Comparison Of Pharyngeal Space Width In Hyperdivergent Patients With And Without Mouth Breathing - A Cephalometric Study
Anu Rose James, Ajith V.V*, SapnaVarma N.K
Department of Orthodontics and DentofacialOrthopaedics, Amrita VishwaVidyapeetham, Kochi, India.
*Corresponding Author
Dr. Ajith V.V,
Professor, Department of Orthodontics and DentofacialOrthopaedics, Amrita VishwaVidyapeetham, Kochi, India.
E-mail: ajithvv72@gmail.com
Received: October 13, 2021; Accepted: June 14, 2022; Published: June 30, 2022
Citation: Anu Rose James, Ajith V.V, SapnaVarma N.K. Comparison Of Pharyngeal Space Width In Hyperdivergent Patients With And Without Mouth Breathing - A Cephalometric Study. Int J Dentistry Oral Sci. 2022;9(6):5304-5307.
Copyright: Dr. Ajith V.V©2022. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: The importance of respiratory function in orthodontic diagnosis and treatment planning cannot be overstated.
The growth and function of the nasal cavities, nasopharynx, and oropharynx are all associated to appropriate skull growth.
The aim of this study was to compare the pharyngeal space width in hyperdivergent patients with and without mouth breathing.
Materials and Methods: Lateral cephalograms of 30 patients with hyperdivergent facial patterns who reported for orthodontic
treatment were obtained and allotted to 2 groups based on the clinical history recorded with respect to nasal/mouth
breathing and cephalometric findings. The upper and lower pharyngeal airway widths were measured manually on the cephalograms
using the Mc Namara airway analysis.
Results: The upper airway width in hyperdivergent subjects with mouth breathing was greater compared to subjects who
had nasal breathing. However there was no statistically significant differences in lower pharyngeal widths in the two groups
(p<0.0625).
Conclusion: The upper airway width in hyperdivergent subjects with and without mouth breathing varied significantly
(p<0.047). Subjects with hyperdivergent growth patterns show a narrow upper pharyngeal airway space.
2.Case Report
3.Discussion
4.Conclusion
5.References
Keywords
Hyperdivergent; Mouth Breathing; Pharyngeal Space.
Abbreviations
UPA: Upper Pharyngeal Airway; LPA: Lower Pharyngeal Airway.
Background
Respiration is a metabolic process in which an organism's living
cells obtain energy (in the form of ATP) by inhaling oxygen and
exhaling carbon dioxide produced by the oxidation of complex
organic molecules [1]. The upper and lower respiratory airways
are structurally separated in the respiratory system [2]. Both the
nasopharynx and the oropharynx are parts of the unit that carries
out respiration [3].
A normal airway is crucial for the normal development of the
craniofacial tissues. Breathing through the nose acts as a filter of
the inspired air by extracting contaminants such as dust and bacteria
prior to air passing into the remaining respiratory system [2].
However, a large percentage of indivituals in the general population
have mouth breathing due to various etiologies including
enlarged tonsils, deviated nasal septum. On evaluation, these patients
have been found to have reduced airway volume.
Maintaining an oral airway is required to breathe through the
mouth, which is achieved by shifting the mandible and tongue
downward and backward, as well as tilting the head backward.
Obstruction of upper airway alters breathing, which can have a
substantial impact on craniofacial development, resulting in defects
in transverse maxillary growth, as well as cause downward
and backward growth of the mandible [4].
According to Harvold EP et al, increased convexity of face, increased
lower face height, narrow maxillary arch shape, deep palatal contour, gummy smile, Class II and Class III malocclusion are
all characteristic features that occur due to changes in the pattern
of craniofacial growth caused by upper airway obstruction, resulting
in mouth breathing [5].
Skeletal features such as retroposition of the upper and lower
jaws and vertical maxillary excess in hyperdivergent patients may
lead to narrow anteroposterior dimensions of the airway [6].
However, according to Tourne LP et al, variables that influence
dentofacial development and the onset of a malocclusion condition
include genetic, developmental, and environmental factors
[7].
McNamara airway analysis is a cephalometric analysis used to examine
the possibility of an airway impairment by measuring the
upper and lower pharyngeal width [8].
Adults of both sexes have an average upper airway measurement
of 15-20 millimeter. With age, this measure increases [8].
The average width of the lower pharyngeal space is 11 to 14 mm
and does not alter much with age [8].
An understanding of upper and lower pharyngeal airway is great
value and helps the clinician in diagnosis and planning of orthodontic
treatment objectives. This study aimed to compare the
pharyngeal space width in hyperdivergent patients with and without
mouth breathing.
Methods
Lateral cephalograms of 30 patients of age group 12 -35 years
who had reported to the Amrita School of Dentistry for orthodontic
treatment were obtained for each subject and allotted to
2 groups based on the clinical history recorded with respect to
nasal/mouth breathing and cephalometric findings.
The subjects were assigned into 2 groups
Group A- 15 patients with Mouth Breathing and Increased facial
height.
Group B- 15 patients without Mouth breathing and Increased facial
height.
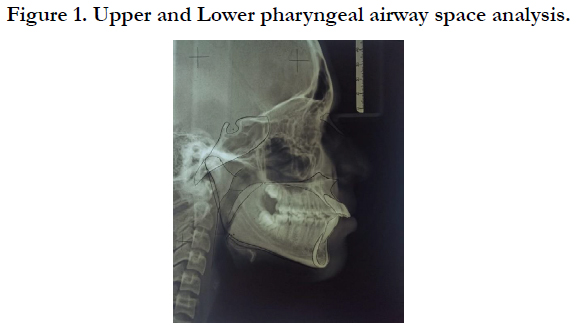
The upper and lower pharyngeal width in these patients were
measured on the cephalogram. The soft palate, the posterior border
of tongue, and the wall of posterior pharynx were all defined
(Fig 1)
To measure the upper pharyngeal width, the distance from posterior
nasal spine to the tip of the soft palate was bisected. The distance
between the soft palate's anterior region and the posterior
pharyngeal wall was measured. Measurements of less than 5 mm
is an indicator of possible airway impairment [8].
To measure the lower pharyngeal width, the point of intersection
between the tongue's posterior outline and the mandible's inferior
border (at the gonial angle) was identified. The distance between
this point and the posterior pharyngeal wall was calculated [8]. A
lower pharyngeal width of more than 15 mm indicates that the
tongue is positioned anteriorly, either as a result of habitual posture
or due to an enlarged tonsil [9].
SN-GoGn angle was used to identify the facial patterns3. An angle
of greater than 32 degrees was classified into hyperdivergent
facial pattern.
Statistical Details
To test the statistical significant difference in the mean pharyngeal
space width between hyperdivergent patients with and without
mouth breathing, independent sample t test, was applied.
Results and Discussions
Normal respiration relies heavily on adequate anatomical dimensions
of the airway. According to Linder Aronson S et al, the
development of the face and occlusion could be influenced by
respiratory function[10]. In recent years, studies have focused on
the variations in skeletal pattern that can predispose to airway obstruction
[3]. This study aimed to compare the width of the upper
and lower pharyngeal space in hyperdivergent patients with and
without mouth breathing.
According to Preston CB at al, in children of all ages, lateral skull
radiographs provide a good view of the nasopharyngeal airway
[11]. The measurements of the upper and lower pharyngeal
widths in our study was carried out on lateral cephalograms using
the Mc Namara airway analysis. This was similar to a study by Joseph
at al who also used lateral cepahlometric records to compare
the nasopharyngeal, oropharyngeal, and hypopharyngeal dimensions
of people with hyperdivergent and normodivergent facial
types [12]. This was also similar to a study carried out by Mirja et
al who used lateral cephalograms to study the upper airway structure
in Class II malocclusion children who underwent treatment with cervical headgear [13].
Linder Aronson also observed a strong link between posterior
rhinoscopy results and radiographic cephalometrics [10]. However,
according to Malkoc et al, because lateral cephalometric
radiographs only provide two-dimensional representation of the
nasopharynx, which is made up of complex three-dimensional
anatomic features, their relevance in evaluating the upper airway
is restricted [14]. In this study, we have evaluated only the pharyngeal
airway width and not airway volume.
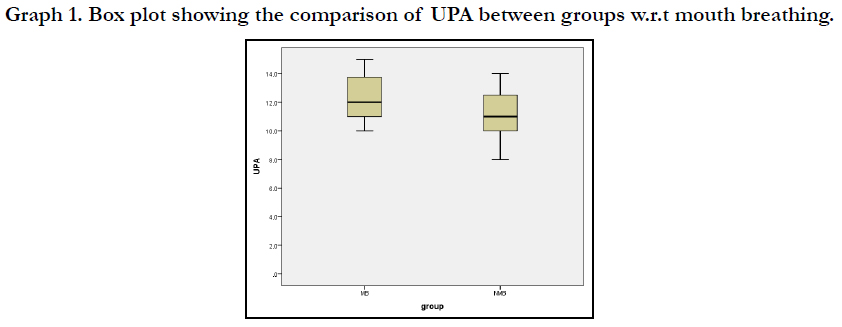
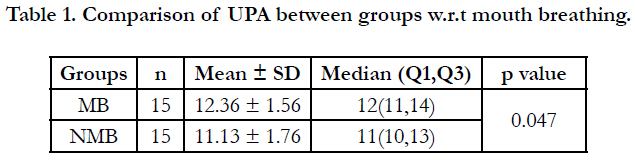
The results of this study showed that the median upper pharyngeal
airway (UPA) of the patients those who had mouth breathing
was 12 mm, (11 mm and 14 mm as the first and third quartile
respectively). The median upper pharyngeal airway (UPA) of the
patients without mouth breathing was 11 mm, (10 mm and 13
mm as the first and third quartile respectively). There was a statistically
significant difference in the median UPA of patients with
and without mouth breathing (p<0.047) (Table 1).
The upper pharyngeal airway in subjects with mouth breathing
was greater compared to subjects without mouth breathing which
may be attributed to the varying age groups of subjects included
in the study. However, these hyperdivergent subjects showed a
small upper airway space. This is consistent with the findings of
Mani et al, who observed a small width of the upper pharyngeal
airway in hyperdivergent facial pattern patients which was statistically
significant.[3]
Box plot graphs showing the comparison of UPA between groups
with respect to mouth breathing showed a positively skewed distribution.(
Graph 1). Lines in the boxes denote the median value
with the lower whisker demonstrating the first quartile and the
upper whisker demonstrating the third quartile.
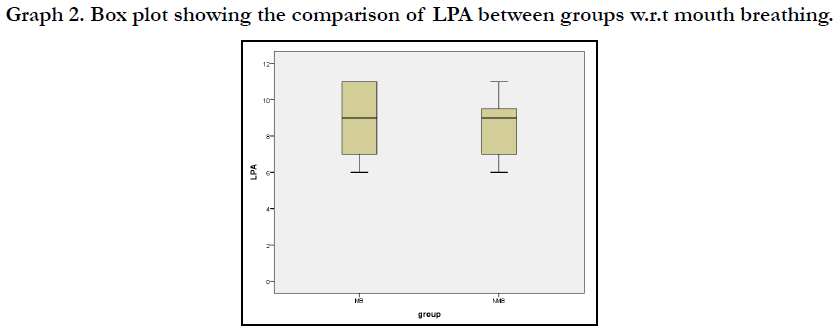
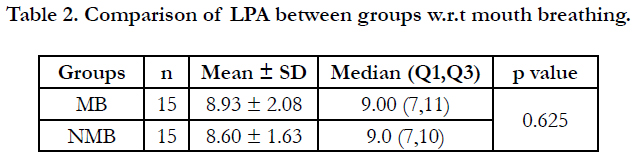
The median lower pharyngeal airway (LPA) of the patients those
who had mouth breathing was 9 mm, (7 mm and 11 mm as the
first and third quartile respectively). The median lower pharyngeal
airway (LPA) of the patients without mouth breathing was 9 mm,
(7 mm and 10 mm as the first and third quartile respectively).
The comparison of the median LPA in patients between the two
groups was found to be not statistically significant (p<0.625) (Table
2). When compared to other facial types, hyperdivergent facial types
have a small maxillary area.
On the contrary, de Freitas et al mentioned that upper pharyngeal
airway width is not influenced by malocclusion type, and lower
pharyngeal airway width is unaffected by malocclusion type and
growth pattern [15].
Orthodontists should evaluate pharyngeal airway morphologies
while evaluating and treating preadolescent children with malocclusion
because they may be a risk factor for undesired craniofacial
development. This can help provide better stability of
treatment results. Future studies should include a long term examination
of craniofacial morphology with a larger sample size
and patients with sagittal Class I, Class II, and Class III and vertical
facial growth patterns must be examined.
Conclusion
? The upper airway width in hyperdivergent subjects with and
without mouth breathing varied significantly.
? Subjects with hyperdivergent growth patterns show a narrow
upper pharyngeal airway space.
? There was no statistically significant differences in lower pharyngeal
width in hyperdivergent subjects in the two groups.
Authors' contributions: The work presented here was carried
out in collaboration with all the authors. Anu Rose James carried
out the analysis, performed the literature review, interpreted
the results, and wrote the manuscript. Ajith V.V was the chief
supervisor of the study and provided guidance in every phase of
the study and the writing of the manuscript. Sapna Varma N.K:
provided approval of final study design and critical review of the
article.All authors read and approved the final manuscript.
Acknowledgements
I would like to express my gratitude to my guide and mentors for
helping me in performing the study and better understanding of
the subject. I/We confirm that we have no financial ties to any
commercial entity and we are having a direct financial interest in
the subject or materials addressed in this work. Any additional
possible conflict of interest is disclosed.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of the
Amrita Institute of Medical Sciences, Kochi (IRB No: 2019/147).
References
-
[1]. Mortola JP. How to breathe? Respiratory mechanics and breathing pattern.
RespirPhysiolNeurobiol. 2019 Mar;261:48-54. PubMed PMID: 30605732.
[2]. Woodson BT. A method to describe the pharyngeal airway. Laryngoscope. 2015 May;125(5):1233-8. PubMed PMID: 25346200.
[3]. Mani P, Muthukumar K, Krishnan P, Senthil Kumar KP. Upper and lower pharyngeal airway space in West-Tamil Nadu population. J Pharm Bioallied Sci. 2015 Aug;7(Suppl 2):S539-42. PubMed PMID: 26538913.
[4]. Yamada T, Tanne K, Miyamoto K, Yamauchi K. Influences of nasal respiratory obstruction on craniofacial growth in young Macacafuscata monkeys. Am J OrthodDentofacialOrthop. 1997 Jan;111(1):38-43. PubMed PMID: 9009922.
[5]. Harvold EP, Tomer BS, Vargervik K, Chierici G. Primate experiments on oral respiration. Am J Orthod. 1981 Apr;79(4):359-72. PubMed PMID: 6939331.
[6]. Roy AS, Tandon P, Chandna AK, Sharma VP, Nagar A, Singh GP. Jaw morphology and vertical facial types: a cephalometric appraisal. J Orofac Res. 2012:131-8.
[7]. Tourne LP, Schweiger J. Immediate postural responses to total nasal obstruction. Am J OrthodDentofacialOrthop. 1996 Dec;110(6):606-11. PubMed PMID: 8972806.
[8]. McNamara JA Jr. A method of cephalometric evaluation.Am J Orthod. 1984 Dec;86(6):449-69. PubMed PMID: 6594933.
[9]. McNamara JA. Influence of respiratory pattern on craniofacial growth. Angle Orthod. 1981 Oct;51(4):269-300. PubMed PMID: 6947703.
[10]. Linder-Aronson S, Leighton BC. A longitudinal study of the development of the posterior nasopharyngeal wall between 3 and 16 years of age.Eur J Orthod. 1983 Feb;5(1):47-58. PubMed PMID: 6572594.
[11]. Preston CB, Goldberg J, Grist D. Facial profile reproduction in lateral cephalometric radiographs. J Dent Assoc S Afr. 1979 Oct;34(10):571-4. PubMed PMID: 298383.
[12]. Joseph AA, Elbaum J, Cisneros GJ, Eisig SB. A cephalometric comparative study of the soft tissue airway dimensions in persons with hyperdivergent and normodivergent facial patterns. J Oral Maxillofac Surg. 1998 Feb;56(2):135-9. PubMed PMID: 9461134.
[13]. Kirjavainen M, Kirjavainen T. Upper airway dimensions in Class II malocclusion. Effects of headgear treatment.Angle Orthod. 2007 Nov;77(6):1046- 53. PubMed PMID: 18004913.
[14]. Malkoc S, Usumez S, Nur M, Donaghy CE. Reproducibility of airway dimensions and tongue and hyoid positions on lateral cephalograms.Am J OrthodDentofacialOrthop. 2005 Oct;128(4):513-6. PubMed PMID: 16214635.
[15]. de Freitas MR, Alcazar NM, Janson G, de Freitas KM, Henriques JF. Upper and lower pharyngeal airways in subjects with Class I and Class II malocclusions and different growth patterns.Am J OrthodDentofacialOrthop. 2006 Dec;130(6):742-5. PubMed PMID: 17169736.