention: The last unique theme in research
question 4 was Protective Stabilization. This theme emergedfromtheanswers
of Dentist E.
As reported by Dentist E, Patient E was able to tolerate the procedure
and control his behavior after several appointments at the
dental clinic. During his initial visits, the presence of his mom is
needed for the child to cooperate. The support of the parents also
played a significant role since Patient E’s mom consistently brings
him to dental checkups. Dentist E cited:
“Actually, it is the parents who manage their child during the treatment.
Usually, when they cry, parentshelp us out to identify what works best for
their child.”
The parent's presence is used to get the patient’s attention and increase
compliance, decrease negative behaviors, establish appropriate
roles during treatment, provide effective communication
between the dental provider and patient, and provide a positive
dental experience [2].
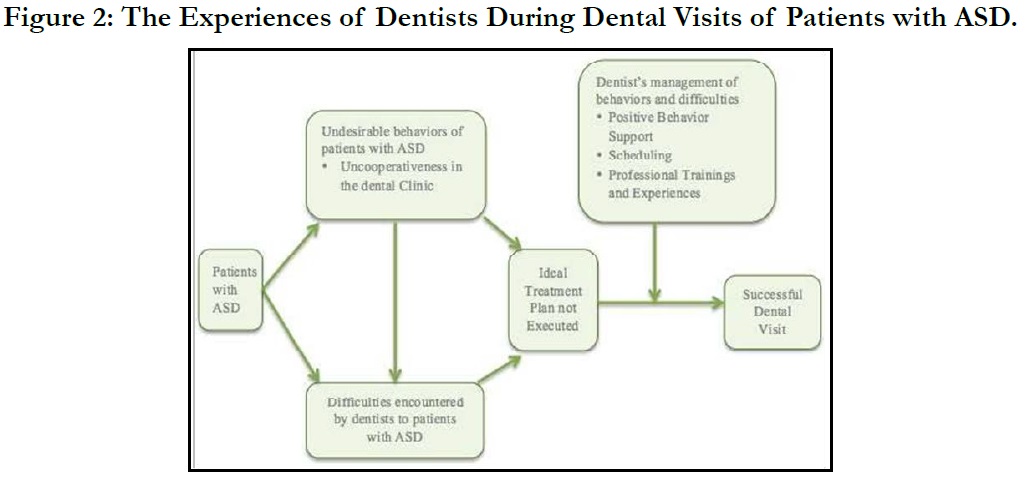
Emerging Framework of the Experiences of Dentists During
Dental Visits of Patients with ASD
Based on the results, Figure 2 illustrates the experiences of dentists
during dental visits of their patients with ASD. The manifestation
of the characteristics and behaviors of the said patients
varies from one person to another. Even if these patients do not
show undesirable behaviors during treatment, it has the potential
to make dental visits challenging for the dental team in a variety
of ways.
Patients with ASD can exhibit undesirable behaviors such as uncooperativeness
when receiving oral care. Most of the patient’s
uncooperative behavior shows a refusal to follow instructions, enter
the clinic, and sit on the dental chair. Inappropriate behaviors
come in when they display inappropriate verbalizations and reactions
during the visit. Throughout the dental checkup, they might
exhibit various reactions suchas crying, whining, or even throwing
at antrum whenever they feel afraid, anxious, or uncomfortable.
It can be their coping strategy with a demanding environment
or it can be their means of communication saying that they are
in a difficult situation. Aggressive behaviors may come in when
unknown or uncertain situations trigger the patient. It was also
revealed that some behaviors were exhibited because the patient
associated them with a negative dental experience in the past.
The undesirable behaviors directly lead to various difficulties that
dentists may encounter intreating patients with ASD. Communicating
with patients can be challenging for dentists due to the
said patients’ reduced ability in expressing their wants and needs.
In somecases, dentists may have a hard time handling a patient
with ASD since the latter were not settled and comfortable inthe
clinic. Dentists might not carry out the dental procedure needed
if undesirable behavior persists. When behaviors are still difficult
to manage, the stress it brings to the dental team might also affect
the decision-making ofthe dental care provider.
There is also an arrow that directly points from patients with
ASD to difficulties encountered by dentists. Even if patients with
ASD do not exhibit undesirable behaviors, there can still be possible
situations where in dentists may encounter difficulty treating
them.
The undesirable behaviors of patients with ASD and the difficulties
of the dentists greatly affect the success of the dental visit.
The primary effect of this leads to an ideal treatment plan not
being executed. All of the said behaviors manifested in the dental
clinic have an effect on the dental team and the treatment plan
intended for the patient. Other effects include being time-consuming
when not treated during the actual visit and the oral health
of the patient willbe at risk.
For a treatment to be successful, dentists should use management
techniques every time they treat the said patients. Aside from
equipping themselves with training, their years of experiencein
their field added an important role in strengthening their skills
in handling patients with ASD. Nonetheless, the use of positive
behavior support and proper scheduling, whenever they treat patients
with ASD played a significant role. Dentists can also accommodate
their patients at their most convenient time and schedule
them during non-peakhours. Familiarizing the patient with the
dental environment before their scheduled appointment, and using
distraction techniques during the treatment helped the patients
have a positive dental visit. In addition, sedation and protective
stabilization techniques were also applicable for patient management
as long as properly administered and with parental consent.
With all these, proper preparation for the patient and the dental
team, and appropriate use of dental management techniques can
achieve a positive dental experience for patients with ASD.
Conclusion
Based on the results of the study, the undesirable behaviors of
patients with ASD were manifested through uncooperativeness
inthe dental clinic, inappropriate behaviors, aggressive behaviors,
unexpected behaviors, and behaviors associated with the past.
The difficulties encountered by the dentists were carrying out
the dental procedures, communicating with patients, handling patients
with ASD, making a patient comfortable, getting the patient
settled, and self-regulation. The ideal treatment plan intended for
the said patients will be affected and the oral health of the patient
maybe at risk if left untreated because of manifested undesirable
behaviors. It will also be time-consuming for both parents and
the dental team to reschedule another visit. Even if there were
behaviors exhibited and challenges experienced by the dentists,
the latter strives to provide apositive and successful dental visit.
The observed dentists were equipped with training on how totreat
patients with ASD. Their experiences in handling different patient
profiles also made them knowledgeable about various techniques
in managing several behaviors. Aside from professional qualifications,
applying positive behavior support, providing accommodation,
giving proper scheduling, allowing patients to get familiarized
with the environment, and using sedation were some of the
helpful strategies that were seen effective in treating patients with
ASD.
It is recommended that dentists motivate parents to pursue regular
dental consultations and to give positive information to their
children about dental checkups before the actual visit. Incorporate
strategies suchas positive behavior support by using a gentle
tone of voice, positive approach, and reinforcements.
For dental clinics, aside from having a small waiting area where
patients can play while waiting, having a television with the child’s
favorite cartoon placed inside the treatment room may be helpful
to distract his attention while the dentist is doing the procedure. It
is also beneficial for patients with ASD to have a prior visit before
their actual dental checkup to get familiarized with the dental environment.
Moreover, it will be helpful if the said patients will be
scheduled during non-peak hours of the clinic so that the dentist
can maximize the time for the treatment.
During the checkup, it is necessary to provide information such
as the possible manifestation ofbehaviors, effective strategies for
management, and reinforcers to the dentist so that the dental
team can also have their preparation. It will be helpful if parents
can assist their children throughout the treatment. Parental presence
may be significant to some patients to decrease their anxiety
and increase compliance.
For the special education teachers and schools, it will be helpful
to include oral care and hygienelessons in classroom discussions
and incorporate the minactual classroom schedules like brushing
teeth after recess or lunch. Students can also have regular visits
to their school clinic to get familiarized with the school dentist
and dental setting. Special education teachers can provide dental
mockups and environment adaptation during their sped sessions
so the students can be accustomed to the routine inside the dental
clinic and the tools that dentists use for their patients.
References
-
[1]. Marti LF. Dietary interventions in children with autism spectrum disorders
- an updated review of the research evidence. CurrClinPharmacol.
2014;9(4):335-49. PubMed PMID: 24050740.
[2]. Chandrashekhar S, S Bommangoudar J. Management of Autistic Patients in Dental Office: A Clinical Update. Int J ClinPediatr Dent. 2018 May- Jun;11(3):219-227. PubMed PMID: 30131645.
[3]. Carter A, Carter G, Georde R.AutismSpectrumDisordersandtheRoleofGeneralDentalPractitioners: A Review.J Dent Appl. 2015;2(7):254-260.
[4]. Jaber MA. Dental caries experience, oral health status and treatment needs of dental patients with autism. J Appl Oral Sci. 2011 May-Jun;19(3):212-7. PubMed PMID: 21625735.
[5]. Stein LI, Polido JC, Mailloux Z, Coleman GG, Cermak SA. Oral care and sensory sensitivities in children with autism spectrum disorders. Spec Care Dentist. 2011 May-Jun;31(3):102-10. PubMed PMID: 21592164.
[6]. Johnson NL, Rodriguez D. Children with autism spectrum disorder at a pediatric hospital: a systematic review of the literature. PediatrNurs. 2013 May-Jun;39(3):131-41. PubMed PMID: 23926752.
[7]. Roberts JF, Curzon ME, Koch G, Martens LC. Review: behaviour management techniques in paediatric dentistry. Eur Arch Paediatr Dent. 2010 Aug;11(4):166-74. PubMed PMID: 20840826.
[8]. J U, M M V, J P, Srinivasan I. Autism Disorder (AD): An Updated Review for Paediatric Dentists. J ClinDiagn Res. 2014 Feb;8(2):275-9. PubMed PMID: 24701555.
[9]. Singh H, Rehman R, Kadtane S, Dalai DR, Jain CD. Techniques for the behaviors management in pediatric dentistry. Int J Sci Stud. 2014 Oct;2(7):269- 72.
[10]. Yin RK. Case study research: Design and methods (applied social research methods). 5thed. Thousand Oaks, CA: Sage publications; 2014.
[11]. Dhanore P, Shaik A, Ramtekkar P. Dental Clinic Management System-A New Approach. IJCSET. 2016 May 1;6(5):176.
[12]. Gao X, Hamzah SH, Yiu CK, McGrath C, King NM. Dental fear and anxiety in children and adolescents: qualitative study using YouTube. J Med Internet Res. PubMed PMID: 23435094.
[13]. Suprabha BS, Rao A, Choudhary S, Shenoy R. Child dental fear and behavior: the role of environmental factors in a hospital cohort. J Indian SocPedodPrev Dent. 2011 Apr-Jun;29(2):95-101. PubMed PMID: 21911945.
[14]. Hernandez P, Ikkanda Z. Applied behavior analysis: behavior management of children with autism spectrum disorders in dental environments. J Am Dent Assoc. 2011 Mar;142(3):281-7. PubMed PMID: 21357862.
[15]. Bultas MW, Johnson NL, Burkett K, Reinhold J. Translating Research to Practice for Children With Autism Spectrum Disorder: Part 2: Behavior Management in Home and Health Care Settings. J Pediatr Health Care. 2016 Jan-Feb;30(1):27-37. PubMed PMID: 26525946.
[16]. Jolly AA. Handle with Care: Top Ten Tips a Nurse Should Know Before Caring For a Hospitalized Child with Autism Spectrum Disorder. PediatrNurs. 2015 Jan-Feb;41(1):11-6, 22. PubMed PMID: 26281270.
[17]. Appukuttan DP. Strategies to manage patients with dental anxiety and dental phobia: literature review. ClinCosmetInvestig Dent. 2016 Mar 10;8:35- 50. PubMed PMID: 27022303.
[18]. Goleman J. Cultural factors affecting behavior guidance and family compliance. Pediatr Dent. 2014 Mar-Apr;36(2):121-7. PubMed PMID: 24717749.
[19]. Nirmala SV. Dental Care and Treatment of Children with Emotional Disorders– An Overview. Autism Open Access. 2016;6(167):2.
[20]. Wali A, Siddiqui TM, Khan R, Batool K. Knowledge, Attitude, and Practices of Dental Surgeons in managing Child Patients. Int J ClinPediatr Dent. 2016 Oct-Dec;9(4):372-378. PubMed PMID: 28127171.
[21]. Sugai G, Horner RH, Dunlap G, Hieneman M, Lewis TJ, Nelson CM, et al. Applying positive behavior support and functional behavioral assessment in schools. J Posit BehavInterv. 2000 Jul;2(3):131-43.
[22]. Dougall A, Fiske J. Access to special care dentistry, part 2. Communication. Br Dent J. 2008 Jul 12;205(1):11-21. PubMed PMID: 18617935.
[23]. Green D, Flanagan D. Understanding the autistic dental patient. Gen Dent. 2008 Mar-Apr;56(2):167-71. PubMed PMID: 18348375.
[24]. Farokh-Gisour E, Hatamvand M. Investigation of Stress Level Among Dentistry Students, General Dentists, and Pediatric Dental Specialists During Performing Pediatric Dentistry in Kerman, Iran, in 2017. Open Dent J. 2018 Sep 28;12:631-637. PubMed PMID: 30369972.